PHYSIOLOGY
Dr. Basim Mohamad Alwan Lecture 14MOTOR FUNCTIONS OF SPINAL CORD
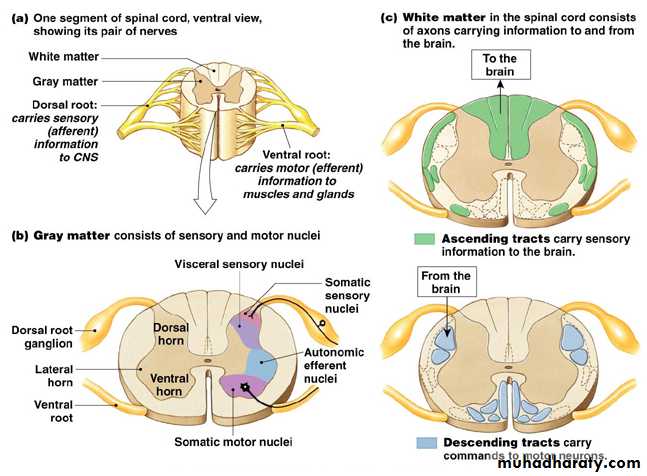
The cord gray matter is the integrative area for the cord reflexes.
Each segment of the spinal cord has several million neurons in its gray matter. Aside from the sensory relay neurons, the other neurons are of two types:(1) anterior motor neurons
(2) interneurons.
Anterior Motor Neurons.
Located in each segment of the anterior horns of the cord gray matter are several thousand neurons that are 50 to 100 per cent larger than most of the others and are called anterior motorneurons. They give rise to the nerve fibers that leave the cord by way of the anterior roots and directly innervate the skeletal muscle fibers. The neurons are of two types, alpha motor neurons and gamma motorneurons.Alpha Motor Neurons.
The alpha motor neurons give rise to large type A alpha motor nerve fibers, averaging 14 micrometers in diameter; these fibers branch many times after they enter the muscle and innervate the large skeletal muscle fibers. Stimulation of a single alpha nerve fiber excites anywhere from three to several hundred skeletal muscle fibers, which are collectively called the motor unit.
Gamma Motor Neurons.
Along with the alpha motor neurons, about one half as many much smaller gamma motor neurons are located in the spinal cord anterior horns. These gamma motor neurons transmit impulses through much smaller type A gamma motor nerve fibers, averaging 5 micrometers in diameter, which go to small, special skeletal muscle fibers called intrafusal fibers. These fibers constitute the middle of the muscle spindle,which helps control basic muscle “tone.Interneurons.
Interneurons are present in all areas of the cord gray matter in the dorsal horns, the anterior horns, and the intermediate areas between them. These cells are about 30 times as numerous as the anterior motor neurons. They are small and highly excitable, often exhibiting spontaneous activity and capable of firing as rapidly as 1500 times per second. They have many interconnections with one another, and many of them also synapse directly with the anterior motor neurons. The interconnections among the interneurons and anterior motor neurons are responsible for most of the integrative functions of the spinal cord.Renshaw Cell Inhibitory System.
Also located in the anterior horns of the spinal cord, in close association with the motorneurons, are a large number of small neurons called Renshaw cells.Almost immediately after the anterior motor neuron axon leaves the body of the neuron, collateral branches from the axon pass to adjacent Renshaw cells.
These are inhibitory cells that transmit inhibitory signals to the surrounding motor neurons (lateral inhibition). The motor system uses this lateral inhibition to focus, or sharpen motor signals, suppressing the tendency for signals to spread laterally.
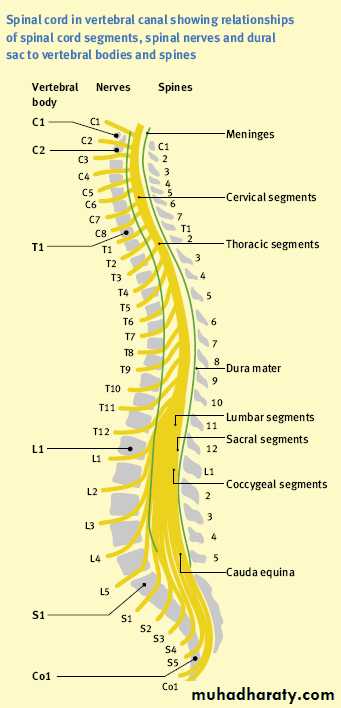
Fig. 14-1 Spinal cord organization for sensory, motor and autonomic functions
Spinal Cord Injuries:
Spinal cord injuries are classified 'depending on the completeness of the lesion into two main types, complete and incomplete lesions.
a)) Incomplete lesions is further subdivided into:
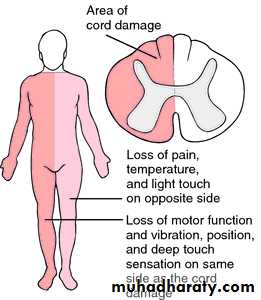
1. Hemi-section of the spinal cord
(Brown-Séquard Syndrome)
This is a unilateral transverse lesion in the spinal cord that interrupts the continuity of both ascending and descending tracts at only one half. Such lesion causes the following symptoms:
Paralysis of the muscles of the UMNL type on the same side due to interruption of descending tracts.
Contralateral analgesia and athermia (loss of pain, heat, and cold sensations) due to interruption of the ascending fibers of the lateral spinothalamic tract of the opposite side.
Ipsilateral loss of the kinesthetic position, vibration, discrete localization and the two-point discrimination sensations due to interruption of the dorsal columns.
Crude touch sensation is diminished but not lost on both sidesm because it is transmitted by both ventral spinothalamic tract as well as by the dorsal column.
Fig. 14-2 Brown sequard syndrome
2. Anterior cord syndrome:This is when the damage is towards the front of the spinal cord, this can leave a person with the loss or impaired ability to sense pain, temperature and touch sensations below their level of injury. Pressure and joint sensation may be preserved.
3. Posterior cord syndrome:
This is when the damage is towards the back of the spinal cord. This type of injury may leave the person with good muscle power, pain and temperature sensation, however they may experience difficulty in coordinating movement of their limbs.
4. Central cord syndrome:
This is when the damage is in the centre of the spinal cord. This typically results in the loss of function in the arms, but some leg movement may be preserved.
B. Complete Transverse Section
This is fatal if it is above the origin of the phrenic nerve, however at lower levels, patients pass in three stages:
Spinal shock
Recovery of spinal reflex activity.Failure of spinal reflex activity.
a)) Spinal shock:
Spinal shock is due to sudden withdrawal of supraspinal facilitation on the spinal alpha motor neurons (particularly discharges transmitted through reticulospinal,vestibulospinal, and corticospinal tracts).The duration of the shock varies directly with the degree of development of the cerebral cortex. In human being it lasts from 2-6 weeks.The management of spinal shock stage is tried to prevent any complications which can delays the recovery of spinal reflex (bladder catheterization, prevention of pressure sores and adequate nutrition.
b)) Recovery of spinal reflex activity:
After few hours to few weeks, the spinal neurons gradually regain their excitability (this is a natural characteristic of the neurons anywhere in the CNS). In human being, return is delayed from several weeks and occasionally never complete. Sometimes, recovery is excessive with resultant hyper excitability of some or all cord functions.Release of the spinal centers from the inhibitory control of the higher center (a release phenomenon), denervation hypersensitivity or growth of new collaterals could be the possible mechanism of spinal reflex recovery.
c)) Failure of spinal reflex activity:
Bad management during the recovery stage will lead to failure of spinal reflex functions.Complication of Cord Transection
They develop negative nitrogen balance and catabolize large amounts of body proteins.Pressure sores due to compression of skin circulation by the body weight.
Hypercalcemia that lead to hypercalciuria and calcium stones.
The stones in combination with neuropathic bladder cause urine stasis which predispose to urinary infection.
Death from septicemia and uremia.
Responses in Chronic Spinal Humans
In chronically quadriplegic humans, there is certain complications originating from long standing spinal cord injuries:
Threshold of withdrawal reflex is low (minor noxious stimuli may cause not only prolonged withdrawal of one extremity but marked flexion-extension patterns in the other 3 limbs).
Repeated flexion movements occur for prolonged periods and contractures of flexor muscles develop.
Stretch reflexes are hyperactive.
Reflex contractions of the full UB and rectum occur. The hyperactive UB reflexes keep it in a shrunken state leading to hypertrophy and fibrosis of its wall.
Blood pressure is generally normal at rest, but wide swings in the pressure are common as the feedback regulation by baroreceptor reflexes is absent.
Bouts of sweating and blanching of the skin.
Genital manipulation in males produces erection and even ejaculation.
The Mass reflex (strong nociceptive stimulus to skin or excessive filling of a viscous (over distention of the UB or gut) can cause massive discharge of large portions of the cord. The effects are:
Major part of the body goes into strong flexor spasm
The colon and UB are likely to evacuate
The blood pressure rises to a systolic pressure of > 200 mmHg
Profuse sweating of large areas of the body.
Upper and Lower Motor Neurons
Lesions of the lower motor neurons (spinal and cranial motor neurons that directly innervate the muscles) are associated with flaccid paralysis muscular atrophy and absence of the reflex responses.Upper motor neuron lesions (the neurons in the brain and spinal cord that activate the motor neurons are destroyed) are associated with spastic paralysis and hyperactive stretch reflexes in the absence of the muscle atrophy. It is of 3 types:
Lesions in the extrapyramidal posture regulating pathway cause spastic paralysis.
Lesions limited to the pyramidal tracts causes UMNL type below the level of the lesion. However, the side effected and the extent of paralysis depends on the site of the lesion.Cerebellar lesions cause incoordination.
Important note:
Crossed hemiplegia is contralateral hemiplegia (UMNL) plus ipsilateral paralysis of the cranial nerves (LMNL) and it is caused by lesion of the pyramidal tract in the brain stem.