1
Diuretics
Dr.Nasser A. H. Al-Harchan
Diuretics:
These are drugs that increase renal excretion of Na
+
(solutes) and
water, Diuresis as an act is initiated by renal and extra-renal mechanisms.
Extra renal mechanisms that increase excretion of urine are:
1. CO (cardiac output), this lead to increase in glomerular filtration rate and
then increase the excretion of urine as digoxin used in heart failure.
2. Inhibition in ADH release by either water or hypotonic solutions.
3. Mobilizing peripheral edema fluid like the use of albumin in
hypoproteinemic cases.
Renal mechanisms:
Glomerular filtration in 24 hrs. will be 180 L/day, while the volume of urine
is 1liter, so the rest is reabsorbed by the renal tubules.
The major effect of these drugs is to inhibit the reabsorption of Na
+
by renal
tubules so that to increase the Na
+
excretion which are accompanied with
water so as to keep the osmotic balance of the body.
Notes:-
H+ ion help in the reabsorption of Na
+
, HC03 and help in ammonium ion
excretion.
H+ & K+ can exchange with Na
+
and substitute for each other also.
2
3.
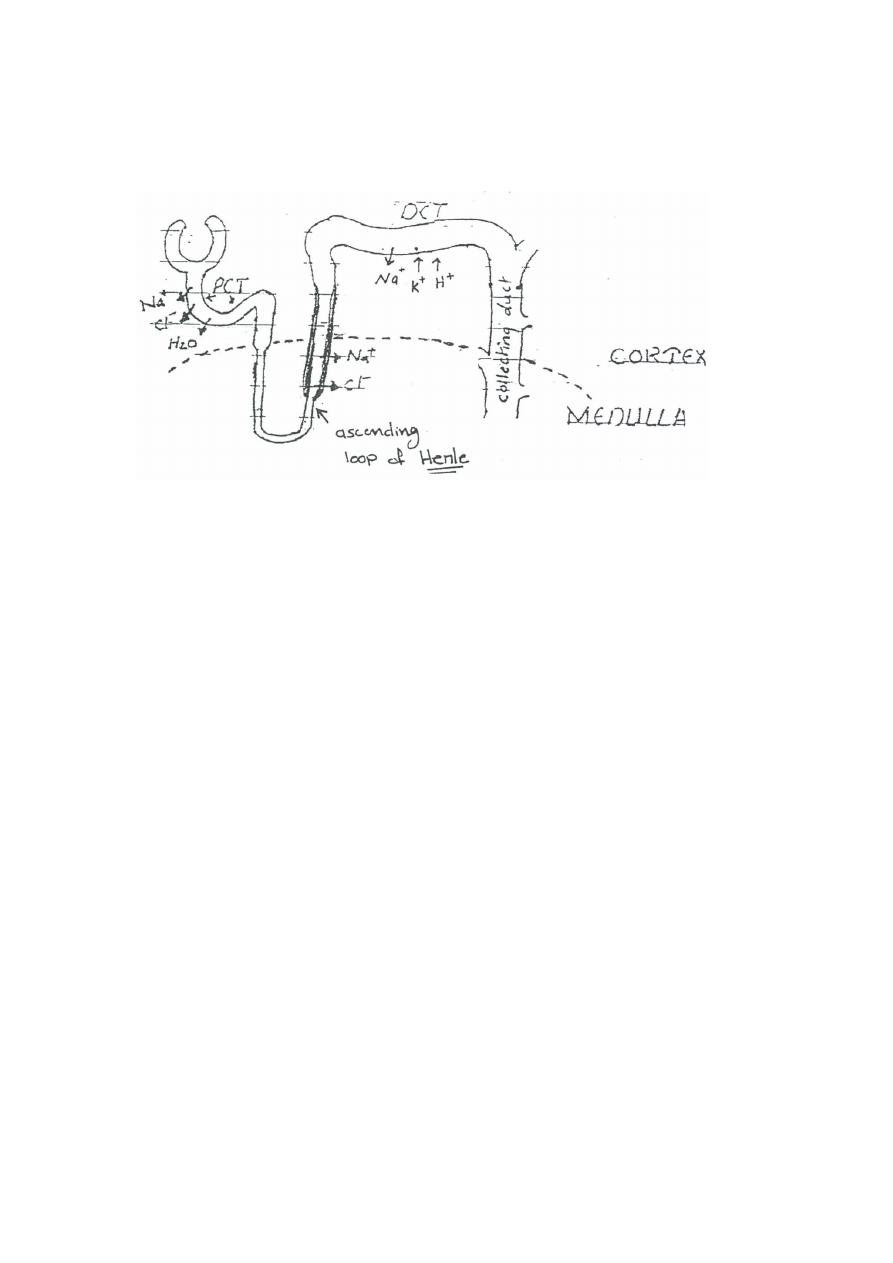
Distal convoluted tubules (DCT): Na+ is actively reabsorbed in
exchange with K+ & H+ under aldosterone influence, this part is
responsible for 5% of filtered Na+ reabsorption and it's the site of action
of ADH.
4.
Collecting duct: is the site of ADH because in the presence of ADH
this part is permeable to water and urine (becomes hypertonic
"hyperosmolar" because it contains a large amount of electrolytes and
vice versa). And if no ADH the urine becomes hypotonic.
Division of Nephrons:
1. Proximal convoluted tubule (PCT): 60 - 70 % of the filtered Na, Cl
-
, H
2
O are
reabsorbed actively in such rapidity that osmotic balance is kept below
intraluminal & interstitial fluid.
2. Ascending loop of Henley: in this part there is active reabsorption of Cl
-
followed by Na
+
and no water reabsorption in this part so it's known also as
diluting segment, 20-30 % of filtered Na
+,
Cl
-
is reabsorbed here.

3
Groups of Diuretics:
1.
High Efficacy Diuretics (HED) "Loop diuretics II"
2.
Moderate Efficacy Diuretics (MED)
3.
Low Efficacy Diuretics (LED)
High Efficacy Diuretics (HED):
•
It's also called high ceiling diuretics or loop D. & they are:
Furosemide* or you can write it as frusemide and (it's the most popular
one & the most effective one), Ethacrynic a. , Bumetanide, Piretanide &
torasemide .
•
HED can cause 5-25 % of filtered Na+ to be excreted.
•
They are called Loop D. due to their action on the medullary part
of ascending Loop of Henley, also slight effect on proximal CT.
Notes:
•
HED can work even if the GFR is below 10 ml/min; a case of
Oliguria (normal GFR is 120 ml/min.).
•
Anuria is a contraindication of this group.
•
They are chemically different but although have similar properties
& indications, they vary in their efficacy “i.e. maximum diuresis they
produce”
•
Frusemide - Bumetanide 1 Etharcrynic a. is less than both. *Lasix
(marketing name)

4
Mechanism of action:
HED act by inhibiting Cl
-
& Na
+
reabsorption load to excretion of both Cl
-
& Na
+
in urine which is usually accompanied by water and large amount of urine, K is
also excreted lead to hypokalemia because of large amount of Na is subjected to
the distal t. where it has more chance to be exchanged with K there.
This loss of K+ may be corrected by either k supplement or using of LED (K
sparing diuretics) that retains K
+
to body.
NOTE: the onset of action of HED is within 2-10 min if given W & 1 hr. if given
orally.
Indications:
1. Acute pulmonary edema but the relief occurs before diuresis so this is a hint
of their effect on B.V.
2. Hypertensive crisis.
3. All cases of heart failure particularly refractory hear failure "which are not
responsible to other drugs "
4. Chronic renal failure.
5. Refractory edema.
6. Nephrotic syndrome.
7. Oligouric state {urine volume } to protect from acute renal failure but
shouldn't be used in Anuria.
8. Promote Ca
++
excretion but not to a state of hypocalcaemia, but in some
cases of hypercalceamia it's used with saline.
9. Forced alkaline diuresis to get rid of some drugs from the body “like
salicylate and barbiturates ".
5
7.
GI disturbances with or without bleeding. If it's given to patient
with ascites "free fluid in peritoneal cavity" leads to hepatic coma and
probably hepatorenal syndrome because of liver cell necrosis.
8.
Hypomagnesaemia" Mg++ Depletion".
9.
Hypotension.
10.
Skin rush and parasthesia "abnormal sensation in hand and feet
nn.".
Routes of administration:
•
Furosemide and Bumetanide taken orally, IM & IV routes.
•
Ethacrynic a. taken orally and IV only.
ü
HED can inhibit 15-20% of filtered load.
Side effects and clinical toxicity:
1. Metabolic alkalosis might result as CI
-
loss is relatively excreted more than
HCO
3
.
2. Hyperuricemia ( uric acid in blood) because of that high efficacy diuretics
and uric a. have the same secretory mechanism on tubules.
3. Decrease CHO tolerance (diabetics and prediabetics, sugar level may be
increased) occur with less extent than thiazides.
4. Hypokalemia & corrected as mentioned before in the mechanisms of
action.(this hypokalemia is less serious than that produced by MED because
of their short duration of action in comparison with MED).
5. Might cause renal interstitial nephritis lead to reversible renal failure.
6. Deafness may be:
Transient with Furosemide.
Infrequent with Bumetanide.
Permanent with Ethacrynic a.
6
Moderate Efficacy Diuretics {MED}:
They are:
Thiazide, chlorthiazide I hydrochlorthiazide I hydroflumethiazide I
cyclopenthiazide, Bendrothiazide.
Drugs related to thiazides:
Chlorthalidone, quinethazone, metolazone "used in renal problems", clopamide,
mefruzide, indapamide, teinilic a. "related to ethacrynic a. but moderate with
uricosuric effect" i.e. uric acid secretion in urine.
MEO are represented by thiazide group, they inhibit 5 -10 % of
filtrated load of Na
+,
they won't work if GFR is below (20 ml/min)
Their site of action is at cortical diluting segment cortex part loop of
Henley ( some books say happens in OCT)
They have qualitatively similar properties but they differ quantitively
and this is reflected in the doses used and their potency.
Mechanism of action:
related to
1. Carbonic anhydrase inhibitory effect, the more the drug is potent the less the
contribution of the effect is.
2. Direct inhibition of Na reabsorption, followed by Cl
-
reabsorption so water
excreted with K
+
as in HEO.
They have some anti-hypertensive action partly due to volume of urine lost
lead to decreased CO and partly due to an effect on blood vessels because a
non - diuretic thiazide which is diazoxide act as an antihypertensive agent.
Uses:
1. Chronic renal failure.
2. Edema due to chronic hepatic disease but if there is hypokalemia, may
worsen or ppt. encephalopathy.
3. Hypertension, either used alone or with antihypertensive agent.
4. hypocalceuria : because they reduce excretion of Ca
++
so it might be used in
colic related to idiopathic hypercalceurea.
5. nephrogenic diabetes insipidus, they volume of urine "differ in action" they
produce hyperosmolar urine or can substitute AHD, they may reduce volume
of urine from 12L 3L

7
Side effects:
1. Hypokalemia more serious than HED and treated by the same way.
2. Hyperuricemia like HED with gout attacks.
3. D.M. aggravation I such patients have CHO tolerance I increase in glucose
in blood I they do so by either inhibiting insulin secretion or inhibit glucose
peripheral utilization.
4. hypercalceamia
5. Hyperlipidemia.
6. Thrombocytopenic purpura.
