DISORDERS OF THE SPINAL NERVES AND SPINAL CORD
The spinal cord and spinal roots may be affected by intrinsic disease or by disorders of the surrounding meninges and bones. The clinical presentation of these conditions depends on the anatomical level at which the cord or roots are affected, as well as the nature of the pathological process involved. It is important to recognise when emergency surgical intervention is necessary and to plan investigations to identify such patients.COMPRESSION OF THE SPINAL CORD
Acute spinal cord compression is one of the most common neurological emergencies encountered in clinical practice. A space-occupying lesion within the spinal canal may damage nerve tissue either directly by pressure or indirectly by interfering with blood supply. Oedema from venous obstruction impairs neuronal function, and ischaemia from arterial obstruction may lead to necrosis of the spinal cord. The early stages of damage are reversible but severely damaged neurons do not recover; hence the importance of early diagnosis and treatment.
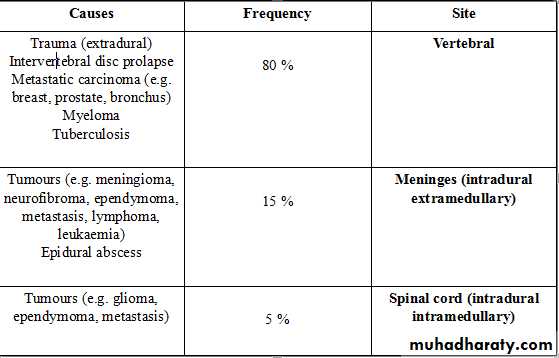
CAUSES OF SPINAL CORD COMPRESSION
Clinical features
The onset of symptoms of spinal cord compression is usually slow (over weeks), but can be acute as a result of trauma or metastases, especially if there is associated arterial occlusion.SYMPTOMS OF SPINAL CORD COMPRESSION
PainLocalised over the spine or in a root distribution, which may be aggravated by coughing, sneezing or straining
Sensory
Paraesthesia, numbness or cold sensations, especially in the lower limbs, which spread proximally, often to a level on the trunk
Motor
Weakness, heaviness or stiffness of the limbs, most commonly the legs
Sphincters
Urgency or hesitancy of micturition, leading eventually to urinary retention
Pain and sensory symptoms occur early, while weakness and sphincter dysfunction are usually late manifestations. The signs vary according to the level of the cord compression and the structures involved. There may be tenderness to percussion over the spine if there is vertebral disease, and this may be associated with a local kyphosis. Involvement of the roots at the level of the compression may cause dermatomal sensory impairment and corresponding lower motor signs. Interruption of fibres in the spinal cord causes sensory loss
SIGNS OF SPINAL CORD COMPRESSION
Cervical, above C5
Upper motor neuron signs and sensory loss in all four limbs
Diaphragm weakness (phrenic nerve)
Cervical, C5 to T1
Lower motor neuron signs and segmental sensory loss in the arms; upper motor neuron signs in the legs
Respiratory (intercostal) muscle weakness
Thoracic cord
Spastic paraplegia with a sensory level on the trunk
Conus medullaris
Lesions at the end of the spinal cord cause sacral loss of sensation and extensor plantar responses
Cauda equina
Spinal cord ends at approximately the T12/L1 spinal level and spinal lesions below this level can only cause lower motor neuron signs by affecting the cauda equina
INVESTIGATION OF ACUTE SPINAL CORD SYNDROME
Plain X-rays of spine may show bony destruction and soft-tissue abnormalities and are an essential initial investigationChest X-rays may provide evidence of systemic disease
MRI of spine is the investigation of choice; myelography also localises the lesion and, with CT in suitable cases, defines the extent of compression and associated soft-tissue abnormality
CSF should be taken for analysis at the time of myelography. In cases of complete spinal block this shows a normal cell count with a very elevated protein causing yellow discoloration of the fluid (Froin's syndrome). Acute deterioration may develop after myelography and the neurosurgeons should be alerted before it is undertaken.
Serum B12
Needle biopsy is required prior to radiotherapy to establish the histological nature of the tumour.
false
Loss of vertebral pedicle (arrow) by bony erosion of an osteolytic metastasisfalse
An osteosclerotic metastasis falsefalse
A neurofibroma is compressing the spinal cord and emerging in a 'dumbbell' fashion through the vertebral foramen into the paraspinal space.
Management
Treatment and prognosis depend on the nature of the underlying lesion. Benign tumours should be surgically excised, and a good functional recovery can be expected unless a marked neurological deficit has developed before diagnosis.
Extradural compression due to malignancy is the most common cause of spinal cord compression in developed countries and has a poor prognosis, although useful function can be regained if treatment is initiated within 24 hours of the onset of severe weakness or sphincter dysfunction. Surgical decompression may be appropriate in some patients, but has a similar outcome to radiotherapy.
Spinal cord compression due to tuberculosis is common in some areas of the world, and requires surgical treatment if seen early. This should be followed by appropriate anti-tuberculous chemotherapy for an extended period.
Traumatic lesions of the vertebral column require specialised neurosurgical treatment.
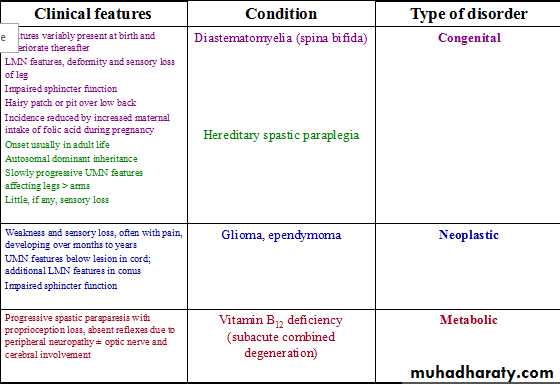
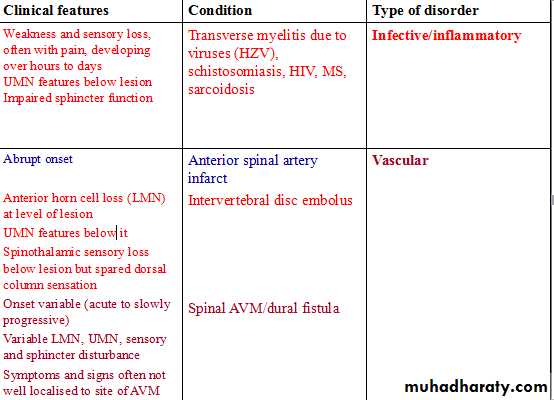
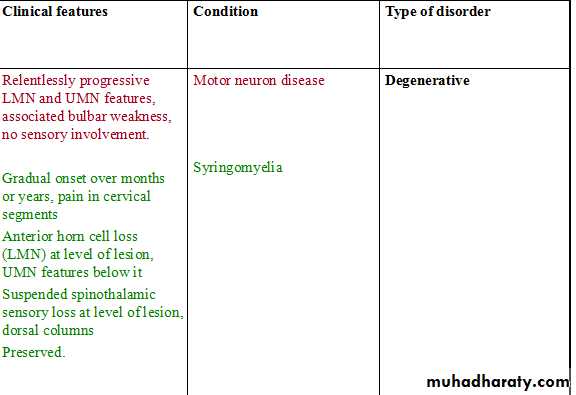
INTRINSIC DISEASES OF THE SPINAL CORD
INTRINSIC DISEASES OF THE SPINAL CORD
INTRINSIC DISEASES OF THE SPINAL CORD
CERVICAL SPONDYLOSIS
In the cervical spine, some degree of osteoarthritic degenerative change is a normal radiological finding in the middle-aged and elderly. Degeneration of the intervertebral discs and secondary osteoarthrosis (cervical spondylosis) is often asymptomatic, but may be associated with neurological dysfunction. The C5/6, C6/7 and C4/5 vertebral levels and C6, C7 and C5 roots, respectively, are most commonly affectedCERVICAL SPONDYLOTIC RADICULOPATHY
Compression of a nerve root occurs when a disc prolapses laterally, which may develop acutely or more gradually due to osteophytic encroachment of the intervertebral foramina.Clinical features
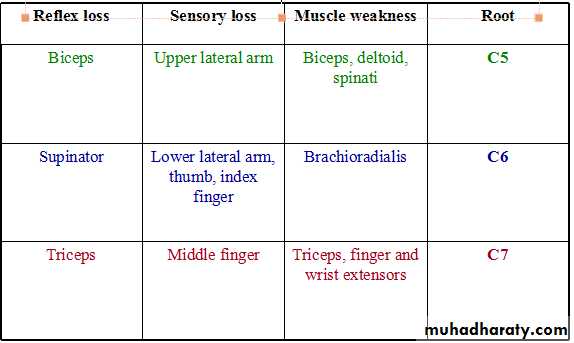
The patient complains of pain in the neck that may radiate in the distribution of the affected nerve root. The neck is held rigidly and neck movements may exacerbate pain. Paraesthesia and sensory loss may be found in the affected segment and there may be lower motor neuron signs, including weakness, wasting and reflex impairmentPHYSICAL SIGNS IN CERVICAL ROOT COMPRESSION
Investigations
Plain X-rays, including lateral and oblique views, should be obtained to confirm the presence of degenerative changes and to exclude other conditions, including destructive lesions. If surgery is contemplated, MRI is required. Electrophysiological studies rarely add to the clinical examination, but may be necessary if there is doubt about the differential diagnosis between root and peripheral nerve lesions.
Management
Conservative treatment with analgesics and physiotherapy results in resolution of symptoms in the great majority of patients, but a few require surgery in the form of foraminotomy or disc excision.CERVICAL SPONDYLOTIC MYELOPATHY
Dorsomedial herniation of a disc and the development of transverse bony bars or posterior osteophytes may result in pressure on the spinal cord or the anterior spinal artery which supplies the anterior twothirds of the cordLUMBAR DISC HERNIATION
Acute lumbar disc herniation is often precipitated by trauma, usually by lifting heavy weights while the spine is flexed. The nucleus pulposus may bulge or rupture through the annulus fibrosus, giving rise to pressure on nerve endings in the spinal ligaments, changes in the vertebral joints or pressure on nerve roots.Clinical features
The onset may be sudden or gradual. Alternatively, repeated episodes of low back pain may precede sciatica by months or years. Constant aching pain is felt in the lumbar region and may radiate to the buttock, thigh, calf and foot. Pain is exacerbated by coughing or straining but may be relieved by lying flat.The altered mechanics of the lumbar spine result in loss of lumbar lordosis and there may be spasm of the paraspinal musculature. Root pressure is suggested by limitation of flexion of the hip on the affected side if the straight leg is raised (Lasègue's sign). If the third or fourth lumbar roots are involved, Lasègue's sign may be negative, but pain in the back may be induced by hyperextension of the hip (femoral nerve stretch test).
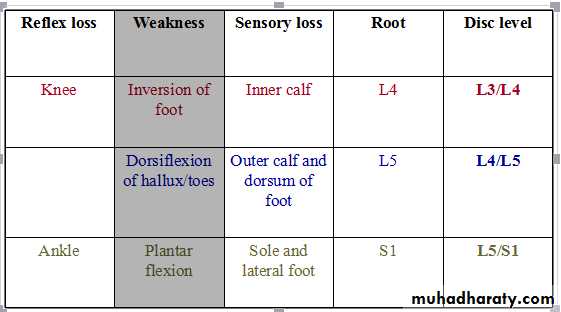
PHYSICAL SIGNS IN LUMBAR ROOT COMPRESSION
Investigations
Plain X-rays of the lumbar spine are of little value in the diagnosis of lumbar disc disease, although they may show other conditions such as malignant infiltration of a vertebral body. CT, especially using spiral scanning techniques, can provide helpful images of the disc protrusion and/or narrowing of the exit foramina. MRI is the investigation of choice if available, since soft tissues are well imaged.L5–SI disc herniationto the left, displacing the SI nerve root