Pharmacology
Adrenal steroidsDr. Ahmad Al-Zohyri
Lec. 10Total Lectures No. 23
Adrenal steroids (corticosteroids & corticotrophins)They are hormones produced by the adrenal cortex, they include: hydrocortisone (cortisol), estrogens, corticosterone, some androgens & estrogens but not cortisone (prodrug).
Corticosteroids are usually given for 1 of 3 reasons:
Suppression of inflammation.
Replacement therapy (failure of adrenal cortex ill case of Addison's disease).
Suppression of immune response.
They are hormones normally synthesized from cholesterol by adrenal cortex & have a wide range of pharmacological functions.
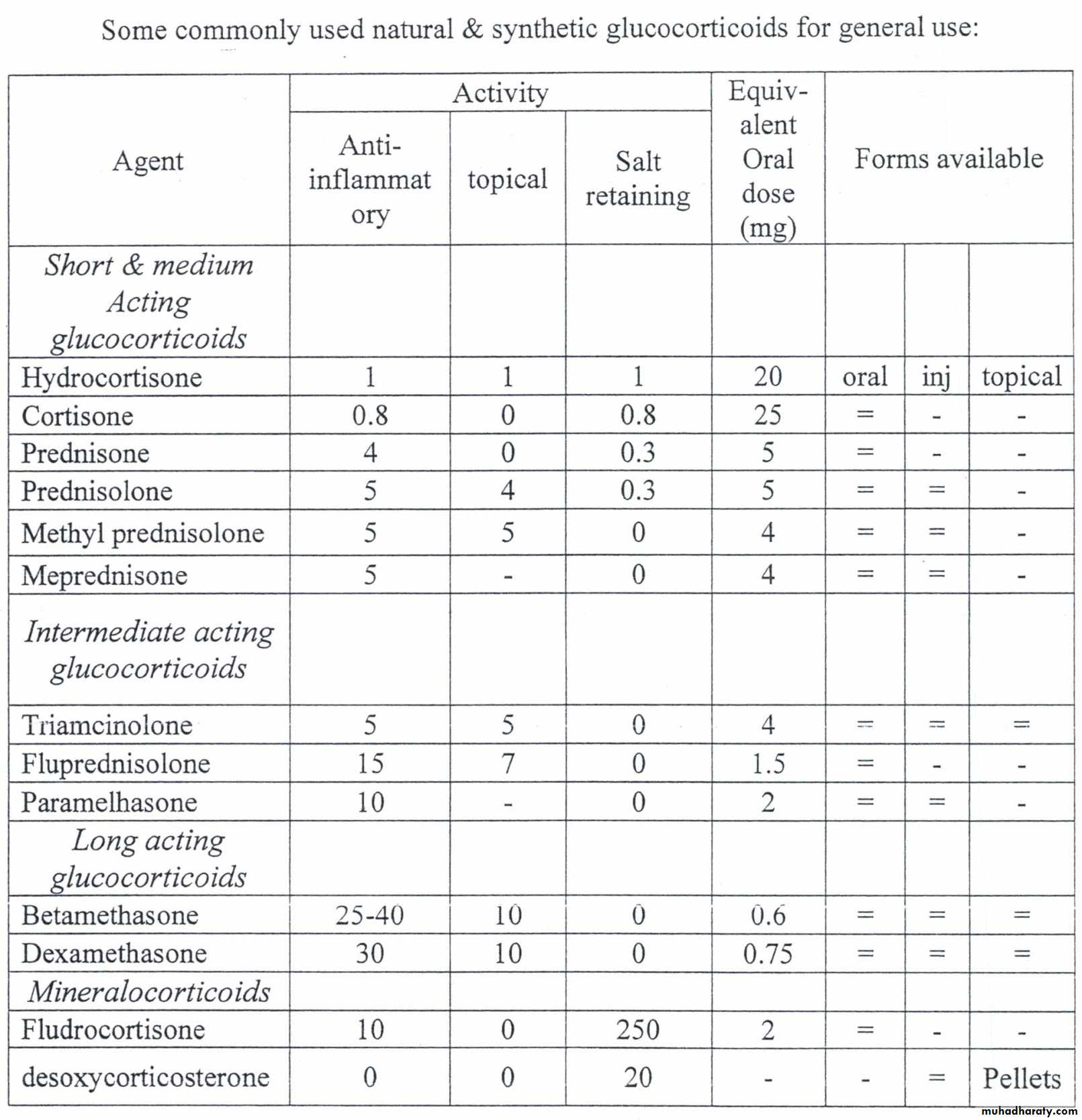
Pharmacologically; they are divided according to the relative potencies of their physiological effects into:-
Glucocorticoids that principally affect CHO & protein metabolism.
Mineralocorticoids that principally affect Na+ balance.
Synthetic steroids have largely replaced the natural compounds in therapeutic use as they are usually more potent, may be more specific with regard to mineralocorticoid & glucocorticoid activity & can be given orally. Prednisolone, betamethasone & dexamethasone are widely used as anti-inflammatory & immunosuppressant drugs.
Mechanism of action (general)
Adrenal steroids enter the cell & combine with the steroid receptors of the cytoplasm.The combination enters the nucleus & controls protein synthesis; this includes enzymes regulating cell functions such as inflammation.
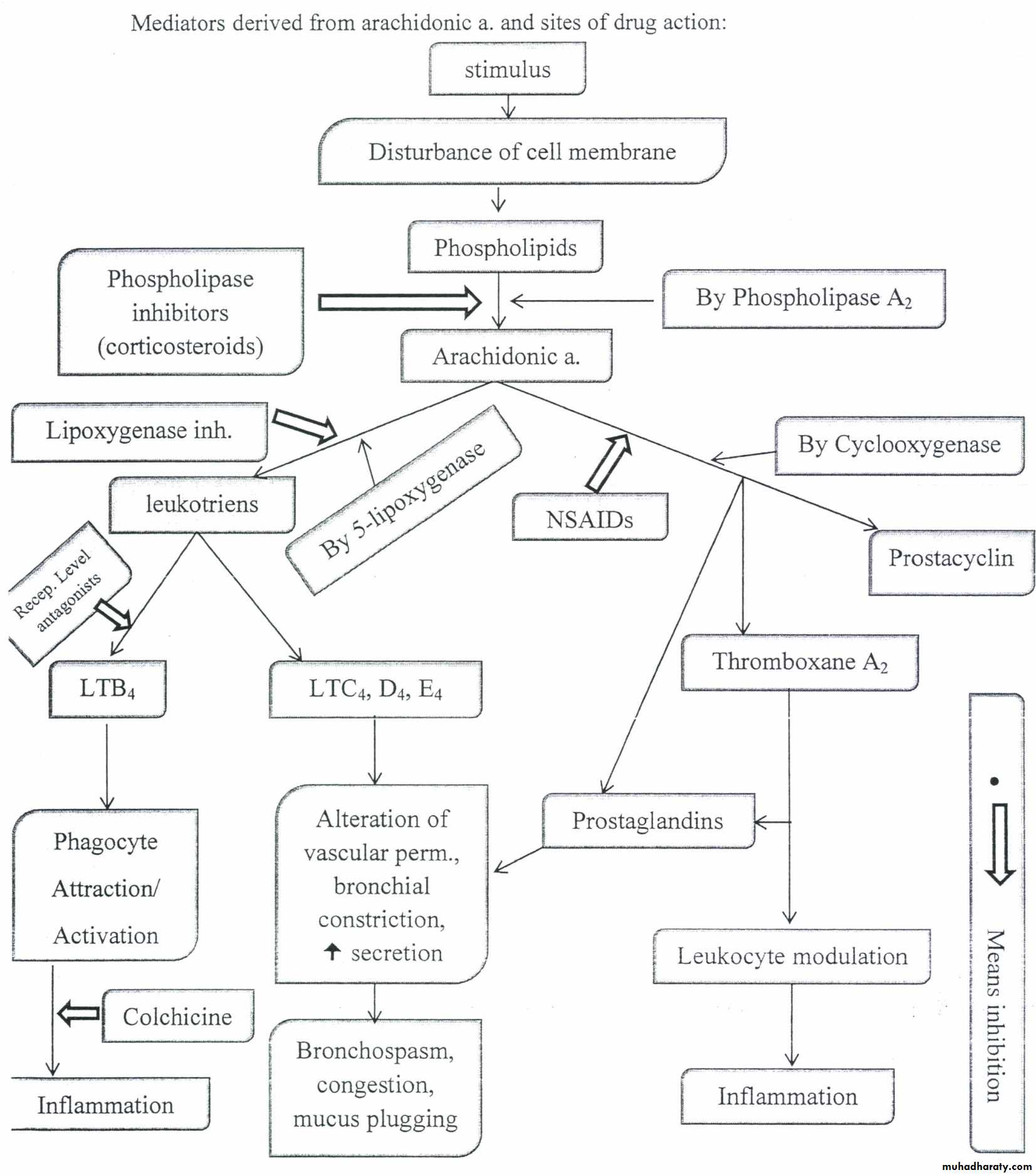
Inhibition of inflammation achieved through the formation of a protein (lipocortin) that inhibits the enzyme phospholipase A2 (it's activity) which is needed to allow the supply of mediators essential for the inflammatory process.
Corticosteroids also act on cell membranes altering ion permeability & modify production of neurohormones.
Glucocorticoids (cortisol & its derivatives)
Pharmacological effects:
On inflammatory responses: irrespective of the injury or the insult, corticosteroids interfere non-specifically with all components of the inflammatory response. This includes:
Reduce capillary dilation & exudation.
Inhibition of leukocyte migration & phagocytic activity.
Reduce fibrin deposition of scar formation.
Suppression of reparative processes & functions of fibroblasts.
Lysosomal stabilization.
Prevention of the release of arachidonic acid from phospholipids.
2) On immunological response: in high doses:
Lymphocyte mass & immunoglobulin production are reduced.
Reduce monocyte & macrophage function.
These will lead to impaired immunological competence.
3) On CHO & protein metabolism: steroids promote:
Glycogen deposition in the liver & gluconeogenesis, an increase in glucose output by the liver & decrease in glucose utilization by peripheral tissues,
An increase in protein catabolism with mobilization of amino acids from peripheral tissues.
4) On fluid & electrolyte balance: even glucocorticoids have some mineralocorticoid activity. The principle effects are:
Enhanced Na reabsorption from the distal tubules of the kidney.
An associate increase in urinary excretion of K+ and hydrogen ions.
Edema is rare but moderate hypertension is not uncommon.
5) On lipid metabolism: Corticosteroids facilitate fat mobilization & redistribution of body fat to "centripetal" areas: face, neck & shoulders.
6) On mood & behavior: mild euphoria is quite common with higher doses.
7) Other effects:
Increase in number of RBCs, platelets & polymorphs but decrease in number of eosinophil & lymphocytes.
Reduction of bone formation.
Increased production of gastric acid and pepsin.
Adverse effects:
Metabolic effects: Patients on high dose steroid therapy quickly develop a characteristic appearance: a rounded face (moon face), deposition of fat over the supraclavicular and cervical areas (buffalo hump), obesity of the trunk with relative thin limbs, purple stria on the thighs & lower abdomen, a tendency to bruising.
Disturbed CHO metabolism leads to hyperglycemia and glucosuria. In addition to the loss of protein from skeletal m. patients develop muscular weakness (thighs & upper arms),
Fluid retention: This may be associated with hypokalemic alkalosis & hypertension.
Increase Susceptibility to infection.
Osteoporosis, which may cause compression fractures of the vertebral bodies and a vascular necrosis of the head of the femur.
Psychosis: a sense of euphoria frequently accompanies high dosage steroid therapy & this may rarely proceed to overt manic psychosis.
The increased sense of well-being may lead to an improved appetite & contribute to wt. gain.
Cataract: a rare complication, usually in children, reflecting prolonged high dose therapy.
GI symptoms: dyspepsia frequently accompanies high dose oral steroid therapy. There is increased incidence of peptic ulceration & upper GIT bleeding. Signs of peritonitis which would complicate a perforated peptic ulcer may be masked by the anti-inflammatory effect of steroids.
Metabolism:
Glucocorticoids absorbed rapidly & completely from the GIT. The max. plasma cone. Reached within 1-2hrs. Hepatic degradation leaves 25% of the max. after 8 H. & the active drug disappear within 12hrs..
Drugs that promote microsomal enzymes accelerate steroid metabolism (i.e. phenobarbital, phenytoin), so the dose of steroids should be increased in this case.
Tropical therapy:
Topically applied steroids are absorbed through the skin & in case of very potent drugs such as clobetasol or betamethasone adrenal suppression & other toxic effects can occur. This usually happens with high doses on extensive areas for long time.
Other effects:
Worsening of local infections.
Local thinning of the skin.
Increased hair growth.
With the use ofbeclomethasone aerosol can result in candidiasis of the mouth.
Clinical use & dose:
Hydrocortisone: used in three different situations:
Replacement therapy, when it is given orally in a dose of20 mg in the morning & l0 mg in the evening.
Shock & status asthmatic us, when it is given IIV up to 500 mg 6 hourly.
Topical application: e.g. 1 % cream or ointment in eczema; 100 mg doses as enemata or foam in treating ulcerative colitis.
Prednisolone: Used orally in three types of conditions:
Inflammatory disease; e.g. severe rheumatoid arthritis, ulcerative colitis, chronic active hepatitis.
Allergic diseases; e.g. severe asthma, minimal change glomerulonephritis.
Acute lymphoblastic leukemia & non-Hodgkin lymphoma.
It would be usual to start at 20 mg 8 hourly& reduce the dose according to clinical improvement.
Used topically in ulcerative colitis as 20 mg enema.
Prednisone: this is usually metabolized to prednisolone.
Beclomethasone: A fluronated & therefore non-polar steroid which passes across membranes.
It is used topically in:
Asthma when it is given by metered aerosol doses each of 50 µg. Usual daily dose is. 100 µg 6-8 hourly. About 20% of this reaches the lungs; the rest is swallowed and destroyed by 1st pass metabolism.
Severe eczema, when it is used 0.025% cream.
Betamethasone: used for:
Cerebral edema caused by tumors & trauma, given either orally or I/M in a doses of up to 4 mg 6 hourly.
Severe eczema given topically as 0.1 % cream.
Dexamethasone: is used in cerebral edema.
Triamcinalone: used in:
Local inflammation of joints or soft tissue given by intra-articular injection in doses up to 40 mg depending on joint size.
Severe eczema given topically as 0.1 % cream.
Clobetasal: used topically in severe resistant eczema & discoid lupus erythematosus.
Mech. Of anti-inflammatory & immunosuppressive action of glucocorticoids:
Glucocorticoids have the capacity to reduce the manifestations of inflammation due to their profound effect on:
i) Cone.
ii) Dist. Of peripheral WBCs + inhibition of
iii) Function phospholipase A2
After a single dose of a short acting glucocorticoid:
The cone. Of neutrophil increased.
Lymphocytes (T & B), monocytes, eosinophil & basophils decrease in number.
This change max. at 6 hours and fade away after 24 hours.
The increase neutrophil is due to: increase influx from bone marrow and decrease migration from blood vessels leading to reduction in number of cells at site of inflammation.
The reduction in circulating lymphocytes, monocytes, eosinophil & basophils is the result of their movement from vascular bed to lymphoid tissue.
Glucocorticoids inhibit the function of WBCs & tissue macrophages.
The ability of these cells to respond to antigens is reduced.
The effect on macrophages is marked, it limits their phagocytic ability on microorganisms & to produce enzymes (i.e. collagenase, elastase, ... etc.).
Large doses stabilize laysosomal membranes, so reducing the cone. of proteolytic enzymes at site of inflammation.
In addition to their effects on WBCs function, they influence the anti-inflammatory response by inhibiting phospholipase A2.
They also cause vasoconstriction when directly applied to vessels, they decrease cap. permeability by inhibiting kinins & bacterial endotoxins & by reducing the amount of histamine released by basophils.
The anti-immune effect of glucocorticoids is largely due to the effect described above.
Antibody production reduced by large doses (not moderate or small doses).
Use of steroid in control of homograft rejection is augmented by their ability to reduce Ag release from grafted tissue, delay vascularization & interfere with the sensitization of Ab-forming cells.
The anti-inflammatory & immune suppressive effects are responsible for some of glucocorticoid serious effects.
Indications:-
Diagnosis & treatment of disturbed adrenal function: chronic Addison's disease ( adrenocortical insufficiency).
Adrenocortical hyperfunction:
Congenital adrenal hyperplasia.
Cushing syndrome.
Hyperaldosteronism.
Diagnostic purpose; to suppress ACTH to identify the source of particular hormone whether its production affected by ACTH.
Used to stimulate lung maturation in the fetus (if mother taking large doses of steroids, this delay lung maturation because it is under the influence of glucocorticoids ).
Therapeutic indications in non-adrenal disorders:
Allergic disorders, arthritis, cerebral edema, collagen disorders, eye dis., OIT dis., hemolytic disorder, hypercalcemia, immunosuppression, infection, neurological disorder, pulmonary dis., renal dis. ... etc.
Contraindications of adrenal steroids:
To be used with caution in patients with peptic ulcer, heart disease, hypertension with congestive heart failure, infections, psychosis, diabetes, osteoporosis, glaucoma, etc.
Mineralocorticoids:
(Aldosterone, desoxycorticosterone, flurocortisone)
Aldosterone is the most important in humans, also small amounts of desoxycorticosterone are formed and released, its action, effects & metabolism are similar to that of aldosterone.
Flurocortisone, a synthetic corticosteroid, the most commonly used salt-retaining hormone.
Aldosterone:
Its secretion is influenced by many factors. ACTH produces a moderate stimulation of its release (the effect lasts for few days).
It is 1/3 of cortisol effect is suppressing ACTH, the small amounts of it prevent it from taking part in any feedback relation in control of ACTH secretion.
An important stimulus for aldosterone secretion is reduction in blood volume whether due to hemorrhage, dietary Na restriction or Na loss following diuretic administration.
Physiologic & pharmacologic effects:
Induce Na reabsorption from urine by the distal renal tubules.
Na reabsorption in sweat, salivary gland, GI mucosa & across cell membranes increase by aldosterone.
High levels of aldosterone produced by tumors or over dosage with mineralocorticoids cause hypematremia, hypokalemia, metabolic alkalosis, increase plasma volume & hypertension.
Metabolism:
- Secreted at rate of 100-200 µg/day (normal individuals with moderate, dietary salt intake).
- T1/2 when injected in trace quantities is 15-20 min
- Metabolism, similar to cortisol.
- About 50 µg/24 hours appearing in urine (conjugated).
- 5 -15 µg/24 hours excreted free or glucoronoid.
Desoxycorticosterone:
- Precursor for aldosterone, secreted in amounts of 200 µg/day.
- T 112 when injected in human circulation is 70 min.
- Cone. In plasma about 0.03 µg/dl
- Secretion under control of ACTH.
- Secretion enhanced by dietary Na restriction.
Fludrocortisone:
- A potent glucocorticoid & mineralocorticoid & most widely used mineralocorticoid.
- Doses of 0.1 mg 2-7 times weekly have potent salt-retaining activity.
- Used in treatment of adrenocortical insufficiency but are too small to have anti-inflammatory effects.
Clinical use and dose:
Fludrocortisone is a fluorinated hydrocortisone with powerful mineralocorticoid activity & very little anti-inflammatory action.
It is used in:
Replacement therapy in doses of 50-200 µg/day
Congenital adrenal hyperplasia in doses up to 2 mg / day.
Idiopathic postural hypertension 100-200 µg each day
ACTH (adrenocorticotrophic hormone)
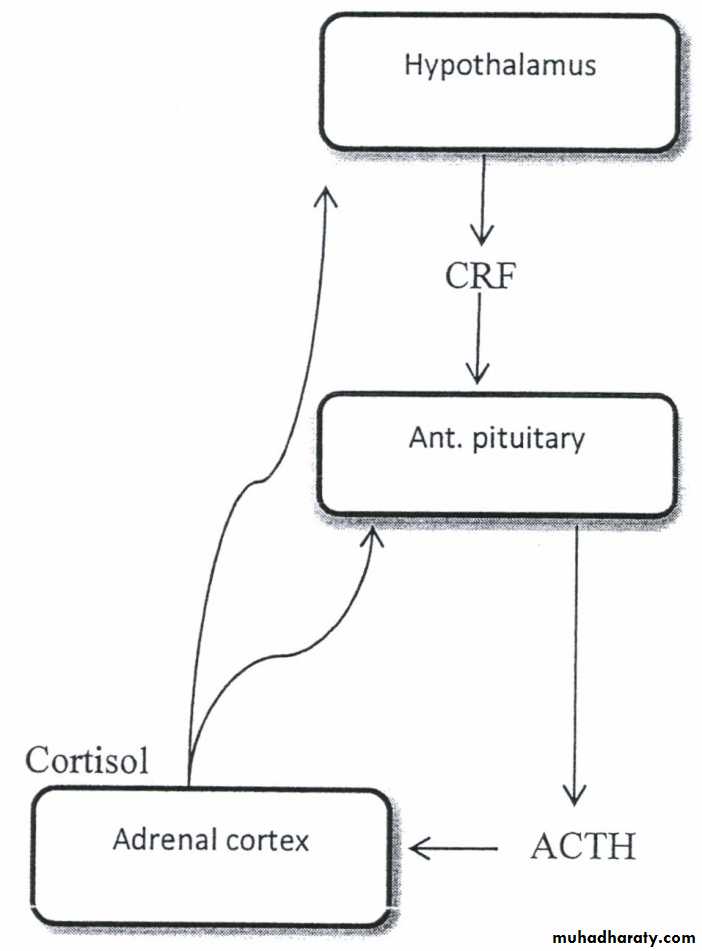
Corticotrophin is a polypeptide secreted by the anterior pituitary gland; its production by the pituitary gland responds rapidly to physiological requirements by the familiar -ve feedback mechanism.Its t1/2 is 10 min. the adrenal cortex responds rapidly (within 2 min.)
Actions:
Stimulate the synthesis of corticosteroids from the cells of adrenal cortex.
It has a transient effect on aldosterone production.
Regulation of corticotrophin release determined largely by the influence of cortisol level on CRF production through a -ve feedback mech.
Effect of corticotrophin on adrenal cortex is mediated by cAMP.
Preparations: Corticotrophin available for I/V & I/M administration. I/V injection rapidly destroyed in mins. So IN infusion or IM/ repository are better to use.
Uses:
Diagnostic: as a test of the capacity of the adrenal cortex to produce cortisol (measuring plasma concentration of cortisol after an IM injection of tetracosactrinTherapeutic: is seldom appropriate, but may be used in severe chronic rheumatic disease.
Principles in adrenal steroid therapy:
Steroids are powerful drugs; dramatic improvement in certain severe diseases is matched by equally dramatic ill health due to adverse effects when these drugs are used in mild inflammatory disorders for which they are not indicated.
Steroids; therefore, should be used only when other less toxic drugs have failed, or when the severity of the condition justifies aggressive treatment with steroids in high doses.
Once control of the clinical state has been achieved, steroid dose should be reduced to the min. necessary to maintain the desired effect & if possible stopped all together.