
Nutritional diseases
Nutrition and Nutrients
Nutrients
are substances that must be supplied by
the diet because they are not synthesized in the body in
sufficient amounts.
The need is depend :
Age
physiological state

Nutrition and Nutrients
macronutrients
Carbohydrates
Fats
Proteins
micronutrients
Vitamins
Minerals
Water

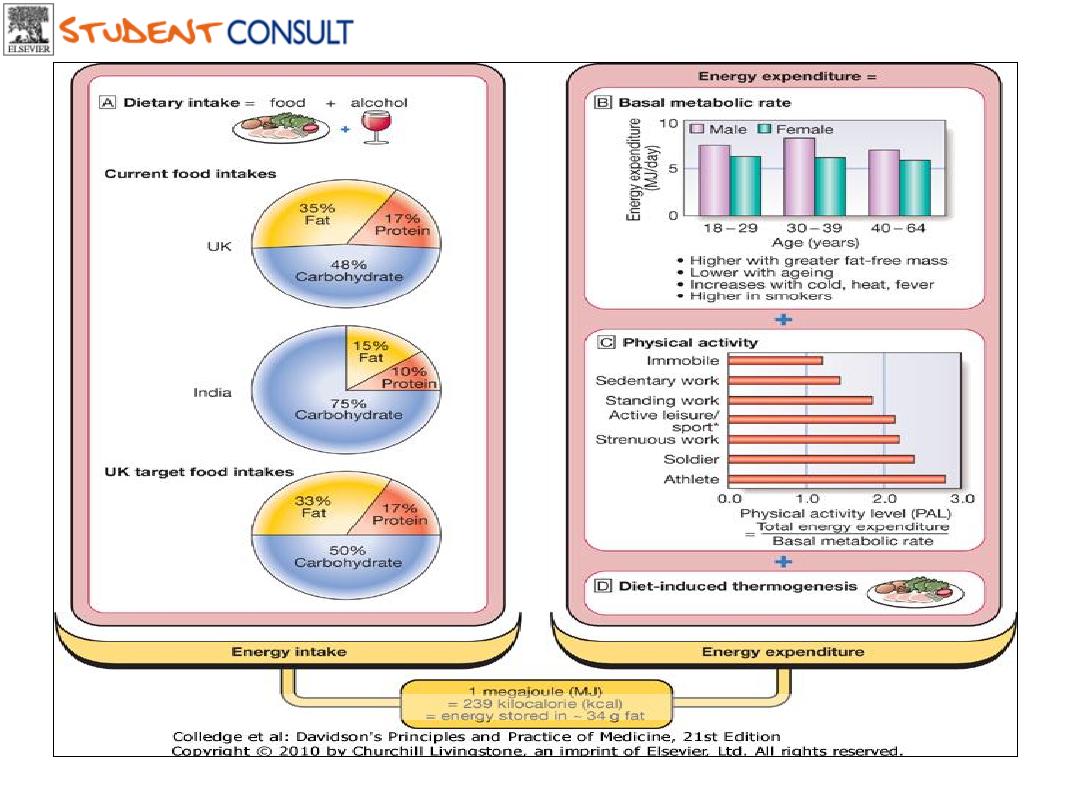
The energy balance
The
energy intake
equal to
energy output
The major components of energy output are:
1. resting energy expenditure (
REE
) (
BMR
) (60%)
depend on FFM (total body mass- fat mass)
2. physical activity (30%)
3. Diet induced thermo-genesis (10%)
Downloaded from: StudentConsult (on 17 October 2011 08:27 PM)
© 2005 Elsevier

The energy balance
Energy intake depend on macronutrient content
Different energy densities:
carbohydrates
(4 kcal/g),
fat
(9
kcal/g) and
protein
(4 kcal/g).
The average energy intake is about
2800
kcal/d (2000-3500)
for men and about
1800
kcal/d(1600-2250)for women
.
Downloaded from: StudentConsult (on 17 October 2011 08:27 PM)
© 2005 Elsevier
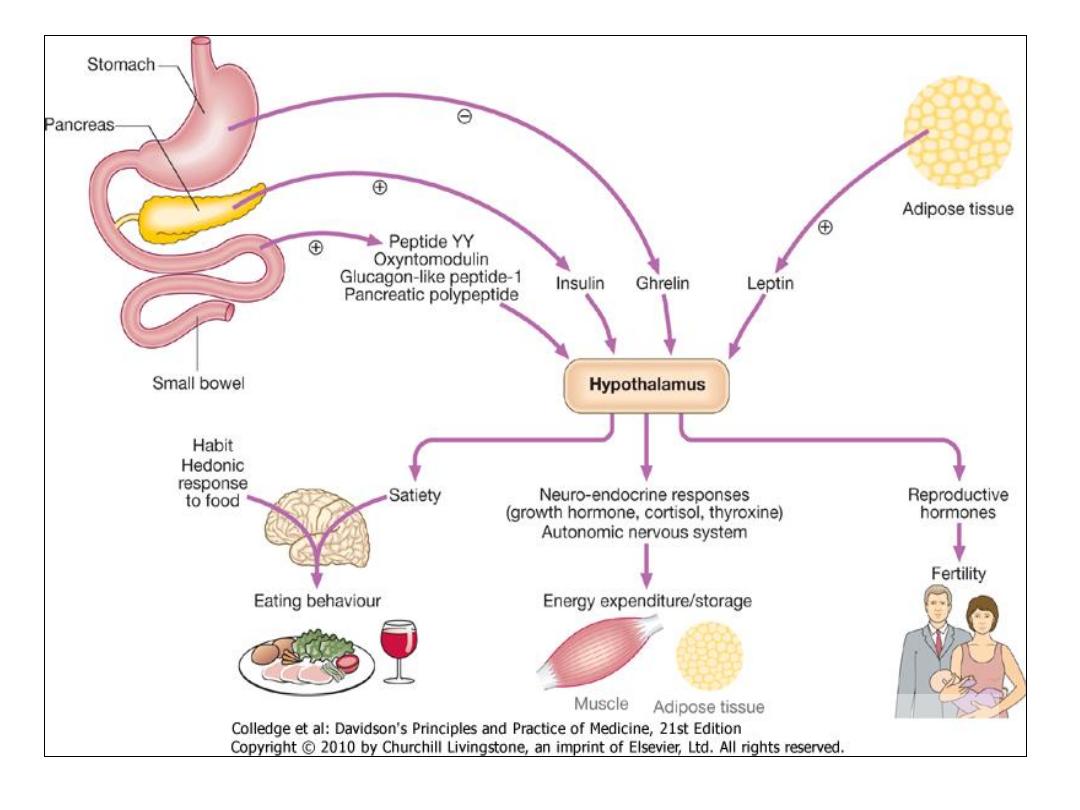
Response to under- and over-nutrition
under-nutrition over-nutrition
BMR
energy preserved BMR
low insulin
energy consumed
glycogen depletion
high insulin
the triglyceride depletion increase fat store
as triglyceride
the protein breakdown disease state

Carbohydrates
• Carbohydrates are the
sugars
and
starches
found in foods.
• There are two general types of carbohydrates:
simple
and
complex
.
• At least
55%
of total calories should be derived from
carbohydrates.
( 100-200 g/ d )
• No
individual carbohydrate is an essential nutrient as
carbohydrates can be synthesized de novo from protein.

Simple Carbohydrates
These sugars are
fructose
and
glucose
(found in fruits and
vegetables,
lactose
(found in milk), and
sucrose
(table sugar).
• The most important to the body is
glucose
– the form of the
sugar that goes directly to the bloodstream and
• provides quick energy. All other sugars must be changed into
glucose by the body before the cells can use them. The cells
use glucose as their primary source of energy. Glucose that is
not needed immediately is converted by body to
glycogen
, a
form of starch stored in the muscles and liver.
Complex Carbohydrates
• Starches
are complex
carbohydrates that are made up
of many units of glucose. These
chains must be broken down by
the body into single units of
glucose before they can be used.
simple sugars.
Breads, cereals,
and potatoes
contain starch.
• Dietary Fiber
is another complex
carbohydrate, which comes from
non-digestible part of plants.
There two types of dietary fiber:
soluble
and
insoluble
. Soluble
fiber combines with waste to
assist in their removal.
( bran,
beans, apples, carrots, and other
vegetables)
• Insoluble fiber absorbs water
and helps to provide needed
bulk to the diet.
(whole grains
and the skins and seeds of fruits
and vegetables).

DIETARY CARBOHYDRATES
Free sugars
Monosaccharides :Glucose, fructose
Disaccharides : Sucrose, lactose, maltose
fruits, milks, vegetables
Starch polysaccharides
: Cereals (wheat, rice), root
vegetables (potato), legumes (lentils, beans,
peas)
Non-starch polysaccharides
: (NSP, dietary fibre)
Plants Cellulose, Hemicellulose
Fats (Lipids)
•
Fats
are the nutrients that contains the most
concentrated form of energy.
•
Fatty acids
have the highest energy density of
the macronutrients (9 kcal/g)
•
30%
of calorie should be derived from the fat
• Fats
are part of many body tissues and are
important as carriers of other nutrients, such
as vitamins. Fats also carry the flavor of foods
– making foods tastier.

Types of Fats
•
Saturated fats
are usually
solid at room
temperature. They
contain maximum number
of hydrogen atoms.
butter, and animal fats
tend to be high in
saturated fats.
• A diet high in saturated
fats can lead to an
increased chance of
coronary artery disease.
•
Unsaturated
fats are those
fats that are liquid at room
temperature.
• Olive oil and peanut oil
• Fish oils and most
vegetables oils, such as
corn, soybean, and
sunflower oils.
Protein
•
Proteins
are substances found in every cell. The body needs
proteins to build and repair all body tissues. Proteins are made up
of basic units called
amino acids
.
• There are
20 different amino acids
. Nine of them are essential,
and the other eleven amino acids can be
• produced by the body.
10 – 15
% of energy derived from it.
•
Complete proteins
Incomplete proteins
Legumes cereals roots
eggs milk and meat
Nutrients that Regulate
•
Vitamins, minerals,
and
water
are nutrients that
work with the energy-providing nutrients to be sure that
the body functions properly.
• Water is the most vital nutrient because it provides the
means for all other nutrients to be carry throughout the
body.
• Vitamins, minerals, are not digested by our body, and
they do not provide Calories. They work with
carbohydrates, fats, and proteins to promote growth and
regulate body processes.

Vitamins
they also help
change
carbohydrates and
fat into energy.
• Because the body
cannot make most
vitamins, they must
be supplied by the
foods .
•
Vitamins
are organic
substances with the key
roles in certain metabolic
pathways.
Water-soluble Vitamins
•
Thiamin (B1),
Riboflavin (B2), Niacin, Vitamin B6, Folate
(Folic acid), Vitamin B12, Pantothenic acid ,
biotin, choline Vitamin C (Ascorbic acid).
• Fat- soluble vitamins:
vit A, vitD , vitE , vitK
Minerals
• Minerals
are simple substances found in the
environment that are essential to the body’s
functioning.
• Minerals
are used to regulate a wide range of
body processes, from bone formation to blood
clotting.
• Most
minerals
are either quickly used or lost
in waste products, therefore we must eat
mineral-rich foods daily to replenish our
supply. Iron is an exception –it tends to be
kept and recycled by the body.

Major Minerals:
calcium, phosphorus, magnesium,
potassium, sodium .
• Calcium
keeps the nervous system working well
and is needed for blood clotting. Osteoporosis is
disease caused by calcium deficiency.
• Sodium
and
potassium
help regulate the passage
of fluids in and out of cells. Too much sodium in
the diet may aggravate high blood pressure or
hypertension, increasing the risk of heart attack,
stroke or kidney disease. Table salt is one source
of sodium in the diet.
Trace Minerals:
iron, iodine, manganese, zinc, copper, and fluorine
• The majority of the minerals needed for the body to function
are only required in very small, or trace amounts.
• Iron is a vital part of hemoglobin – a substance in red blood
cells that carries oxygen to all parts of the body. Insufficient
iron may cause anemia.
• Iodine is needed for the thyroid gland to function properly.
The thyroid gland produces hormones that control how
quickly chemical reactions occur in our body. Too little iodine
– thyroid gland enlarged. The primary sources are seafood
and iodized table salt.

Standards of Nutrition
• Dietary Reference Intakes (DRIs)
– Quantitative estimates of nutrients
collectively for proper function and health
• Recommended Daily Allowances (RDA)
• The average daily dietary intake that meets
the nutrient requirement of nearly all
healthy persons of a specific sex, age, life
style or physiological condition.
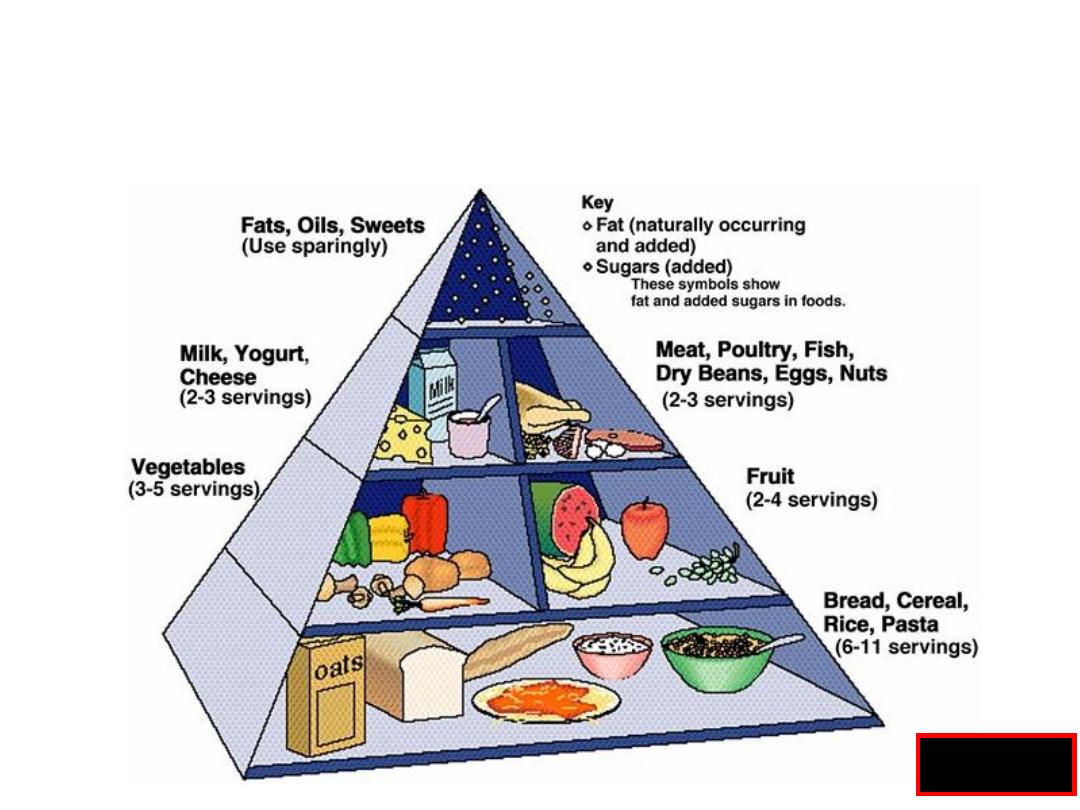
The Food Guide Pyramid
Fig 18.2

Malnutrition
Definition
:
loss of the lean body mass and adipose tissue
due to insufficient dietary supply
1.
primary
: inadequate or poor-quality food intake (war or
famine).
2.
secondary
: from diseases that alter food intake or
nutrient requirements, metabolism, or
absorption.
Two syndrome
:
kwashiorkor (malnutrition with edema)
marasmus (malnutrition with marked muscle-wasting).

CAUSES OF malnutrition
Decreased the energy intake ( hypo metabolism)
Economic
: poverty, famine
anorexia :
nervosa, dementia ,depression
cancer , renal failure
Abdominal pain
: pancreatitis, intestinal
ischemia
Impaired diet transit
: benign and malignant
esoph.
or gastric obstruction
Maldigestion
: pancreatic exocrine
insufficiency, short bowel
syndrome
Malabsorption
: small intestinal disease(celiac
disease

Causes of malnutrition
Increased energy expenditure (hyper metabolism)
Increased BMR
: (thyrotoxicosis , fever, cancer
trauma , sepsis, surgery,burn)
Excessive physical activity
( marathone runner )
Acute and chronic inflammation
: T.B
,collagen diseases.
Energy loss
:(e.g. glycosuria in diabetes)
Mixed mechanisms
Disseminated cancer
Chronic inflammatory bowel disease (crohns
disease
Consequences of malnutrition
Wt loss
Weakness
Loss of cell
mediated immunity Bronchopneumonia
Too week to walk
Urinary tract
infection
Too week to sit
Bed sore
death
Metabolic response to the Starvation
:
First day:
• Circulating glucose and FA and TGs , liver and muscle glycogen
(1200 Kcal ).
• Lipolysis for the FAs production (65% of energy source )
First few days :
• Lipolysis increase and ketone body production
increase
• Gluconeogenesis begin (70 g),15% from protein
2 weeks-30 days
:
• Energy conserved , BMR decrease , thyroids hormones
decrease , sympath. system decrease
• Lipolysis continue 150g/day (90% on fat)
• Muscle PTN breakdown decrease(20g/day)

Metabolic response to stress
• High catecholamines ,glucagon , cortisol
cytokines , TNF , int 1,6
• Skeletal and visceral PTN catabolism (150 g/d)
• 50 % of body protein stores within 3 weeks

Physiological consequences
1. GIT :
Atrophy of small IN. mucosa
Gastric and pancreatic secretion
Volume of bile and conjugated bile acids decrease
Carbohydrate. and fat malabsorption decrease.
2.CVS:
Myocardial Mass and function decrease
3.Immune system
:
Lymphocyte count decrease
Delayed skin hypersensitivity
Decrease production of ABs

4.Respiratory:
• Structural and functional atrophy
5.Bone marrow
:
• Decrease lymphocyte and WBC and RBC
6.Renal :
• Decrease mass and function
7.Skin and hair:
• Dry ,thin, wrinkled , hyperkeratosis
• Wound healing
8.Endocine
Low insuline
Increase cortisol
Increase growth homone
T3and t4 decrease
Primary gonadal dysfuction

.
Clinical features:
WT loss
Weakness and, craving for food
muscle wasting
Loss of subcutaneous fat
Leg edema and ascites
Skin dry pale lax, easy packable thin hair
amenorrhea or impotence
Bradycardia Cold cyanosed extremities, pressure sores
distended abdomen, with diarrhea
apathy, depression, loss of the initiative
Features of associated vitamins deficiency
susceptibility to infections

INFECTIONS ASSOCIATED WITH PEM Patients
:
• Gastroenteritis
• Gram-negative septicemia
• Respiratory infections, especially
bronchopneumonia
• viral infection :herpes simplex
• Tuberculosis
• Streptococcal and staphylococcal skin
infections
• Helminthic infestation

Nutritional Assessment
• History
• Physical examination
• Anthropometric measurements
• Laboratory investigations
• Functional test

Nutritional Assessment
History
Dietary Analysis
Dietary history Review foods eaten
Review preparation methods
Evaluate digestive and absorption adequacy
Review supplements taken
Significant weight loss within last 6 months
> 10% loss of body weight
<90% 0f ideal body weight

patient History of Weight Loss
Finding
Example
Involuntary diet restriction
Poverty due to inadequate income
Anorexia
Anorexia nervosa, severe depression,
dementia, cancer, chronic renal failure
Inadequate diet selection
Chronic alcoholism, strict vegetarianism
Critical illness
trauma, burn, major surgery, sepsis
Dysphagia
Esophageal obstruction
Nausea, vomiting
Gastric or intestinal obstruction
Chronic abdominal pain
chronic pancreatitis, intestinal angina
Chronic diarrhea
Pancreatic, intestinal mucosal

Physical Examination
Evidence of muscle wasting
Depletion of subcutaneous fat
Peripheral edema, ascites
Skin changes (easily plucked hair)
Features of Vitamin deficiency
e.g. nail and mucosal changes
Nutritional Assessment

Anthropometry
Weight for Height comparison
Body Mass Index(BMI)
Triceps-skin fold
< (6mm for the men), <(8mm for the women)
Mid arm muscle circumference
<(20cm for the men),<(18.5cm for the women)
Nutritional Assessment

BODY MASS INDEX (WEIGHT/HEIGHT2)
BMI (kg/m2)
classification
> 25
obese
>20
Adequate nutrition
18.5-20
Marginal
< 18.5
Malnutrition
17-18.5
Mild
16-17
Moderate
< 16
Severe

Lab investigations
1. Serum visceral protein:
albumin < 30 mg/dl
transferrin < 150 mmol/l
pre-albumin <12 mg/dl
Nutritional Assessment
2. vitamin and minerals assays:
tests reflecting specific nutritional deficits
e.g. prothrombin time
3.Assessment of immune function:
Total lymphocyte count < 1800 / mm3
Skin anergy testing
Nutritional Assessment

Nutritional Assessment
Functional test
Hand grip dynamometry
Other
Urinary creatinine excretion:
1g of urine creatinine:18.5g of FFM
23mg/kg of ideal body wt./men
18mg/kg of ideal body wt./women
bioelectric impedance analysis

Nutritional therapy

Nutritional therapy
• Provide a life sustained therapy for the
patient who can not take adequate food by
mouth who consequently at risk for
malnutrition and its complication

Benefits of Nutritional Support
• Preservation of nutritional status
• Prevention of complications of protein
malnutrition
•
Post-operative complications

Nutritional therapy given when
• 1. improve the quality of life.
• 2. improve the ability to recover from the
disease.
Don’t forget it depend
: disease outcome
severity of the
malnutrition
any additional stress
risk of nutritional therapy

Who Requires
Nutritional Support?
• Patients already with malnutrition –
surgery / trauma/sepsis
• Patients at risk of malnutrition

Patients at Risk of Malnutrition
Cannot eat for >9 days
Vomiting
: acute pancreatitis
,hperemesis gravidarum
GIT obstruction
: malignancy
neurological :
coma , swallowing dis.
Abdominal pain
: A. pancreatitis
Can not absorb
: intestinal fistula ,short
bowel syndrome
Should not eat
: bowel rest in
a.pancreatitis
Intestinal fistula ,crohns disease

• Others
nutritional support in patient with malignancy
nutritional support in malnourished patient
before surgery

Type of the nutritional
rehabilitation
• Normal diet
mild malnutrition and
treatable disease
• Supplement
high energy and protein
content used if normal
diet
cant give
sufficient nutrition
• Specific Nutritional support
Enteral feeding
Parentral feeding

Types of Nutritional Support
Enteral Nutrition
Parenteral Nutrition

Enteral Feeding Is Best
• More physiologic
• Less complications
• Gut mucosa preserved
• No bacterial infection
• Cheaper

Enteral Feeding Is Indicated
• When nutritional support is
needed
• Functioning gut present
• No contra-indications
– no ileus, no recent anastomosis, no
fistula
Types of Feeding Tubes
• Naso-gastric tubes
• Naso-duodenal
tubes
• Naso-jejunal tubes
Tubes inserted down the upper GIT,
following normal anatomy
Types of Feeding Tubes
• Gastrostomy tubes
– Percutaneous Endoscopic Gastrostomy (PEG)
– Open Gastrostomy
• Jejunostomy tubes
Tubes that require an invasive
procedure for insertion(feeding for long time)
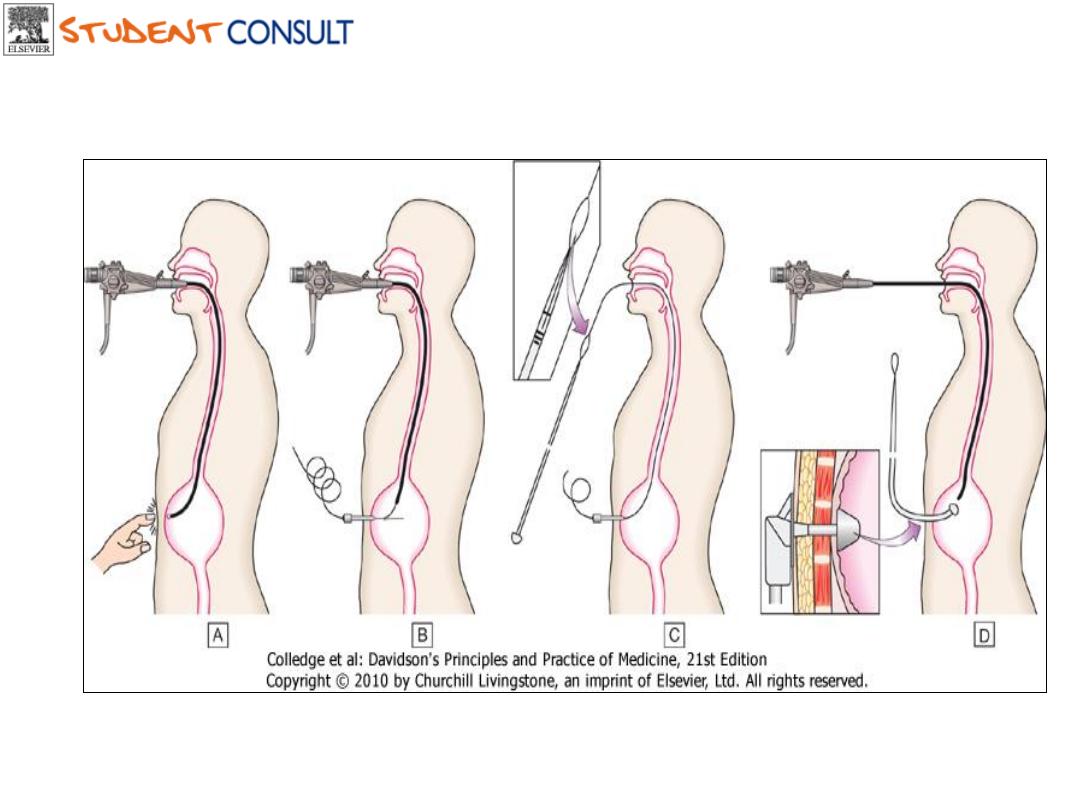
Downloaded from: StudentConsult (on 29 October 2011 12:19 AM)
© 2005 Elsevier


What Can We Give
in Tube Feeding?
Blenderised feeds
Commercially prepared feeds
• e.g. Vivonex

Complications
of Enteral Feeding
12% overall complication rate
• Gastrointestinal complications
• Mechanical complications
• Metabolic complications
• Infectious complications

Complications
of Enteral Feeding
Gastrointestinal
• Distension
• Nausea and vomiting
• Diarrhoea
• Constipation

Complications
of Enteral Feeding
Infectious
• Aspiration pneumonia
• Bacterial contamination
Complications
of Enteral Feeding
Mechanical
• Malposition of feeding tube
• Sinusitis
• Ulcerations / erosions of nasal and esoph
• Blockage of tubes

Parenteral Nutrition

Parenteral Nutrition
Allows greater caloric intake
BUT
• Is more expensive
• Has more complications
• Needs more technical expertise

Who Will Benefit From
Parenteral Nutrition?
Patients with/who
– Abnormal gut function
– Cannot consume adequate amounts of
nutrients by enteral feeding
– Are anticipated to not be able to eat
orally by 5 days
– Prognosis warrants aggressive nutritional
support
Two Main Forms of
Parenteral Nutrition
• Peripheral Parenteral Nutrition
• Central (Total) Parenteral
Nutrition

Peripheral Parenteral Nutrition
Given through peripheral vein
• Short term use
• Mildly stressed patients
• Low caloric requirements
• Needs large amounts of fluid
• Contraindications to central TPN

What to Do Before Starting TPN
• Nutritional Assessment
• Venous access evaluation
• Baseline weight
• Baseline lab investigations

Baseline Lab Investigations
• Daily
: urea , electrolytes, glucose
• Twice weekly
: LFT, calcium,
phosphate, magnesium
• Weekly:
CBC, zinc, triglycerides
• Monthly:
copper, selenium,
manganese


Formula of the TPN
• Dextrose 10% ,20% glucose
• Intralipid 10%, 20% fatty acid
• Vamine ( amino acid) 8%, 14%
• Vitamins
• Minerals
• Trace elements

Complications Related to TPN
• Mechanical Complications
• Metabolic Complications
• Infectious Complications
Mechanical Complications
Related to vascular access technique
• pneumothorax
• air embolism
• arterial injury
• bleeding
• brachial plexus injury
• thoracic duct injury
Mechanical Complications
Venous thrombosis
Catheter occlusion
Related to catheter in situ

Metabolic Complications
Abnormalities related to excessive
or inadequate administration
– hyper / hypoglycemia
– Fluid and electrolyte:
Refeeding
syndrome
hypomagnesemia, hypokalemia,
hypophosph
Congestive heart failure
– acid-base disorders

Metabolic Complications
Hepatic complications
• Biochemical abnormalities
• Cholestatic jaundice
• Hepatic steatosis
• Gall stones
• Acalculous cholecystitis

Infectious Complications
◦ Insertion site contamination
◦ improper insertion technique
◦ use of catheter for non-feeding purposes
◦ contaminated TPN solution
◦ contaminated tubing
• Secondary contamination
– septicaemia
