Physiology Dr. Hanan Luay Lec 1
Endocrine andReproductive physiology
Objectives:
1-What do the body activities controlled by?
2-Define hormones? Describe their chemical structure?
3- Explain the mechanisms of hormone secretion and action?
4-Discuss the control of hormone secretion?
Coordination of body functions:
The activities of the cells, tissues, and organs of the body are coordinated by the interplay of several types of chemical messenger systems, but specifically the control is by either the nervous system or the hormonal or endocrine system through:
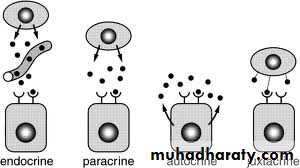
1. Neurotransmitters are released by axon terminals of neurons into the synaptic junctions and act locally to control nerve cell functions.
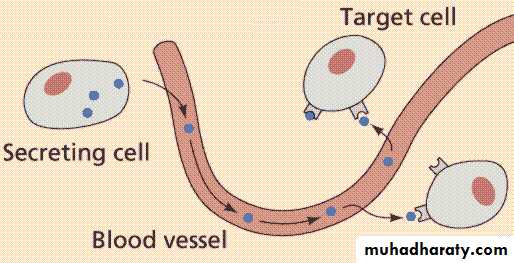
2. Endocrine hormones are released by glands or specialized cells into the circulating blood and influence the function of cells at another location in the body.
3. Neuroendocrine hormones are secreted by neurons into the circulating blood and influence the function of cells at another location in the body.
4. There is what is called Paracrine effect which is secretion by cells into the extracellular fluid and affect neighboring cells of a different type, and Autocrines are secreted by cells into the extracellular fluid and affect the function of the same cells that produced them by binding to cell surface receptors. Also there are Cytokines (e.g interleukins) are peptides secreted by cells into the extracellular fluid and can function as autocrines, paracrines, or endocrine hormones.
The endocrine hormones are carried by the circulatory system to cells throughout the body, including the nervous system in some cases, where they bind with receptors and initiate many reactions. They either affect:
1- Many different types of cells of the body; for example, growth hormone(from the anterior pituitary gland) causes growth in most parts of the body, and thyroxine(from the thyroid gland) increases the rate of many chemical reactions in almost all the body’s cells.
2- Only specific target tissues, because only these tissues have receptors for the hormone. For example, adrenocorticotropic hormone (ACTH) from the anterior pituitary gland specifically stimulates the adrenal cortex, causing it to secrete adrenocortical hormones, and the ovarian hormones have specific effects on the female sex organs as well as on the secondary sexual characteristics of the female body.
Endocrine glands are ductless glands, they release their products direct to the circulation and their products are called hormones.
Hormones are chemical substances produced by glands or neurosecretory cells (so not all the hormones are secreted by endocrine glands e.g. GIT hormones) released into the blood in response to a specific stimulus.
(Guyton, 2011)
The multiple hormone systems play a key role in regulating almost all body functions, including metabolism, growth and development, water and electrolyte balance, reproduction, and behavior.
After the secretion of the hormones, small fraction will circulate freely and the major part will bind to plasma proteins which act as:
1- Storage site, release the hormones on need.
2- Buffer mechanism: to minimize the effect of particular hormones.
Chemical structure of hormones;There are three general classes of hormones:
1. Proteins and polypeptides, including hormones secreted by the anterior and posterior pituitary gland, the pancreas (insulin and glucagon), the parathyroid hormone, and others.
2. Steroids secreted by the adrenal cortex (cortisol and aldosterone), the ovaries (estrogen and progesterone), the testes (testosterone), and the placenta (estrogen and progesterone).
3. Derivatives of the amino acid tyrosine, secreted by the thyroid (thyroxin and triiodothyronine) and the adrenal medullae (epinephrine and norepinephrine). There are no known polysaccharides or nucleic acid hormones.
Onset of Hormone Secretion
Some hormones, such as norepinephrine and epinephrine, are secreted within seconds after the gland is stimulated, and they may develop full action within another few seconds to minutes; the actions of other hormones, such as thyroxin or growth hormone, may require months for full effect. Thus, each of the different hormones has its own characteristic onset and duration of action.Control of hormonal secretion:
A-Feedback mechanism:
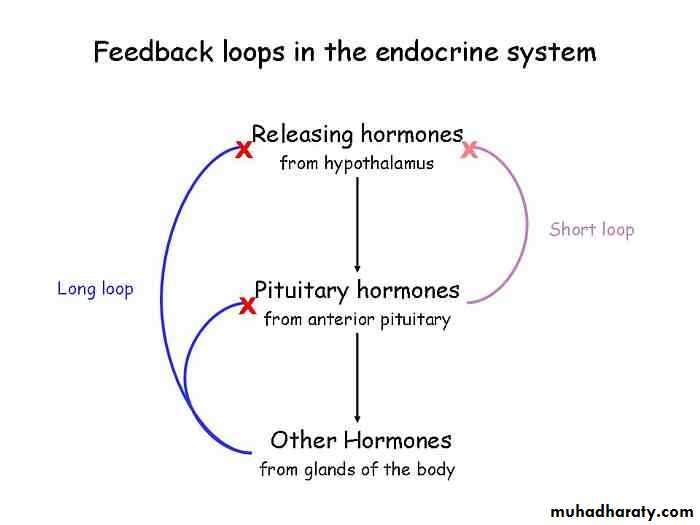
1-Negative feedback mechanism:
a- Direct negative feedback:
It relates the rate of release of the hormone to the blood concentration of that substance. After a stimulus causes release of the hormone, conditions or products resulting from the action of the hormone tend to suppress its further release, to prevent oversecretion of the hormone or overactivity at the target tissue.
e.g:
ACTH (adrenocorticotrophic hormone): synthesized and released from the anterior lobe of the pituitary gland, secreted directly to the circulation and carried by the blood to affect the target organ, the suprarenal cortex, to secret cortisol. as the level of cortisol increased in the circulation it feeds back to the anterior pituitary and inhibit the release of ACTH ,so no more stimulation of the adrenal cortex happen → no more cortisol secreted.
b- Indirect negative feedback:
This type will act when the nervous system (Hypothalamus) is involved in the process:e.g: CRH (corticotrophin releasing hormone) released from the hypothalamus transported to the anterior lobe of pituitary; it stimulates the synthesis and release of ACTH. As the level of cortisol increase, it feeds back to the hypothalamus and inhibit the release of ACTH which inhibits the secretion of cortisol. So ACTH affects the release of cortisol via CRH (indirect feedback).
c- Short negative feedback:
The hypothalamus controls the release of adenohypophysial hormones (anterior pituitary) by secreting releasing substances ,some of these adenohypophysial hormones have feedback effect on the release of hypothalamic hormones ,this is called short feedback loop e.g.:
GHRH (growth hormone releasing hormone, secreted from the hypothalamus and carried by blood (portal system) to the adenohypophysis, stimulates the synthesis and secretion of GH (growth hormone) which affect almost all body tissues and there is no hormone released in response to it(no target gland) . If GH increases in the circulation, it feeds back to the hypothalamus and inhibits the release of GHRH, followed by inhibition of GH secretion, so called short feedback because the distance between the hypothalamus and the pituitary is short.
(Guyton, 2011)
2-Positive feedback mechanism:
Means increase in the release of particular in hormone from a concerned gland in response to the increase in the increase chemical substance.e.g. FSH (follicular stimulating hormone) secreted by the pituitary gland, circulates in the blood to affect the ovary in the female and stimulates the development of ovarian follicle which will secrete estrogen (female sex hormone), as estrogen increases, it feeds back to the anterior pituitary, stimulates the release of LH and more FSH (LH and FSH responsible for the final maturation of the ovarian follicle).This happens in the first half of the menstrual cycle. But after ovulation ,the remnant of the released follicle is converted to corpus luteum which will secret estrogen and progesterone which will feedback to the anterior pituitary and inhibit the release of LH and FSH ,so no more maintenance of corpus luteum and no maintenance of the endometrium → shedding of it → menstrual cycle.
B- Influence of the nervous system;
Means the activity of the supplying nerve to the endocrine glands.
The glands that are primarily controlled by the nervous system are:
Adrenal medulla. 2- Posterior lobe of the pituitary gland.
There is what is called Cyclical Variations occur in hormone release, which are periodic variations in hormone release that are influenced by seasonal changes, various stages of development and aging, the diurnal (daily) cycle, and sleep. For example, the secretion of growth hormone is markedly increased during the early period of sleep but is reduced during the later stages of sleep. In many cases, these are due to changes in activity of neural pathways involved in controlling hormone release.
Mechanism of action of the hormones:
The first step of a hormone’s action is to bind to specific receptors at the target cell, after dissociation of the binding protein. Cells that lack receptors for the hormones do not respond. Each receptor is usually highly specific for a single hormone; this determines the type of hormone that will act on a particular tissue. The shape of the receptor is exactly the same of that hormone, therefore if these receptors are deformed or absent, the effect of the hormones can't be produced, whatever the level of the hormone is (All the receptors in a particular gland are the same shape) e.g feminizing testis, although the male has normal testes can secret enough testosterone, but there are no receptors for it so there is absence of secondary sex characteristics and organs.Another example, nephrogenic diabetes insipidis, here we have ADH (antidiurtic hormone) secreted by the posterior lobe of the pituitary gland and acts on the kidney to increase the permeability of the cell membrane to water leading to reabsorption of it and reduces the volume of urine excreted to the outside, but in the absences of ADH receptors we will have increase urination.
When the hormone combines with its receptor, this usually initiates a cascade of reactions in the cell.
2-Binding of the hormone will cause activation of Adenyl cyclase which causes immediate conversion of small amounts of ATP to cyclic AMP (3,5, adenosine monophosphate)-cAMP, which is sometimes called intracellular hormonal mediator and is called the second messenger, because the hormone mediation is the first messenger ,this will activates cAMP dependent proteins and
3- bring above various action, these are:
Increase in the permeability of the cellular membrane, influencing the formation of special enzymes in the cells, or production of other hormones.
The locations for the different types of hormone receptors are generally the following:
1. In or on the surface of the cell membrane. The membrane receptors are specific mostly for the protein, peptide, and catecholamine hormones.2. In the cell cytoplasm. The primary receptors for the different steroid hormones are found mainly in the cytoplasm.
3. In the cell nucleus. The receptors for the thyroid hormones are found in the nucleus and are believed to be located in direct association with one or more of the chromosomes.
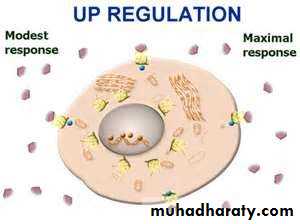
The regulation of the number and sensitivity of hormone receptors
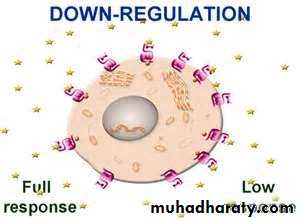
The number of receptors in a target cell usually does not remain constant from day to day, or even from minute to minute. The receptor proteins themselves are often inactivated or destroyed during the course of their function, and at other times they are reactivated or new ones are manufactured. For instance, increased hormone concentration and increased binding with its target cell receptors sometimes cause the number of active receptors to decrease. This is called down-regulation of the receptors. In this case, receptor down-regulation decreases the target tissue’s responsiveness to the hormone.Some hormones cause up-regulation of receptors; that is, the stimulating hormone induces greater than normal formation of receptor. When this occurs, the target tissue becomes progressively more sensitive to the stimulating effects of the hormone.
(www.quizlet.com)
Lec 2
Objectives:
Describe the relation between the hypothalamus and pituitary gland?
Enumerate the hormones and factors released from the hypothalamus and pituitary?
Discuss the control of ADH secretion?
How does Oxytocin act on its receptors?
Pituitary Hormones and Their Control by the Hypothalamus
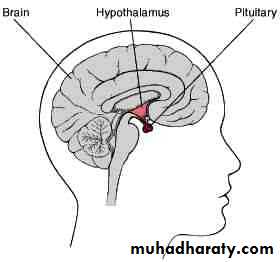
The hypothalamus is composed of nervous tissue situated below the thalamus and it is surrounded by part of the third ventricle with afferent and efferent fibers connecting it to the rest of CNS, the hypothalamus is bounded anteriorly by optic chiasma (decussation of nasal fibers of optic nerve). Posteriorly by the mammilary bodies .laterally by the sulci formed with the temporal lobes .The rounded base of the hypothalamus is called tuber cinerum. The central part of it called median eminence, from which descend a stalk which connect the pituitary to the hypothalamus along this stalk the hypothalamo-hypophysial portal system runs.
The synthesis and storage of chemical substances takes place within a specific nerve cells, the secretion of these substances takes place in close association with the blood vessels, so we can apply the term neurosecretion and the term hormone on them.
Most of the hypothalamic nuclei end on the median eminence with the exception of supraoptic and paraventricular nuclei ,their axon terminate in the posterior lobe of the pituitary gland while the neurosecretion in the median eminence are released to the portal system to the adenohypophysis. Each neurosecretion acts on particular adenohypophysial cell to influence the release of a specific adenohypophysial hormone. So the adenohypophysial hormones are influenced by releasing or inhibiting factors and hormones (if we know the chemical structure we call it hormone if not we call it factor) and these are:
1-Thyrtrophin releasing hormone (TRH).
2-Corticotrophin releasing hormone (CRH).stimulates the synthesis and release of ACTH from the anterior lobe of the pituitary gland to stimulate the adrenal cortex.
3-Somatostatin or growth hormone inhibiting hormone (GHIH).
4-Somatrophin releasing hormone or growth hormone releasing hormone (GHRH), stimulates the synthesis and release of GH from the anterior lobe of the pituitary gland .GH has no target tissue to affect but it affects all tissues of the body.
5-Melanocyte stimulating hormone releasing hormone. Present mainly in animals.
6-Gonadotrophin releasing hormone (GnRH) (stimulate the release of FSH and LH).
7-Prolactin inhibiting factor (PIH) (no milk secretion in normal conditions because of this factor).
The release of any releasing or inhibiting hormones from the hypothalamus is controlled by the nervous impulses and partly by the feedback mechanism.
The pituitary gland:
It lies in the sellaturcica, a bony cavity at the base of the brain (depression in the sphenoid bone) when there is enlargement of the gland as a result of a tumor there is widening of the sellaturcica, in the X ray.
It is located beneath the hypothalamus and connected to it by the pituitary (or hypophysial) stalk.
The pituitary gland is a round or ovoid structure .It weighs about 0.5 gm this weight increases during pregnancy (because increase in gonadotropin hormones)
Physiologically, the pituitary gland is divisible into two distinct portions: the anterior pituitary, also known as the adenohypophysis, and the posterior pituitary, also known as the neurohypophysis. Embryologically, the two portions of the pituitary originate from different sources:1- the anterior pituitary from Rathke’s pouch, which is an embryonic invagination of the pharyngeal epithelium (or the ectoderm of the roof of the primitive mouth), and because it has a glandular structure it is called adenohypophysis.2- the posterior pituitary from a neural tissue outgrowth from the hypothalamus(or from the base of the brain),and the origin of it from neural tissue explains the presence of large numbers of glial-type cells in this gland.
The hormones of the anterior pituitary:
• Growth hormone
• Adrenocorticotropin-ACTH (corticotrophin).
• Thyroid-stimulating hormone-TSH (thyrotropin).
• Prolactin promotes mammary gland development and milk production.
• Two gonadotropic hormones, follicle-stimulating hormone-FSHandluteinizing hormone-LH.
The two hormones secreted by the posterior pituitary play other roles
.Antidiuretic hormone-ADH(also called vasopressin).
• Oxytocin.
Secretion from the posterior pituitary is controlled by nerve signals that originate in the hypothalamus and terminate in the posterior pituitary. In contrast, secretion by the anterior pituitary is controlled by hormones called hypothalamic releasing and hypothalamic inhibitory hormones (or factors) secreted within the hypothalamus itself and then conducted, to the anterior pituitary through minute blood vessels called hypothalamic-hypophysialportal vessels. In the anterior pituitary, these releasing and inhibitory hormones act on the glandular cells to control their secretion.
Hormones of the posterior lobe of the pituitary gland
ADH (ANTIDIURETIC HORMONE) or VasopressinADH is formed primarily in the supraoptic nuclei and to a lesser extent the paraventricular nucleus, in the hypothalamus and carried along the axons to be stored in the posterior pituitary gland.
(Guyton, 2011)
It exerts its action on the kidney, it acts on the distal convoluted tubules and collecting ducts, it increases the permeability of the cellular membrane to water so water diffuses to the surrounding medullary tissues down its osmotic gradient. As a result we have reduction in the volume of urine excreted to the outside and it will become more concentrated. Conversely in the absence of ADH, the collecting tubules and ducts become almost impermeable to water, which prevents significant reabsorption of water and therefore allows extreme loss of water into the urine, also causing extreme dilution of the urine.This hormone is called Vasopressin also because if it reaches above the physiological concentration, it will cause vasoconstriction of arteriols throughout the body→ increase the blood pressure.
Control of hormone secretion;
1-Plasma osmolarity:
If there is reduction in the plasma osmolarity (e.g. overhydration) → inhibition of ADH secretion → inhibition of reabsorption from the distal convoluted tubules and collecting ducts → large amount of water excreted to the outside.
If we have increase in the osmolarity (e.g. dehydration like vomiting, diarrhea and burns) → stimulation of ADH secretion →increase reabsorption and retention of water thus plasma osmolarity returns back to normal.
There are modified neuron receptors called osmoreceptors in or near the hypothalamus (close to supraoptic nuclei).
When the extracellular fluid becomes too concentrated, fluid is pulled by osmosis out of the osmoreceptor cell, decreasing its size and initiating appropriate nerve signals in the hypothalamus to cause additional ADH secretion. Conversely, when the extracellular fluid becomes too dilute, water moves by osmosis in the opposite direction, into the cell, and this decreases the signal for ADH secretion.
2-Blood volume:
One of the stimuli for causing intense ADH secretion is decreased blood volume e.g blood loss (heamorhage). This occurs especially strongly when the blood volume decreases 15 to 25 per cent or more; the secretory rate then sometimes rises to as high as 50 times normal. The cause of this is the following. The atria have stretch receptors (sometimes called volume or low pressure receptors) that are excited by overfilling. When excited, they send signals to the brain to inhibit ADH secretion. Conversely, when the receptors are unexcited as a result of underfilling, the opposite occurs, with greatly increased ADH secretion. Decreased stretch of the baroreceptors of the carotid, aortic, and pulmonary regions also stimulates ADH secretion.
3-Variety of stimuli:
Drugs like morphine, pethedine (tranquilizers), they act centrally and stimulate the release of ADH→ increase of the reabsorption of water and decrease in volume of water excreted to the outside. Both tranqulizers and alcohol act centrally on the supraoptic nucleus.
Alcohol inhibits the secretion of ADH and increase in urination (so drunk people urinate a lot).
Clinical conditions result from disturbances in ADH secretion:
For example, after car accidents we have decrease in secretion of ADH and as a result we have increase urination called polyuria, the urine is of low specific gravity. And as a result of excessive urination, we have excessive drinking of water called polydepsia. This condition is called diabetes insipidus (D.I.).We have 2 types of D.I.:
1-Central D.I.:
When we have tumor of the pituitary gland (craneopharynenoma) → decrease ADH secretion.
2-Nephrogenic D.I.;
Congenital absence of the ADH receptors in the kidney, so high level of ADH but no response (because the feedback mechanism depends on the degree of activity of the target organ, so if the target responds poorly the gland continues secreting the hormone).
We must differentiate between DI. and D.M. (diabetes mellitus in which also there is polyuria and polydepsia ,but the specific gravity of urine in DM is higher because of the presence of glucose.
Oxytocine:
Oxytocin is formed primarily in the paraventricular nuclei in the hypothalamus, carried along the axons to be stored in the posterior pituitary, it is present in male and female but its exact physiological action is not obvious in male. Its action in females is on both 1- the uterus 2- the mammary gland.1-Effect on the uterus;
It causes contraction of the uterus at labour .It aids in the expulsion of fetus and placenta; it increases to the peak value during labour. HOW?The fetus moves downward into the birth canal →dilatation of the cervix→stimulation of stretch receptors (in addition to the stretch receptors of the vagina), send impulses to the spinal cord and paraventricular nuclei, release oxytocin.
Progesterone usually inhibits the sensitivity of the uterus to oxytocin, but estrogen increases the sensitivity of the uterus to oxytocin.
Oxytocin is used medically to induce labour in women passing their expected date of delivery, so it is given intravenously in small amounts (because if the dose is high the uterus may rupture).
2-Effect on the mammary gland:
In lactation, oxytocin causes milk to be expressed from the alveoli into the ducts of the breast so that the baby can obtain it by suckling, so oxytocin causes ejection of milk not secretion of it, because the secretion is under the effect of prolactin.. This mechanism works as follows: The suckling stimulus on the nipple of the breast causes signals to be transmitted from the touch receptors in the areola around the nipples through sensory nerves to the oxytocin neurons in the paraventricular and supraoptic nuclei in the hypothalamus, which causes release of oxytocin by the posterior pituitary gland (it is a neurohormonal reflex). The oxytocin is then carried by the blood to the breasts, where it causes contraction of myoepithelial cells that lie outside of and form a latticework surrounding the alveoli of the mammary glands. In less than a minute after the beginning of suckling, milk begins to flow. This mechanism is called milk letdown or milk ejection.
Also the sound or sight of the baby can stimulate the release of milk, while stress inhibits the release of oxytocin, so the flow of milk is reduced.
It is released also during the process of sexual intercourse ,so stimulation of touch receptors in the vulva and vagina send impulses to the spinal cord →release of oxytocin →causes rhythmical contraction of the uterus which suck the sperms upwards to the uterine cavity and then to the fallopian tube for the process of fertilization.
Oxytocin as a hormone of love and trust.
Oxytocin evokes feelings of contentment, reductions in anxiety, and feelings of calmness and security
This suggests oxytocin may be important for the inhibition of the brain regions associated with behavioral control, fear, and anxiety.
Oxytocin also functions to protect against stress. Increasing trust and reducing fear.
Lec 3
Objectives:How do the anterior pituitary hormones be classified?
What are the effects of Growth hormone on metabolism and growth?
What are the effects of the disturbance in growth hormone secretion?
Anterior lobe of the pituitary gland:
It is a vascular organ .It receives its blood supply from superior and inferior hypophysial arteries. The superior arises from the internal carotid artery then it enters the median eminence, then break into numerous branches and capillary loops called the primary plexus then they reconverge to form parallel venules that descend along the stalk (the long portal vessels), descend along the stalk and penetrate the adenohypophysis and end on the sinusoids bathing the adenohypophysis.Usually, there is one cell type for each major hormone formed in the anterior pituitary gland. With special stains attached to high-affinity antibodies that bind with the distinctive hormones, at least five cell types can be differentiated. These five cell types are:
1. Somatotropes—human growth hormone (hGH), 50% of the anterior lobe.
2. Corticotropes—adrenocorticotropin (ACTH)
3. Thyrotropes—thyroid-stimulating hormone (TSH)
4. Gonadotropes—gonadotropic hormones, which include both luteinizing hormone (LH) and follicle stimulating hormone (FSH)
5. Lactotropes—prolactin (PRL), the number of these cells increase during pregnancy due to estrogen action.
Somatotropes stain strongly with acid dyes and are therefore called acidophils. Thus, pituitary tumors that secrete large quantities of human growth hormone are called acidophilic tumors. There are also basophilic cells and chromophobe cells, and this is the old classification of the cells.
We can classify the hormones of the anterior pituitary also into:
Glycoproteins: TSH, LH, FSH and Human Chorionic Gonadotropins(HCG) secreted during pregnancy from the placenta. Composed of 2 peptide chains α and β chains. Alpha chains are similar in all but beta is different so their action depends on beta chains.
Somatomammotrophins: (single peptide) prolactin and growth hormone, Human Placental Lactogen(HPL).
ACTH related peptide. These close related peptides are derived from parent compound known as (Big ACTH) which has120- 130 amino acid residues. This undergoes enzymatic cleavage → large fragment (β lipoprotein), this gives rise to smaller peptides, the most important of which is ACTH.
ACTH synthesized in basophilic cells and composed of 39 amino acids. The activity of ACTH resides in the first 24 a.a. (a property used in the synthesis of the synthetic ACTH).
The first 13 a.a resembles that of β –melanocyte stimulating hormone; therefore if we have increment of ACTH above the physiological level, we have increase in the pigmentation of the skin.
Other important fragment of β lipotrophes is β endorphin which is present in the brain and GIT and acts as a neurotransmitter (have analgesic property).
If we take the hormones of the first group:
TSH (thyroid stimulating hormone):
TSH is a glycoprotein synthesized and stored in the thyrotroph cells (basophilic cells), its primary action is on the thyroid gland stimulate the synthesis and release of T3 and T4 after several mechanisms:1-Stimulation of iodide pumps in the cell membranes which transport the iodine from the blood to the cell against the electrochemical gradient.
2-It stimulates the synthesis of thyroid storage protein which is thyroglobulin.
3-Stimulates the synthesis of T3 and T 4.
4-Stimulates the release of T3 and T4 from the thyroglobulin complex.
5-If there is oversecretion of TSH there is enlargement of the thyroid gland (goiter).
FSH (follicle stimulating hormone) and LH (lutenizing hormone):
They are glycoproteins synthesized by gonadotrophs (basophilics).They are responsible for development of the ovarian follicles and ovulation. The production of LHRH (lutenizing hormone releasing hormone) is inhibited by estrogen and to lesser extent by progesterone; this phenomenon is used in the contraceptive pills, which contains combination of both estrogen and progesterone and some contain only progesterone. While LHRH is stimulated by estrogen deficiency, so we can use antiestrogenic drugs like clomid.In male FSH stimulates the development of sperms i.e responsible for the process of spermatogenesis, during this process, we have the release of peptide called inhibin ,which feeds back and inhibit the release of FSH.
LH in male is called interstitial cell stimulating hormone (ICSH), it stimulates the interstitial cells to synthesize and release Testosterone. As the level of testosterone increase, we have inhibition of LH secretion.
Growth hormone:
In contrast to other hormones, does not function through target gland but exerts its effects directly on all or almost all tissues of the body.The other name is somatotropin; it is composed of 191 a.a. It shows species differences, so that of human is different from that of the animals.
It exerts an effect on metabolism and tissue growth. The effect on metabolism is a direct effect but on growth is indirect via a peptide called somatomedin.
It is synthesized in the liver and to lesser extent by the kidney under the effect of growth hormone.
GH stimulates every tissue capable of growing by increasing the size of cells (hypertrophy),and increase the number of cells by mitosis also stimulate differentiation of cells e.g chondrocytes→ osteocytes and early muscle cells.
Aside from its general effect in causing growth, growth hormone has multiple specific metabolic effects.
Effect of GH on metabolism:
1-Effect on proteins:
GH increase protein synthesis and tissue growth
1- Enhancement of Amino Acid Transport through the Cell Membranes: it directly enhances transport of most amino acids through the cell membranes to the interior of the cells. This increases the amino acid concentrations in the cells.
2-Enhancement of RNA translation to cause protein synthesis by the ribosomes.
3-Increased nuclear transcription of DNA to form RNA.
4-Decreased catabolism of protein and amino acids.
5-Decrease urinary urea nitrogen.
6-The net effect is positive nitrogen balance.
2-Effect on fat metabolism
Growth hormone has a specific effect in causing the release of fatty acids from adipose tissue and therefore, increasing the concentration of fatty acids in the body fluids i.e stimulates the breakdown of stored fat in adipose tissues, so we have increase in free fatty acids in the blood and increase in utilization of fat which promote a source of energy for tissues, and as a result of that we have increase in keton bodies formation by the liver that’s why it is considered as ketogenic hormone.Note: The aged appearance seems to result mainly from decreased protein deposition in most tissues of the body and increased fat deposition in its place, increased wrinkling of the skin and diminished muscle mass and strength.
3- Effect on carbohydrates:
Growth hormone causes multiple effects on carbohydrate metabolism, including (1) decreased glucose uptake in tissues such as skeletal muscle and fat, (2) increased glucose production by the liver, and (3) increased insulin secretion. This will cause increase in blood glucose concentration. So it is considered as a diabetogenic hormone.4- Effect on electrolytes:
It decreases the elimination of all electrolytes in the body. It increases the absorption of calcium by the intestine. Na and K excretion through the kidney is reduced .These electrolytes are diverted from the blood to the growing tissue, so their levels in blood and urine decrease.5-Effect on growth:
Growth is an organized addition of new tissue result in increase size of the body. The effect of growth hormone is throughincreased deposition of protein by the chondrocytic and osteogenic cells that cause bone growth (deposition of cartilage at the epiphysial plate at the end of the long bones, (2) increased rate of reproduction of these cells, and (3) a specific effect of converting chondrocytes into osteogenic cells, thus causing deposition of new bone i.e stimulate osteoblast cells.
GH stimulates a second humeral factor which acts on the cartilage called somatomedine which is synthesized in the liver and to lesser extent in the kidney under the effect of GH. And GH exerts its effect through this factor. Many of the somatomedin effects on growth are similar to the effects of insulin on growth. Therefore, the somatomedins are also called insulin-like growth factors (IGFs).
Regulation of Growth Hormone Secretion;
After adolescence, secretion decreases slowly with aging, finally falling to about 25 per cent of the adolescent level in very old age. Growth hormone is secreted in a pulsatile pattern, increasing and decreasing.
Factors affecting the release of GH:
1-State of nutrition ;( a) Starvation, especially with severe protein deficiency (under a chronic conditions is a good stimulator); (b) Hypoglycemia (under acute conditions, it is a good stimulator. Note that insulin and carbohydrates are necessary for GH action, so chronic lack of them causes lack of GH action).
(c) Low concentration of fatty acids in the blood.
2-Stress: exercise; excitement; and trauma.
3-Deep sleep: GH increases during the first 2 hours of deep sleep.
4-Feedback mechanism:
GHRH stimulated by hypoglycemia, emotion, stress, trauma, dopamine, serotonin.
(Guyton,2011)
GHRH passes through the hypothalamo-hypophysial portal system to adenohypophysis, bind with receptors in the cell membrane of somatotroph cells leading to:
Immediate response to cAMP and have release of GH via Calcium enter the cell.
Late action of cAMP, stimulate GH synthesis.
GHIH (also called somatostatine) stimulated by hyperglycemia, increase free fatty acids, aging, obesity, exogenous injection of humeral GH.
The level of GH increases in the circulation→ feedback to the hypothalamus→ decrease the release of GHRH → decrease the release of GH (short loop negative feedback).
Abnormalities of Growth Hormone Secretion:
A-Reduction in GH secretion:1-Panhypopituitarism: as in case of tumor decreasing all the pituitary hormones.
2-Dwarfism. Results from deficiency of GH secretion during childhood. All theparts of the body develop in appropriate proportion to one another, but the rate of development is greatly decreased.
B-Increase in GH secretion:
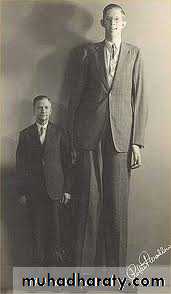
1-Gigantism. Sometimes acidophilic tumors occur in the pituitary gland. As a result, large quantities of growth hormone are produced. All body tissues grow rapidly, including the bones. If the condition occurs before adolescence, before the epiphyses of the long bones have become fused with the shafts, height increases so that the person becomes a giant. The giant ordinarily has hyperglycemia. Consequently, full-blown diabetes mellitus eventually develops.
(www.thetallestman.com)
2-Acromegaly.If an acidophilic tumor occurs after adolescence— that is, after the epiphyses of the long bones have fused with the shafts—the person cannot grow taller, but the bones can become thicker and the soft tissues can continue to grow. Enlargement is especially marked in the bones of the hands and feet and in the membranous bones, including the cranium, nose, bosses on the forehead, supraorbital ridges, lower jawbone, and portions of the vertebrae, because their growth does not cease at adolescence. Many soft tissue organs, such as the tongue, the liver, and especially the kidneys, become greatly enlarged.
(Guyton,2011)
The concentration of GH in different ages
5 to 20 years 6ng/ml
20 to 40 years 3ng/ml
40 to 70 years 1.6ng/ml
Prolactin hormone:
It is secreted by lactotroph cells. In female it causes milk secretion after estrogen and progesterone priming effect. During pregnancy there is no prolactin secretion because of the presence of estrogen and progesterone secreted by the placenta in addition to prolactin inhibiting factor. After delivery the effect of estrogen and progesterone will be gone and no suppression of prolactin so milk secretion will occur. Suckling by the baby produces a prompt increase in secretion, but the magnitude of this rise gradually declines after a woman has been nursing for more than 3 months.Sometimes we have increase in prolactin in pathological way (hyperprolctinemia) which leads to inhibition of LH and FSH → estrogen and progesterone inhibition → amenorrhea (no menstrual cycle).
In case of dead fetus, we don’t need milk so we give antiprolactin drugs (parlodel).So we have both physiological prolactin increase after delivery and pathological increase which needs treatment.
Lec 4
Objectives:
What are the hormones secreted from thyroid gland?
Describe the physiological actions of thyroid hormones?
3-What are the physiological effects of hypothyroidism and hyperthyroidism?
Thyroid gland:
(Guyton,2011)The thyroid gland, located immediately below the larynx on each side of and anterior to the trachea, consisted of two lobes connected by the isthmus.
The thyroid secretes two major hormones, thyroxine (T4) or tetraiodothyronin and triiodothyronine, (T3), these concerned with metabolism. The thyroid gland also secretes calcitonin, an important hormone for calcium metabolism.
Thyroid gland has got a characteristic feature in trapping iodide from the circulation. This feature is also present in salivary gland, intestinal mucosa, mammary gland, ciliary body and choroid plexuses, but cannot synthesize thyroid hormone.
1-Iodide Pump (Iodide Trapping):
The first stage in the formation of thyroid hormones is transport of iodides from the blood into the thyroid glandular cells and follicles. The basal membrane of the thyroid cell has the specific ability to pump the iodide actively to the interior of the cell. This is called iodide trapping. In a normal gland, the iodide pump concentrates the iodide to about 30 times its concentration in the blood (may increase to 250 times in overactivity of the gland).The rate of iodide trapping by the thyroid is influenced by the concentration of TSH; which stimulates the pump and hypophysectomy greatly diminishes the activity of it.
2- Oxidation of the Iodide Ion. is conversion of the iodide ions to an oxidized form of iodine, this oxidation of iodine is promoted by the enzyme peroxidase.
3-Iodination of Tyrosine and Formation of the Thyroid Hormones. Oxidized iodine will be secreted to the lumen of the follicle where it will bind directly but very slowly with the amino acid tyrosine. Tyrosine is first iodized to monoiodotyrosineand then to diiodotyrosine. 2 molecules of diiodotyrosine will form thyroxin(T4), and one monoiodotyrosine with one diiodotyrosine, will form triiodothyronin(T3).
4- All these forms will attach to a protein called thyroglobulin, which is a glycoprotein. It is synthesized in the thyroid cells and secreted by the thyroid cells into the colloid in lumen of the follicle under the effect of TSH. The thyroid hormones remain part of the thyroglobulin molecules until secreted (when synthesis of thyroid hormone stops, the physiologic effects of deficiency are not observed for several months, because there are sufficient amounts for 2-3 months attached to thyroglobulin).
When needed thyroxin and triiodothyronine must first be cleaved from the thyroglobulin molecule, and then these free hormones are released.
On entering the blood, over 99 per cent of the thyroxine and triiodothyronine combines immediately with several of the plasma proteins, all of which are synthesized by the liver. They combine mainly with thyroxine-binding globulin (TBG), binds mainly to T4, and thyroxine-binding prealbumin(TBPA)bound mainly to T3and albumin.
Thyroxine (T4)—are released to the tissue cells slowly, has high affinity for binding with blood proteins (binding is strong). While triiodothyronine—because of its lower affinity to binding with blood proteins—is released to the cells easier.
The physiological action of thyroid hormone:
1- Thyroid hormones increase the transcription of large numbers of genes;It activates nuclear transcription of large numbers of genes, so there will be generalized increase in functional activity throughout the body. Before acting on the genes to increase genetic transcription, one iodide is removed from almost all the thyroxine, thus forming triiodothyronine. Intracellular thyroid hormone receptors have a very high affinity for triiodothyronine. Consequently, more than 90 per cent of the thyroid hormone molecules that binds with the receptors is triiodothyronine.
2-Thyroid hormones increase cellular metabolic activity:
The thyroid hormones increase the metabolic activities of almost all the tissues of the body (increase BMR) There will be increase the number and activity of mitochondria, which increases the rate of formation of (ATP) .Also the enzyme Na+-K+- ATPase, increases its activity which needs energy so increases heat production. So the metabolic rate can increase to 60 to 100 per cent above normal when large quantities of the hormones are secreted.
Basal metabolic rate BMR is the quantity of energy production at rest during optimal temperature, measured 12 hours after last meal.
3-Has Calorigenic Action:
T4 and T3 increase the O2 consumption and heat production of almost all metabolically active tissues. The exceptions are the adult brain, testes, uterus, lymph nodes, spleen, and anterior pituitary. T4 actually depresses the O2 consumption of the anterior pituitary, presumably because it inhibits TSH secretion.
4-Effect on carbohydrates ,fat and protein:
Concerning:
Carbohydrates,It stimulates rapid uptake of glucose by the cells, enhanced glycolysis, enhanced hepatic gluconeogenesis, increased rate of absorption from the gastrointestinal tract, and even increased insulin secretion.So we have increase in blood glucose concentration.
Fat, it has a lipolytic action. Lipids are mobilized rapidly from the fat tissue, which decreases the fat stores of the body to a greater extent than almost any other tissue element. This also increases the free fatty acid concentration in the plasma and greatly accelerates the oxidation of free fatty acids by the cells. It also decreases the concentrations of cholesterol, phospholipids, and triglycerides in the plasma, even though it increases the free fatty acids, because it increases the rate of cholesterol secretion in the bile and consequent loss in the feces. Another possible mechanism of decreasing plasma cholesterol is due to increased formation of LDL(low density lipoprotein) receptors in the liver, resulting in increased hepatic removal of cholesterol from the circulation.
Thyroid hormone may also cause lipolysis indirectly through potentiation of the effect of other hormones like adrenaline, glucagon and glucocorticoids.
In hypothyroidism (low T3 and T 4), there will be high cholesterol level which may predispose to atherosclerosis and the patient will be liable to heart diseases like myocardial infarction.
Protein,it stimulates the synthesis of specific proteins, so small amounts of thyroid hormone are necessary for the maintenance of normal rate of protein synthesis. This anabolic action occurs when TH is within the physiological limits. But if we have increase in the level of thyroid hormone this anabolic will to catabolic action, and cause protein breakdown especially in muscles and causes muscle weakness(thyrotoxic myopathy),. As a result of protein catabolism the plasma creatinin increases and causes excessive amino acids in blood (creatinurea).Conversely, lack of thyroid hormone causes the muscles to become sluggish, and they relax slowly after a contraction.
In hypothyroidism, there will be deposition of mucoprotein subcutaneously which sucks water and causes swelling (edema) differ from heart failure edema because it is not pitting.
Vitamins, thyroid hormone causes increased need for vitamins. Therefore, a relative vitamin deficiency can occur when excess thyroid hormone is secreted.
5-Effect of Thyroid Hormones on the Cardiovascular System;
Increased Blood Flow and Cardiac Output. The increase metabolism causesvaso dilatation in most body tissues, thus increasing blood flow (increase in metabolism will cause accumulation of metabolites and vasodilatation). The rate of blood flow in the skin especially increases because of the increased need for heat elimination from the body. As a result of increase blood flow, the cardiac output increases.
The heart rate increases considerably, so it is one of the sensitive physical signs that the clinician uses in determining whether a patient has excessive or diminished thyroid hormone production.
The systolic blood pressure increases because thyroid hormone enhances the effect of chatcholamines(increase in the rate and force of contraction). While peripherally the vasodilatation due to the increase inBMR will cause decrease in the peripheral resistance that means drop in the diastolic blood pressure. As a result of that we have increase in the pulse pressure (pulse pressure= systolic blood pressure- diastolic pressure).
The mean arterial pressure usually remains about normalbecause the rise in systolic is equal to the drop in diastolic.
The heart muscle strength becomesdepressed because of long-term excessive proteincatabolism.
6-Effect on respiration:
The increased rate of metabolism increases the utilization of oxygen and formation ofcarbon dioxide; these effects activate all the mechanismsthat increase the rate and depth of respiration to get rid of the accumulated CO2.7-Effect on GIT:
TH causes an increase in the absorption of food stuffs and an increase in the rate of secretion of digestive juices and increase in the motility of GIT. Excessive thyroid hormone results in diarrhea (frequent bowel motion) and associated with increase appetite due to increase of BMR and increase of consumption of ATP and sometimes loss of weight.
The lack of the TH will cause constipation and decreased appetite and sometimes increase in weight due to decrease in BMR and a decrease in consumption of energy, decrease of lipolysis and accumulation of lipids and fats in the body.
8-Effect on sexual function:
In men, lack of thyroid hormone is likely to cause loss of libido (decrease desire to have intercourse); great excesses of the hormone, however, sometimes cause impotence (failure of erection).In women, lack of thyroid hormone often causes menorrhagia and polymenorrhea— that is, respectively, excessive and frequent menstrual bleeding. A hypothyroid woman, like a man, is likely to have greatly decreased libido. While in the hyperthyroid woman, oligomenorrhea, which means greatly reduced bleeding, is common, and occasionally amenorrhea results.
9-Effect on growth (effect on the bone):
Thyroid hormones are essential for normal growth and skeletal maturation. In hypothyroid children like congenital hypothyroidism, bone growth is slowed and epiphysial closure delayed. In the absence of thyroid hormones, growth hormone secretion is also depressed, and thyroid hormones potentiate the effect of growth hormone on the tissues.
In those who are hyperthyroid, excessive skeletal growth often occurs, causing the child to become considerably taller at an earlier age. However, the bones also mature more rapidly and the epiphyses close at an early age, so that the duration of growth and the eventual height of the adult may actually be shortened.
Excess thyroid hormone secretion result in excessive demineralization of the bone and a resultant increase in urinary loss of calcium and phosphate and this effect is apart from the effect of parathyroid hormone but it is due to the catabolic effect of TH on the proteins as part of the matrix of the bone.
10-Effect on the central nervous system:
An important effect of thyroid hormone is to promote growth and development of the brain (normal development of the cerebrum and mylination of the nerve fibers during fetal life and for the first few years of postnatal life. If the fetus does not secrete sufficient quantities of thyroid hormone, growth and maturation of the brain both before birth and afterward are greatly retarded, and the brain remains smaller than normal. Without specific thyroid therapy within days or weeks after birth, the child without a thyroid gland will remain mentally deficient throughout life.
In general, thyroid hormone increases the rapidity of cerebration. Conversely, lack of thyroid hormone decreases this function. The hyperthyroid individual is likely to have extreme nervousness, irritability, exaggerated response to environmental stimuli and many psychoneurotic tendencies, such as anxiety complexes, extreme worry, and paranoia (always suspect) , because TH results in hyperexcitibilty due to increase in synaptic transmission .While in hypothyroidism the person become weak, no energy, slowness of speech, diminished speed of nerve conduction.
11-Effect on Sleep. Because of the exhausting effect of thyroid hormone on the musculature and on the central nervous system, the hyperthyroid subject often has a feeling of constant tiredness, but because of the excitable effects of thyroid hormone on the synapses, it is difficult to sleep. Conversely, extreme somnolence is characteristic of hypothyroidism.
12-Effect on Other Endocrine Glands. Increased thyroid hormone increases the rates of secretion of most other endocrine glands, but it also increases the need of the tissues for the hormones. For instance, increased thyroxine secretion increases the rate of glucose metabolism everywhere in the body and therefore causes a corresponding need for increased insulin secretion by the pancreas. Also, thyroid hormone increases many metabolic activities related to bone formation and, as a consequence, increases the need for parathyroid hormone. Thyroid hormone also increases the rate at which adrenal glucocorticoids are inactivated by the liver. This leads to feedback increase in adrenocorticotropic hormone production by the anterior pituitary and, therefore, increased rate of glucocorticoid secretion by the adrenal glands.
Lec 5
Objectives:What is goiter? Enumerate the causes of iodine deficiency?
Explain the physiological influence of hypothyroidism and hyperthyroidism?
Describe the action of parathyroid hormone?
Clinical conditions of thyroid hormone disturbance:
Enlargement of the thyroid gland for any reason is called goiter. The metabolic function of the gland is either increased or decreased (hyper or hypothyroidism).Endemic goiter
Usually in places where iodine is insufficient in food, so there is inadequate formation of the TH. The mechanism for development of large endemic goiters is the following: Lack of iodine prevents production of TH. As a result, no hormone is available to inhibit production of TSH by the anterior pituitary; this causes the pituitary to secrete excessively large quantities of TSH. .The TSH then stimulates the thyroid cells to secrete tremendous amounts of thyroglobulin colloid into the follicles, and the gland grows larger and larger.Idiopathic Nontoxic Colloid Goiter. Enlarged thyroid glands similar to those of endemic goiter can also occur in people who do not have iodine deficiency. These goitrous glands may secrete normal quantities of thyroid hormones, but more frequently, the secretion of hormone is depressed, as in endemic colloid goiter.
The exact cause of the enlarged thyroid gland in patients with idiopathic colloid goiter is not known, but most of these patients show signs of mild thyroiditis.
Iodine deficiency is due to:
1-Deficiency of iodine intake.
2-Substances interfere with absorption of iodide from GIT.
3-Substances interfere with the taken up by follicular cells such as thiocynate ions. Some foods contain goitrogenic substances, thus leading to TSH-stimulated enlargement of the thyroid gland. Such goitrogenic substances are found especially in some varieties of turnips and cabbages.
4- Substances interfering with its transforming to iodine.
In some persons with colloid goiter, the thyroid gland has an abnormality of the enzyme system required for formation of the thyroid hormones.
1. Deficient iodide-trapping mechanism, 2. Deficient peroxidase system, in which the iodides are not oxidized to the iodine state
3. Deficient coupling of iodinated tyrosines in the thyroglobulin molecule,
4. Deficiency of the deiodinase enzyme, which prevents recovery of iodine from the iodinatedtyrosines that are not coupled to form the thyroid hormones.
Hypothyroidism:
The cause is either in the thyroid gland or in pituitary or hypothalamus.
Hypothyroidism, probably is initiated by autoimmunity against the thyroid gland. The thyroid glands of most of these patients first have autoimmune “thyroiditis,” which means thyroid inflammation. Several other types of hypothyroidism also occur, often associated with development of enlarged thyroid glands, called thyroid goiter, as discussed. So the causes for hypothyroidism:
thyroiditis, endemic colloid goiter, idiopathic colloid goiter, destruction of the thyroid gland by irradiation, or surgical removal of the thyroid gland.
Physiologic Characteristics of Hypothyroidism.
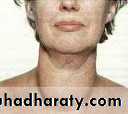
Fatigue and extreme somnolence with sleeping up to 12 to 14 hours a day, extreme muscular sluggishness (decrease tone), slowed heart rate, decreased cardiac output, decreased blood volume, sometimes increased body weight, constipation, mental sluggishness, depressed growth of hair and dryness of the hair and skin, development of husky voice, slowness of speech and, in severe cases, development of an edematous appearance throughout the body called myxedema. HypothyroidMyxedema. Develops in the patient with almost total lack of thyroid hormone function such a patient, demonstrating bagginess under the eyes and swelling of the face. In this condition, for reasons not explained, greatly increased quantities of hyaluronic acid and chondroitin sulfate bound with protein form excessive tissue gel in the interstitial spaces and this causes the total quantity of interstitial fluid to increase. Because of the gel nature of the excess fluid, it is mainly immobile, and the edema is the non pitting type (hard), while in case of for example renal and liver failure.
Atherosclerosis in Hypothyroidism. Lack of thyroid hormone increases the quantity of blood cholesterol
The increase in blood cholesterol is usually associated with increased atherosclerosis. Therefore, many hypothyroid patients, particularly those with myxedema, develop atherosclerosis, which in turn results in peripheral vascular disease, deafness, and coronary artery disease with consequent early death.
Diagnostic Tests in Hypothyroidism.
The free thyroxine in the blood is low. The basal metabolic rate low. And the secretion of TSH by the anterior pituitary is usually greatly increased.
Cretinism
It is caused by extreme hypothyroidism during fetal life, infancy, or childhood. This condition is characterized especially by failure of body growth and by mental retardation. It results from: 1- congenital lack of a thyroid gland (congenital cretinism), 2- from failure of the thyroid gland to produce thyroid hormone because of a genetic defect of the gland, or from iodine lack in the diet especially of the pregnant woman (endemic cretinism).A neonate without a thyroid gland may have normal appearance and function because it was supplied with some (but usually not enough) thyroid hormone by the mother while in utero, but a few weeks after birth, the neonate’s movements become sluggish and both physical and mental growth begin to be greatly retarded.
We have to treat the child during the first few weeks after birth .and if not there will be mental and growth retardation.3- treatment of the hyperthyroid mother with antithyroid drugs that passes placental barrier to fetus.
Skeletal growth in the child with cretinism is characteristically more inhibited than is soft tissue growth. As a result of this disproportionate rate of growth, the soft tissues are likely to enlarge excessively, giving the child with cretinism an obese and short appearance.
So in cretinism we have short stature and mental retardation, while in GH deficiency we also have short stature but without mental retardation.
Occasionally the tongue becomes so large in relation to the skeletal growth that it obstructs swallowing and breathing.
Hyperthyroidism
Excessive thyroid secretion.In hyperthyroidism, the level of TSH is reduced, but it is not accompanied by the decrease in thyroid hormone. Because there are substances which have similar action to that of TSH found in the blood of almost all patients, these are immunoglobulin antibodies that bind with the same membrane receptors that bind TSH. They induce continual activation of the cAMP system of the cells, with resultant development of hyperthyroidism. These antibodies are called thyroid-stimulating immunoglobulin (TSI).
Thyroid Adenoma.Hyperthyroidism occasionally results from a localized adenoma (a tumor) that develops in the
Thyroid tissue and secretes large quantities of thyroid hormone.
Symptoms of Hyperthyroidism
(1) a high state of excitability, (2) intolerance to heat, (3) increased sweating, (4) mild to extreme weight loss (sometimes as much as 100 pounds), (5) varying degrees of diarrhea (increase in GIT motility), increase appetite (6) muscle weakness, (7) nervousness or other psychic disorders, (8) extreme fatigue but inability to sleep, and (9) tremor of the hands.10) vitamin deficiency especially D.Exophthalmos. It is protrusion of the eyeballs, sometimes becomes so severe that the eyeball protrusion stretches the optic nerve enough to damage vision. Much more often, the eyes are damaged because the eyelids do not close completely when the person blinks or is asleep. As a result, the epithelial surfaces of the eyes become dry and irritated and often infected, resulting in ulceration of the cornea. The cause of the protruding eyes is edematous swelling of the retro-orbital tissues and degenerative changes in the extraocular muscles.
Muscle Tremor. One of the most characteristic signs of hyperthyroidism is a fine muscle tremor. This is not the coarse tremor that occurs in Parkinson’s disease or in shivering, because it occurs at the rapid frequency of 10 to 15 times per second. The tremor can be observed easily by placing a sheet of paper on the extended fingers and noting the degree of vibration of the paper. This tremor is believed to be caused by increased reactivity of the neuronal synapses in the areas of the spinal cord that control muscle tone. The tremor is an important means for assessing the degree of thyroid hormone effect on the central nervous system.
Calcitonin:
This peptide hormone is synthesized and secreted by the parafollicular cells (c- cells), it is also called calcium lowering hormone it is not under the control of pituitary or the hypothalamus. It is affected by the level of calcium in the blood. When it increases, it stimulates the hormone, mobilizes the calcium from the blood to the bone and enhances the osteoblastic activity, so it opposes the parathyroid hormone.We have increase in its level when there is need to calcium i.e growth, pregnancy, lactation.
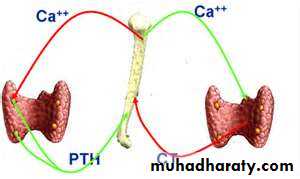
Parathyroid Hormone:
Normally there are four parathyroid glands in humans; they are located immediately behind the thyroid gland—one behind each of the upper and each of the lower poles of the thyroid.Removal of half the parathyroid glands usually causes no major physiologic abnormalities. However, removal of three of the four normal glands causes transient hypoparathyroidism. But even a small quantity of remaining parathyroid tissue is usually capable of hypertrophying satisfactorily to perform the function of all the glands, but its complete removal is lethal because it is essential to life. It controls the level of calcium and phosphate in the blood by the movement of calcium and phosphate from the bone to blood and excretion of PO4 by the kidney.
Usually 99% of calcium is in the bone and small fraction is ionized and circulates in the blood and this is the active form which performs the physiological action. .
Calcium level is controlled by:
1-Parathyroid hormone.
2-Calcitonin
3-Metabolites of vitamine D “1,25dihydroxycholecalceferol”.
The level of calcium is about 10 mg/dl) or 5 meq/L in SI units (the normal requirement of Ca is 1gm/day) and is present in 3 forms:
Non diffusible through the capillary membrane form 41%: bound to protein albumin, Globulin.
Hyperventilation→ alkalosis→ increase protein→ increase number of non diffusibleform→ decreased ionized diffusible form→ increase the excitability of nerve and muscle→tetany.
2-About 9 per cent of the calcium is diffusible through the capillary membrane but is combined with anionic substances of the plasma and interstitial fluids (non ionized).
3-The remaining 50 per cent of the calcium in the plasma is both diffusible through the capillary membrane and ionized.
The diffusible form isperforming physiological functions.
1-Maintain membrane permeability.
2-Activation of enzymatic process involved in muscular contraction.
3-Release of neurohormones and neuropeptides.
4-Excitability of neuromuscular system
5-Involvement in clotting mechanism.
6- It acts as hydroxyapetite in the bone, responsible for the strength of the bone so if there is decrease in the Ca in the bone it will become liable for fractures as in case of old age.
Calcium is absorbed from the first half of the small intestine partly by active transport and partly be the help of vitamin D.
The phosphate level is 3-4 mg/dl as follows:
85% in bone, 14% intracellular, 1% extracellular fluid.
If we multiply the concentration of calcium by the concentration of phosphate we will get the figure 40, this is a constant figure, so whenever we have hypercalciemia we have hypophosphatemia.
Parathyroid hormone acts on calcium and phosphate through:
1-Parathyroid Hormone Increases Calcium and Phosphate Absorption from the Bone:
It mobilizes both calcium and phosphate from the bone to the extracellular fluid; as a result we have increase in calcium and phosphate in the plasma.
2-Parathyroid Hormone Increases Intestinal Absorption of Calcium and Phosphate:
It increases the absorption leading to increase in calcium and phosphate in plasma this effect is enhanced by metabolite of vitamin D.3-Parathyroid Hormone Decreases Calcium Excretion and Increases Phosphate Excretion by the Kidneys
It increases phosphate excretion in the urine and decreases renal tubular reabsorption of phosphate and increase reabsorption of calcium so we get rid of the excess phosphate in the body, so still there is equilibrium between the calcium and phosphate.
Clinical conditions:
1-Hypofunction of the parathyroid hormone (hypoparathyroidism):This leads to decrease in calcium concentration in the blood → abnormal function of the neuromuscular system → hyperexcitibilty of the nerves and muscle(low threshold of excitation).
This may be sever especially in children and may lead to laryangeal spasm →asphyxia and death.
Hypoparathyrodismmay be mild and we have twitching of the facial muscles elicited by mild stimuli( which is normally not enough to produce twitching of the muscle)because we have trapping of the facial nerve at the angle of the jaw, this condition is called chvostek' s sign .
The other sign we can see it by occlusion of blood flow to the hand like by a sphygmomanometer, this will lead to more decrease in calcium, so we have flexion of the wrist and thumb,extension of the fingers this is called trousseau's sign.
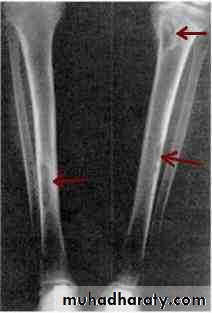
2-Hyperparathyroidism:
The cause may be:
1-Primary: tumor in the gland (mainly in women because of lactation and pregnancy which predispose for tumors).
2-Secondary: vitamin D deficiency or chronic renal failure.
Excessive secretion of the parathyroid gland will cause excessive mobilization of calcium and phosphate from the bone to the extracellular fluid .If we take x ray to the bone we will see a cyst filled with fibrous tissue so we call this condition osteitisfibrosacystica.
The bone will be liable for mild trauma and fracture.
The increase in osteoclastic activity will cause increase in the osteoblastic activityto replace the eating bone.
The most important complication is renal calculi (stones) which is associated with increase calcium level.
Other complications: CNS excitability, constipation, weakness and hypophosphatemia.
Oestitis fibrosacystica