Infection in immuncompromized patient
Dr.Mustafa NemaBaghdad College of Medicine
2014
Objectives
Describe the main types of immunocompromised conditionsReview the causes of immune suppression
List the major types of infections associated with altered immunity
Outline management of such infections
Dr.Mustafa Nema/Baghdad College of Medicine 2014
ImmunityTwo Intrinsic Defense Systems
1. Innate (nonspecific) system.
Responds quickly and consists of:
First line of defense – intact skin and mucosae prevent entry of microorganisms
Second line of defense – antimicrobial proteins, phagocytes, and other cells
Dr.Mustafa Nema/Baghdad College of Medicine 2014
2. Adaptive (specific) defense system
If the innate immune system fails to provide effective protection against an invading pathogen, the adaptive immune system is mobilisedInclude humoral immunity ( B cells, Ab producing) and cell- mediated immunity (T cells non-Ab producing ).
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Immune-competent and immune-compromised bodyWhen immune system function is normal = immune-competent and vice versa with immune-compromised.
Immunodeficiency (or immune deficiency) is a state in which the immune system's ability to fight infectious disease is compromised or entirely absent.
Immune deficiency may arise through primary (intrinsic) defects in immune function, but is much more commonly due to secondary causes, including drug therapy, malignancy and ageing.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Immunocompromising conditions
Primary (Congenital) conditionsCongenital conditions most commonly affect the newborn and children.
Classes of congenital conditions include the following syndromes:
Primary phagocyte deficiencies
Complement pathway deficiencies
Primary deficiencies of the adaptive immune system
Primary T-lymphocyte deficiencies
Combined B- and T-lymphocyte immune deficiencies
Primary antibody deficiencies
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Examples of primary immune deficiency
• Example 1• Primary T-lymphocyte deficiencies:
These are characterised by recurrent viral, protozoal and fungal infections .
The immune deficiency is characterised by very low numbers of circulating T cells.
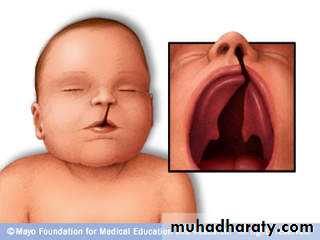
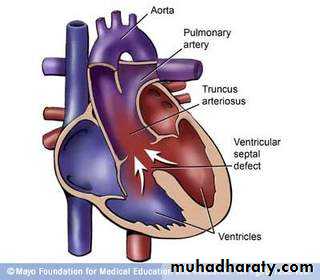
These disorders generally present in childhood e.g. DiGeorge syndrome
Dr.Mustafa Nema/Baghdad College of Medicine 2014
DiGeorge syndrome : associated with multiple abnormalities, including congenital heart disease, hypocalcaemia tracheo-oesophageal fistulae, cleft lip and palate, and absent thymic development.Dr.Mustafa Nema/Baghdad College of Medicine 2014
Example 2
Primary antibody deficiency:
Selective IgA deficiency:
Is the most common primary immune deficiency that can also present in adulthood.
In most patients, low or undetectable IgA is an incidental finding with no clinical sequelae.
However, 30% of individuals experience recurrent mild respiratory and gastrointestinal infections.
In some patients, there is a compensatory increase in serum IgG levels.
Specific treatment is generally not required.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Investigations
Investigations include serum immunoglobulins, and B and T lymphocyte counts in blood.Management
With the exception of individuals with selective IgA deficiency, patients with other antibody deficiencies ( like IgG, IgM) require aggressive treatment of infections, and prophylactic antibiotics may be indicated.
The mainstay of treatment is life-long immunoglobulin replacement therapy.
Immunisation is generally not effective. Why?
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Secondary immune deficienciesSecondary immune deficiencies are much more common than primary immune deficiencies.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Causes of secondary immune deficiency
Physiological
• • Ageing
• • Prematurity
• • Pregnancy
Infection
• • HIV
• • Measles
• • Mycobacterial infection
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Iatrogenic
• • Immunosuppressive therapy• • Antineoplastic agents
• • Corticosteroids
• • Stem cell transplantation
• • Radiation injury
• • Some anti-epileptic agents
Malignancy
• • B-cell malignancies including leukaemia, lymphoma and myeloma
• • Solid tumours
• • Thymoma
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Biochemical and nutritional disorders
• • Malnutrition
• • Renal insufficiency/dialysis
• • Diabetes mellitus
• • Specific mineral deficiencies, e.g. iron, zinc
Other conditions
• • Burns
• • Asplenia/hyposplenism
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Common causes of secondary immune defeciency include infections, such as HIV and measles, and cytotoxic and immunosuppressive drugs, particularly those used in the management of transplantation, autoimmunity and cancer.
Physiological immune deficiency occurs at the extremes of life.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
How can a patient with immune deficiency presents to you and how can you manage?
Dr.Mustafa Nema/Baghdad College of Medicine 2014Most patients with an immune deficiency present with: Recurrent Infections.
An immunocompromised person may be particularly vulnerable to opportunistic infections, in addition to normal infections that could affect everyone.Dr.Mustafa Nema/Baghdad College of Medicine 2014
In primary immune deficiency..
Many warning signs may help in suspecting the presence of primary immune deficiency in newborn /childhood.The presence of ≥ 2 warning signs may indicate an underlying primary immunodeficiency:
• ≥ 4 new ear infections within 1 yr
• ≥ 2 serious sinus infections within 1 yr
• ≥ 2 months on antibiotics with little effect
• ≥ 2 pneumonias within 1 yr
Dr.Mustafa Nema/Baghdad College of Medicine 2014
• Failure of an infant to gain weight or grow normally
• Recurrent, deep skin or organ abscesses• Persistent thrush in mouth or fungal infection on skin
• Need for intravenous antibiotics to clear infections
• ≥ 2 deep-seated infections, including septicaemia
• A family history of primary immune deficiency
Dr.Mustafa Nema/Baghdad College of Medicine 2014
In patient with infection and secondary immune deficiency suspected..The following should be addressed in the history:
• • Identification of the immunosuppressant factors, and nature of the immune defect.
• • Any past infections and their treatment.
• • Exposure to infections, including opportunistic infections that would not cause disease in an immunocompetent host.
• • Prophylactic medicines and vaccinations administered.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Examination:
Examination should include inspection of the normal physical barriers provided by skin and mucosal surfaces and, in particular, central venous catheters, the mouth, sinuses, ears and perianal area. ( Do Not forget hidden areas )
The areas around fingernails and toenails should also be inspected closely.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Investigations
If the clinical features do not suggest a specific infection, then initial investigations should include:• (ANA).
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Chest X-ray and chest CT scan should be considered when respiratory symptoms occur.
Abdominal imaging may also be warranted, particularly if there is right lower quadrant pain, which may indicate typhlitis (inflammation of the caecum) in neutropenic patients.Culture of the blood, central venous catheter site, urine, and stool if related symptoms and sign present.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Specific conditions
Dr.Mustafa Nema/Baghdad College of Medicine 2014Neutropenic fever
Neutropenia is a common complication of malignancy.
It is usually secondary to chemotherapy but may occur with radiotherapy if large amounts of bone marrow are irradiated.
It may also be a component of pancytopenia due to malignant infiltration of the bone marrow.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
A reduction in neutrophil count (usually less than 1.5 × 109/L, but dependent on age and race) is called neutropenia
The risk of bacterial infection is related to the degree of neutropenia, with counts lower than 0.5 × 109/L considered to be critically low.
The risk of sepsis is related to the severity and duration of neutropenia and the presence of other risk factors such as intravenous or bladder catheters.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Neutropenic fever is an emergency in cancer patients as, if left untreated, it can result in septicaemia with a high mortality rate.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Clinical featuresThe typical presentation is high fever and affected patients are often non-specifically unwell.
Examination is usually unhelpful in defining a primary source of the infection.
Hypotension is an adverse prognostic feature and may progress to systemic circulatory shutdown and organ failure
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Investigations and Treatment
An infection screen should be performed.
Typical first-line empirical therapy consists of an anti-pseudomonal β-lactam (ceftazidime, cefotaxime or meropenem), or a combination of an aminoglycoside and a broad-spectrum penicillin with anti-pseudomonal activity (gentamicin and piperacillin).
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Metronidazole should be added if anaerobic infection is suspected, and flucloxacillin or vancomycin or teicoplanin when Gram-positive infection is suspected (for example, in patients with central lines).If there is no response after 36–48 hours, treatment with amphotericin B or voriconazole should be considered to cover fungal infection.
Other supportive therapy, including intravenous fluids and dialysis, may be required.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Infections in transplant recipients
Infections in solid transplant recipients are grouped according to the time of onset.Those in the first month are related to the underlying condition or surgical complications.
Those occurring 1–6 months after transplantation are characteristic of impaired T-cell function.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Time post-transplantation
• InfectionsSolid organ recipients
0–1 mthBacterial or fungal infections related to the
underlying condition or surgical
complications
1–6 mths
CMV, other opportunistic infections (e.g.
Pneumocystis jirovecii pneumonia)
> 6 mths
Bacterial pneumonia, other bacterialcommunity-acquired infections, shingles,
cryptococcal infection.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Types of immune deficiency, causes and resultant infectionDr.Mustafa Nema/Baghdad College of Medicine 2014
• Humoral immune deficiencyB cells, plasma cells or antibodies
• Primary humoral• Multiple myeloma
• Chronic lymphoid leukemia
• AIDS
• Streptococcus pneumoniae
• Hemophilus influenzae
• Pneumocystis jirovecii
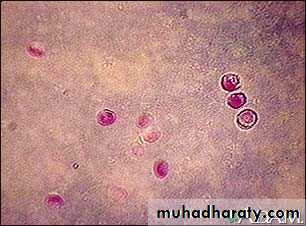
• Giardia intestinalis
• Cryptosporidium parvum
Type of immune deficiency
• Affected components
• Main causes
Main pathogens of resultant infectionsDr.Mustafa Nema/Baghdad College of Medicine 2014
Cryptosporidium parvumStrept pneuomonia
Dr.Mustafa Nema/Baghdad College of Medicine 2014
T cell deficiencyT cells
• Marrow and other transplantation
• AIDS
• Cancer chemotherapy
• Lymphoma
• Glucocorticoid therapy
• Intracellular pathogens, including Herpes simplex virus, Mycobacterium, Listeria, and intracellular fungal infections.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
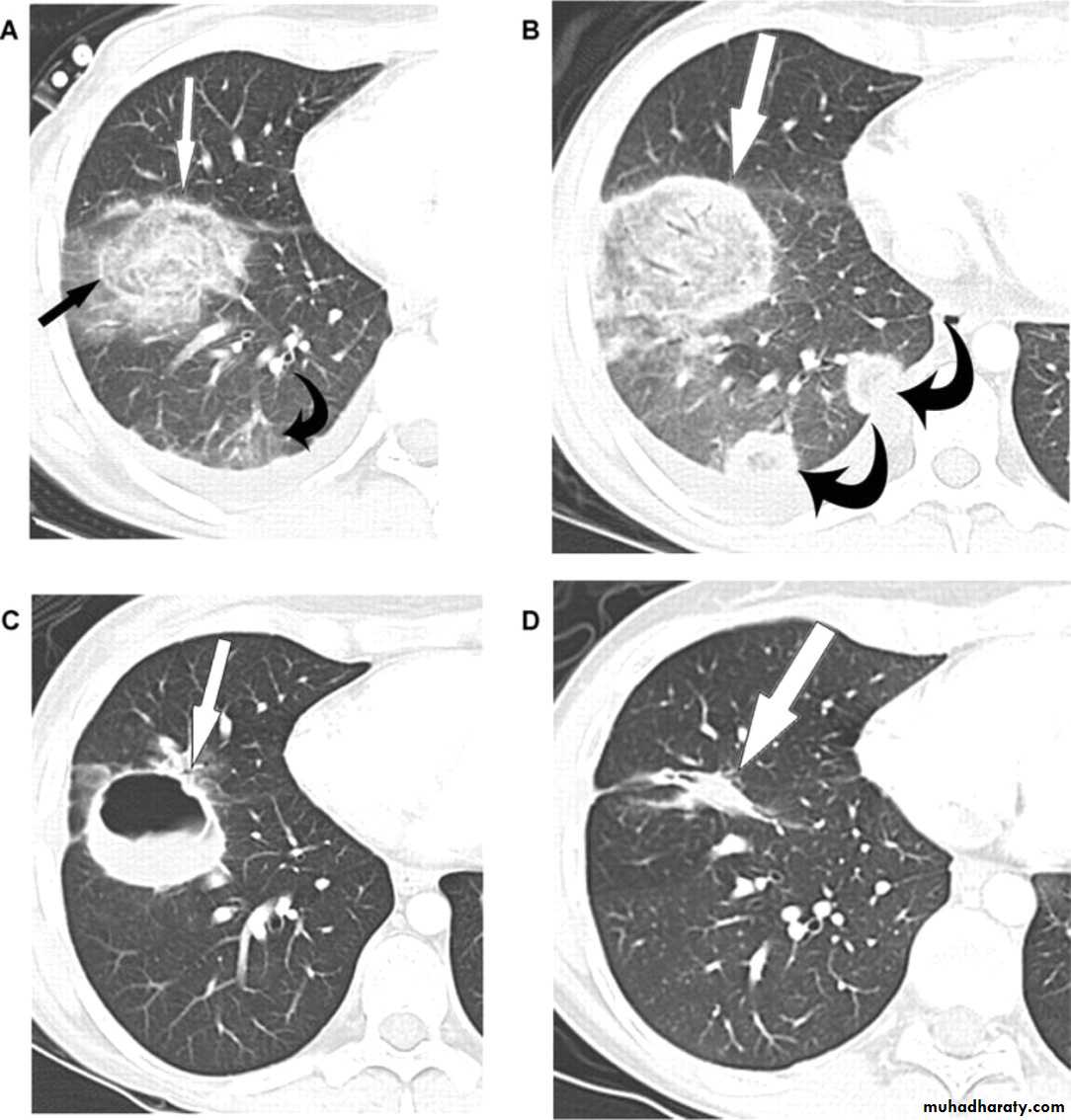
Miliary TB
Dr.Mustafa Nema/Baghdad College of Medicine 2014Neutropenia
Neutrophil granulocytes• Chemotherapy
• Bone marrow transplantation
• Dysfunction, such as chronic granulomatous disease
• Oral Streptococci
• Pseudomonas aeruginosa
• Enterococcus species
• Candida species
• Aspergillus species
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Aspergillus lung infectionDr.Mustafa Nema/Baghdad College of Medicine 2014
AspleniaSpleen
• Splenectomy
• Trauma
• Sickle-cell anemia
Polysaccharide encapsulated bacteria,particularly:
• Streptococcus pneumoniae
• Haemophilus influenzae
• Neisseria meningitidis
• Plasmodium species
• Babesia species
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Complement deficiencyComplement system
Congenital deficiencies
• Neisseria species
• Streptococcus pneumoniae
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Opportunistic infections
BacterialMycobacterial infections including M.avium complex
Legionellosis
Nocardia
Actinomycetes
Salmonellosis
Campylobacter infection
Viral
CMV
Herpes simplex
Adenovirus
Dr.Mustafa Nema/Baghdad College of Medicine 2014
ParasiticPneumocystis jirovecii pneumonia (PJP). the old name is P.carinii pneomonia (PCP)
Toxoplasmosis
Cryptosporidiosis
Isosporiasis
Generalised strongyloidiasis
Fungal
Candidosis
Cryptococcosis
Aspergillosis
Histoplasmosis
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Pneumocystis jirovecii
pneumoniaDr.Mustafa Nema/Baghdad College of Medicine 2014
VaccineNew guidelines recommend that most immunocompromised patients should be vaccinated.
Dr.Mustafa Nema/Baghdad College of Medicine 2014
Readings
Davidson clinical and practice of medicine 22th ed. 2014.www.emedicine.medscape.com
Dr.Mustafa Nema/Baghdad College of Medicine 2014