Calcium Disorders
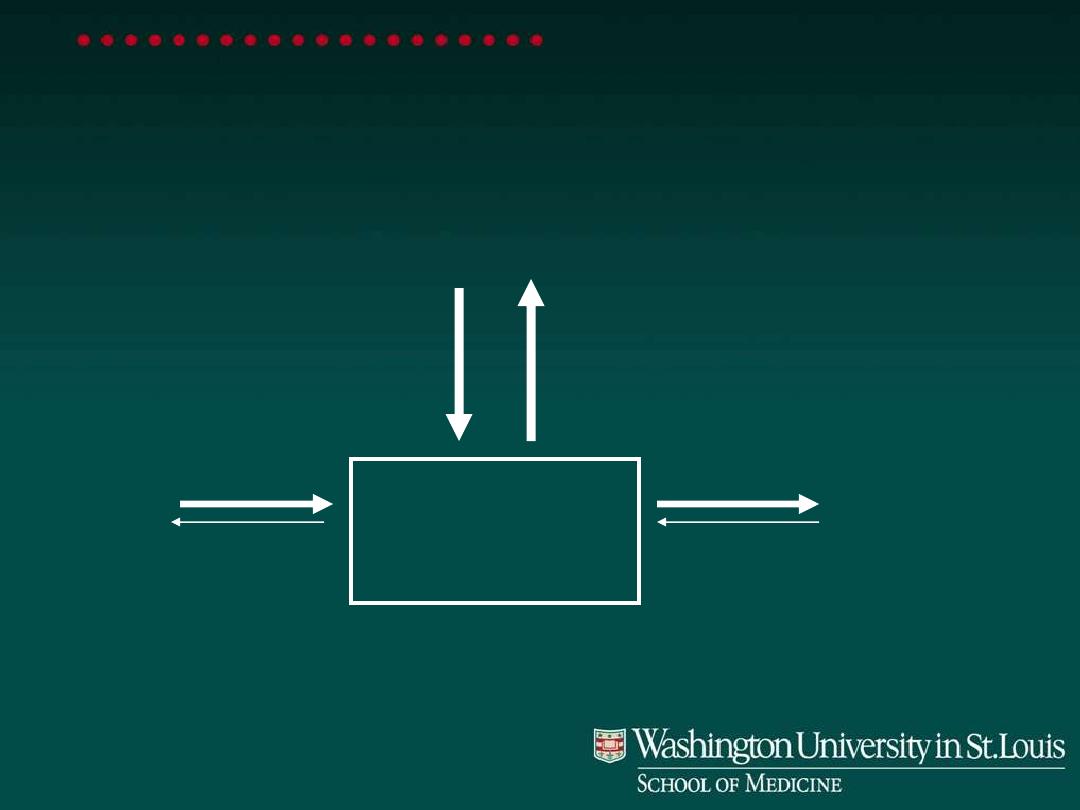
Calcium balance
ECF CALCIUM
GUT
KIDNEY
BONE (1 kg)
Net 175 mg
Net 175 mg
500 mg
500 mg
1000 mg

Hypercalcemia: clinical signs
GI:
•
Nausea, vomiting, abdominal pain& Constipation
•
Acute pancreatitis and gastric ulcer
Renal:
Polyuria, dehydration, renal calcification&Renal failure
Neurological
Fatigue ,Confusion ,Stupor, coma
Increased neuromascular excitability& muscle weakness
Heart
Characteristic ECG, and in severe cases cardiac arrest

Hypercalcemia: major causes
Primary hyperparathyroidism
(PHPT), and Tertiary
hyperparathyroidism THPT
Malignancy
Others

Hyperparathyroidism: causes
Primary PHPT
•
Adenoma (90%)
•
Multiple gland enlargement (10%)
–
MEN 1
–
MEN 2A
–
Familial hyperparathyroidism
•
Carcinoma (<1%)
•
Familial benign hypercalcemia (FBH)
Tertiary THPT
It occurred as a result of secondary HPT

In
PHPT,
there
is
autonomous
inappropriate secretion of PTH from the
gland(mainly because of tumor) and this
secretion is not subjected to negative
feed back of hypercalcemia. In THPT, the
autonomous secretion of PTH is due to
sustained and prolonged stimulation of
the
parathyroid
gland
by
previous
hypocalcemia that caused by either renal
failure and/or vitamin D deficiency.

In Renal failure and vitamin D deficiency,
the
resulted
hypocalcemia
is
not
corrected even by stimulated secretion of
PTH, this referred to secondary HPT,
which characterized
by
↓ S.Ca, normal
PO4 - -, and
↑S.PTH. The continues
stimulation
of
PTH
gland
leads
to
hypertrophy
of
it
with
resultant
autonomous secretion of PTH
which
unable to correct hypocalcemia because
of renal damage or deficeint vitamin D.

Only after correction of underlying cause of
hypocalcemia by kidney transplantation or
vitamin D supplementation, the serum levels of
Ca will be corrected and increased because of
gland hypertrophy, and this state referred to
THPT in which
↑ S.Ca, ↓S.PO4 - -, ↑S.PTH and
the differentiating parameter between the PHPT
and THPT is the marked increased of S.ALP in
THPT, but normal in THPT, and the history of
previous
hypocalcemia
in
THPT.

Malignant hypercalcemia: major causes
PTHrP - mediated
•
Breast carcinoma
•
Squamous carcinoma (lung, head & neck,
esophagus)
•
Renal carcinoma
Cytokine - mediated
•
Myeloma (lymphoma, leukemia)

Hypercalcemia: other causes
Drugs:
•
Vitamin D
•
Calcium carbonate (milk alkali syndrome)
•
Lithium
•
PTH
•
Vitamin A
Sarcoidosis, other granulomatous disorders
Hyperthyroidism

Hypercalcemia: presentations
Chronic, mild-moderate
•
Often asymptomatic
•
Cause: primary hyperparathyroidism
•
Issues: parathyroidectomy or not
Acute, severe
•
Symptomatic
•
Cause: malignant hypercalcemia (rarely others)
•
Issues: treat hypercalcemia, find & treat cause

Primary hyperparathyroidism
F:M 3:1
Usually > 50 y/o
Presentation:
•
Asymptomatic hypercalcemia (>50%)
•
Renal stones (20%)
•
Decreased bone density
•
Symptoms of hypercalcemia (<5%)

Hypercalcemia: evaluation
Duration >6 months or renal stones: PHPT
Signs of malignancy, other rare causes
Plasma PTH
•
Normal or elevated: primary
hyperpararthyroidism
•
Low: other causes
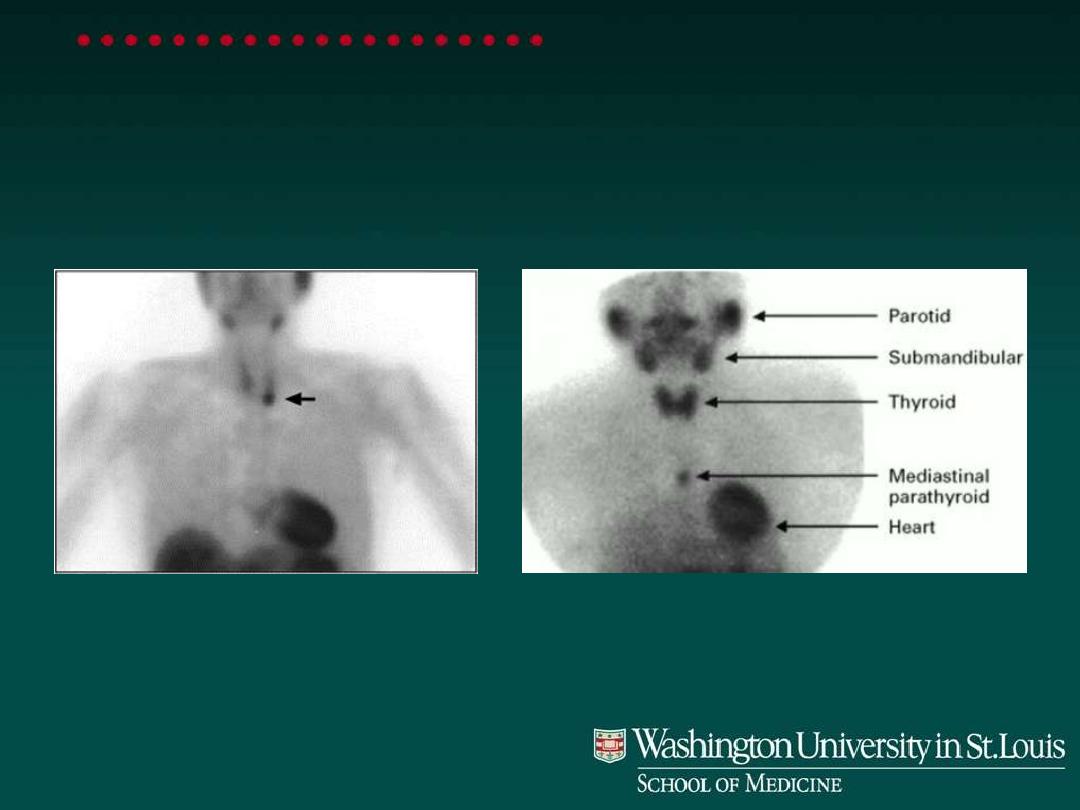
Parathyroid Localization
Sestamibi scans
Left lower parathyroid adenoma
Mediastinal parathyroid adenoma

Biochemical
evaluation:
1.
In primary hyperparathyroidism:
PTH
↑, S.Ca ↑ , S.PO4 - - ↓,
with normal renal function,
the
S.Urea and S.Creatinine
are
normal.

2. In malignancies:
a. Bony tumor; primary or
metastasis
S.Ca ↑, S.PO4 - - ↑, S.PTH ↓ and
S.ALP ↑. These are due to bone
broken down by tumor
b. humoral hypercalcemia of
malignancy: S.Ca ↑, S.PO4 - - ↓ and
S. PTHrP(PTH related protein) is
detected and increased. This PTHrP

produced by malignant tumors of
breast, bronchus, neck, head
… etc
and has the biological activity of
PTH in rising the serum levels of Ca
and decreasing serum PO4 - - levels.

Nonparathyroid hypercalcemia
Repeat history (especially drugs)
Vitamin D toxicity suspected: 25 (OH) vitamin D
Sarcoidosis suspected: 1,25 (OH)
2
vitamin D
In vit. D toxicity :
S.Ca ↑, S.PO4 - - ↑, S.PTH ↓ and S. D3
is ↑.

Severe hypercalcemia:
Indications for therapy
•
Symptoms of hypercalcemia
•
Plasma [Ca] >12 mg/dl

Hypocalcemia: clinical signs
Paresthesias
Tetany (carpopedal spasm)
Trousseau’s, Chvostek’s signs
Seizures
Chronic: cataracts, basal ganglia Ca

Trousseau’s sign

Hypocalcemia: causes
Primary Hypoparathyroidism
•
Surgical,total or partial thyroidectomy and or
parathyoidectomy
•
Autoimmune
•
Magnesium deficiency;it is important for PTH
secretion
PTH resistance (pseudohypoparathyroism)
Vitamin D deficiency
Vitamin D resistance
Other: renal failure, pancreatitis

Hypocalcemia: evaluation
Confirm low corrected (change in protein
bound)& ionized calcium(Free Ca
History:
•
Neck surgery
•
Other autoimmune endocrine disorders
•
Causes of Mg deficiency
•
Malabsorption
•
Family history

Hypocalcemia: evaluation
Physical exam:
•
Signs of tetany
Lab
•
PTH
•
Creatinine, Mg, P, alkaline phosphatase
•
25-OH vitamin D

Hypocalcemia: evaluation
Cause
Hypoparathyroidism
PTH resistance
Vitamin D deficiency
Vitamin D resistance
Phosphate
High
High
Low
Low
Other
PTH low
PTH high
25-OHD low
Alk phos
Normal
Normal
High
High 25-OHDHigh

In renal failure:
↓ S.Ca , ↑S.P, ↑ .S. Urea
and
S.Creatinine,
with
expected
increased
of
S.PTH.
Ricket in childern and Osteomalacia in
adult(demineralized bone dis.) occur due
to deficiency of vitamin D and P. In these
bone
disorder
serum
Ca
&
P
are
decreased due to 1. low intake of these
element
2.
low
intake
in
vit.
D
3.
malabsorption
of
vitamin
D(GIT
disortders) 4. defect in normal pathway
of vitamin D metabolism
5.
hereditary
hypophosphatemia

Hypocalcemia: acute therapy
IV calcium infusion
•
1-2 gm Ca gluconate (10-20 ml) IV over 10 min
•
6 gm Ca gluconate/500 cc D5W over 6 hr
•
Follow plasma Ca & P Q 4-6 hr & adjust rate
IV or oral calcitriol 0.25-2 mcg/day
Oral calcium carbonate 1-2 gm BID-TID

Hypocalcemia: chronic therapy
Oral calcitriol 0.25-2 mcg/day
Calcium carbonate 1-2 gm BID-TID

Hypophosphataemia
Serum
or
plasma
PO4-
-
may
be
associated
with
widspread
cell
dysfunction and cell death. Muscle pain
and
weakness(↑CPK), urgent phosphate
supplementation is required . Dietary
deficiency of PO4 is uncommon.
↓PO4
may occur due to; antacids, respiratory
and
metabolic(Diabetic
ketoacidosis
DKA
&
lactic
acidosis
).
Insulin
in
treatment
of
DKA
aggravate
hypophosphataemia(movement
to
IC)

Magnesium
It is an essential IC cation. It found mainly in
skel. eton, a small proportion in ECF. Mg
deficiency
rarely
occurs
as
an
isolated
phenomenon, it usually accompanied by Ca, K,
and
PO4.
However,
tetany,
cardiac
arrhythmias, and CNS abnormalities may occur
due
to
Mg
deficiency
but
not
Ca.
Hypomagnesaemia should be suspected in
case of hypocalcaemia and/ or hypokalaemia.
↓
Mg may be due to GIT, and renal disorders, and
reduced intake
