1
Fifth stage
Surgery
Lec-5
.د
أركان
29/3/2016
CARDIOPULMONARY RESUSCITATION CPR
Cardiopulmonary resuscitation (CPR) is a key part of emergency medical care designed
to resuscitate individuals in cardiac arrest
‘Revives heart (cardio) and lung (pulmonary) functioning’
The purpose of CPR is to temporarily provide effective oxygenation of vital organs,
especially the brain and heart, through artificial circulation of oxygenated blood until
the restoration of normal cardiac and respiratory activity occurs
This is to stop the degenerative processes of ischemia and anoxia caused by inadequate
circulation and inadequate oxygenation.
Time to initiation of CPR is critical to improve likelihood of recovery; ideally, it should
be started within 4 min of arrest, and advanced cardiac life support should be initiated
within 8 min of arrest
Basic life support BLS
Basic life support is the maintenance of an airway & the support of breathing & the
circulation .
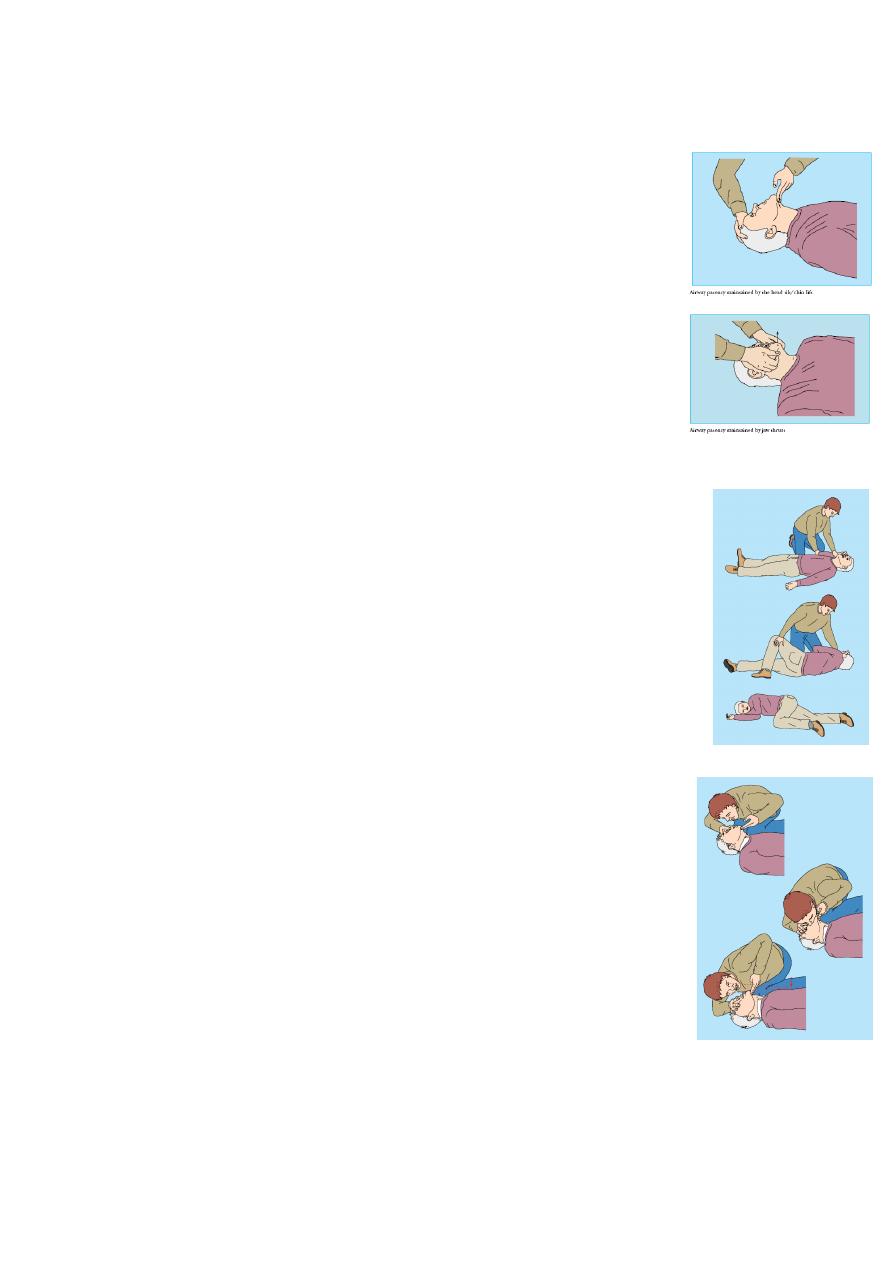
Assessment
When approaching a patient who appears to have suffered a
cardiac arrest the rescuer should check that there are no hazards
to himself before proceeding to treat the patient
Rapidly assess any danger to the patient & yourself from hazards
such as electricity ; fire or traffic.
2
Establish whether the patient is responsive by gently shaking his or her shoulder &
asking loudly “are you all right” ?
If no response is given; shout for help.
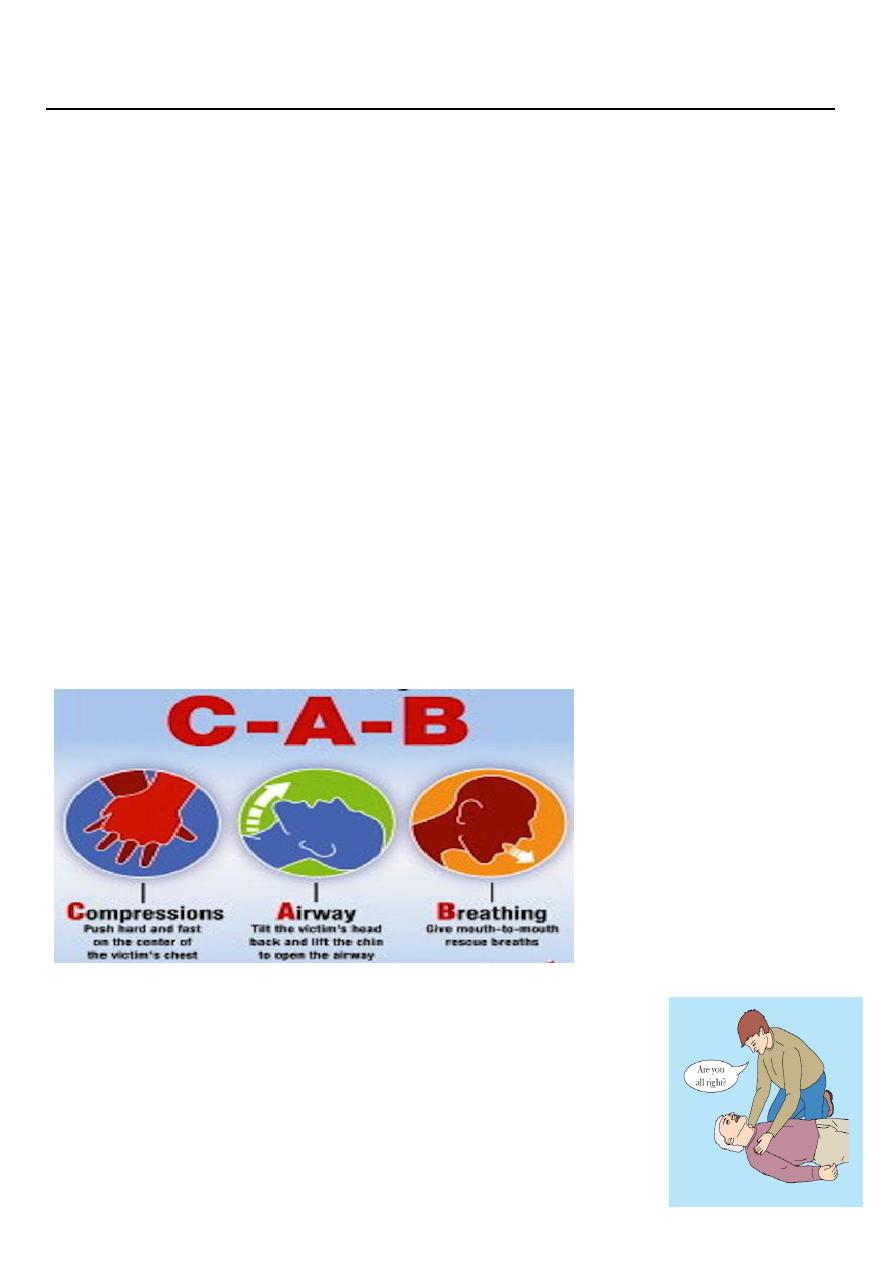
Airway
Loosen tight clothing around the patient neck.
Extend the neck ;thus lifting the tongue off the posterior wall of the
pharynx . Head tilt/chin lift.
If suspect cervical spine injury → jaw thrust
Remove any obvious obstruction from the mouth.
“All rescuers should immediately begin CPR for adult victims who
are unresponsive with no breathing or no normal breathing (only
gasping).”
Quick “look” for no breathing or no normal breathing
Recovery position
If the patient is unconscious but is breathing ; place him or her in the
recovery position.
In this position the tongue will fall away from the pharyngeal wall & any
vomit or secretion will flow out of the corner of the mouth rather than
obstruct the airway or later on cause aspiration
If breathing is absent ; pinch the nose closed with fingers of your
hand .Take a breath ;seal your lips firmly around those of the patient
& breath out until you see the patient’s chest rising.
The chest should rise as you blow in & fall when you take your
mouth away.
Rescue breaths deliver over 1 second
The best pulse to feel in an emergency is the carotid pulse; but if the
neck is injured the femoral pulse may be felt at the groin.
Circulation
If there are no signs of circulation (cardiac arrest) ,ensure that the patient is on his or
her back & lying on a firm , flat surface , then start chest compression.
For chest compressions, position hands at center of chest
compression:ventilation ratio is 30 : 2
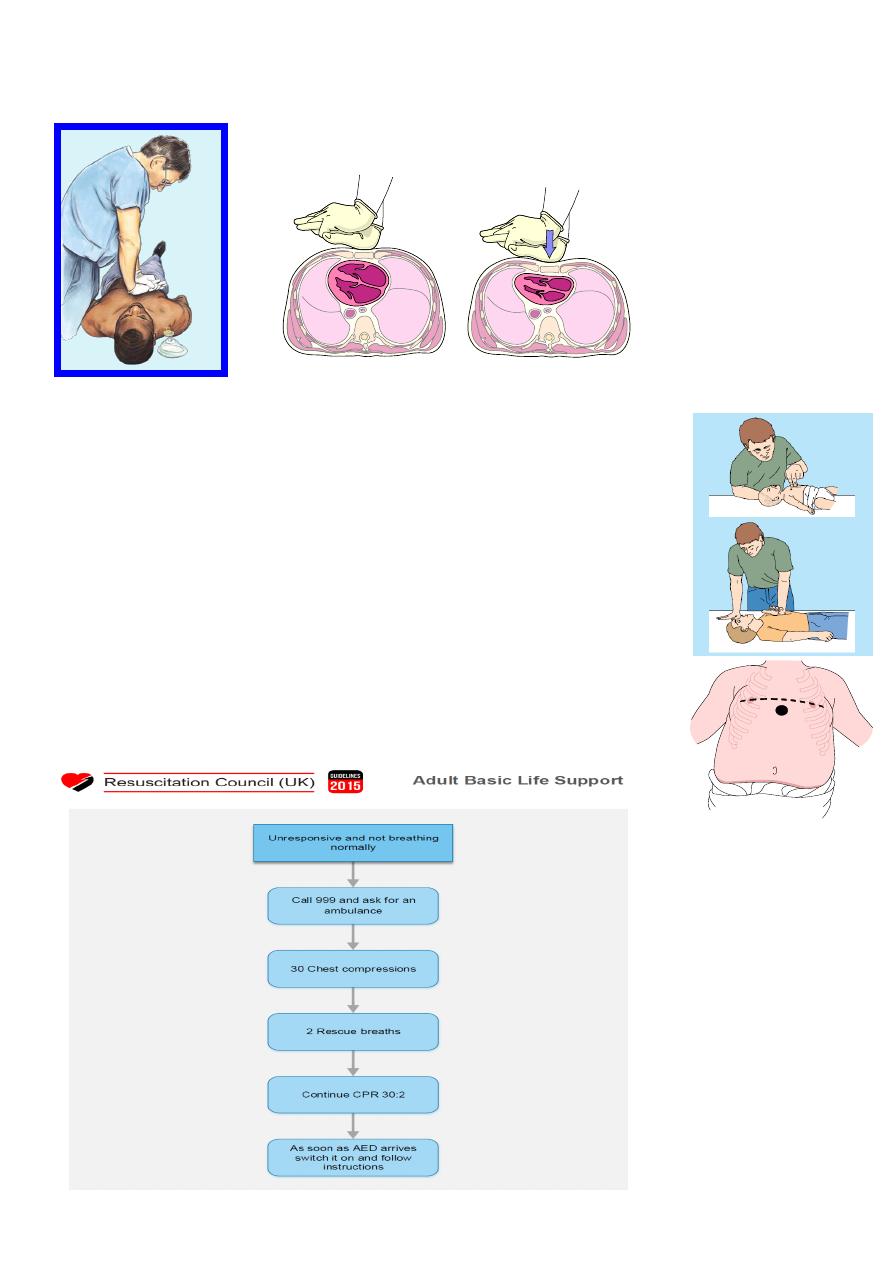
3
compression depth for adults is 5-6 cm
Rate is 100-120 /min
In infants, compress the lower third of the sternum with two fingers
of one hand; the upper finger should be one finger’s breadth below
an imaginary line joining the nipples
When more than one healthcare provider is present, the two-
thumbed (chest encirclement) method of chest compression can be
used for infants
In children, the heel of one hand is positioned over a compression
point two fingers’ breadth above the xiphoid process.
In both infants and children the sternum is compressed to at least
one third of the AP diameter of the chest
4
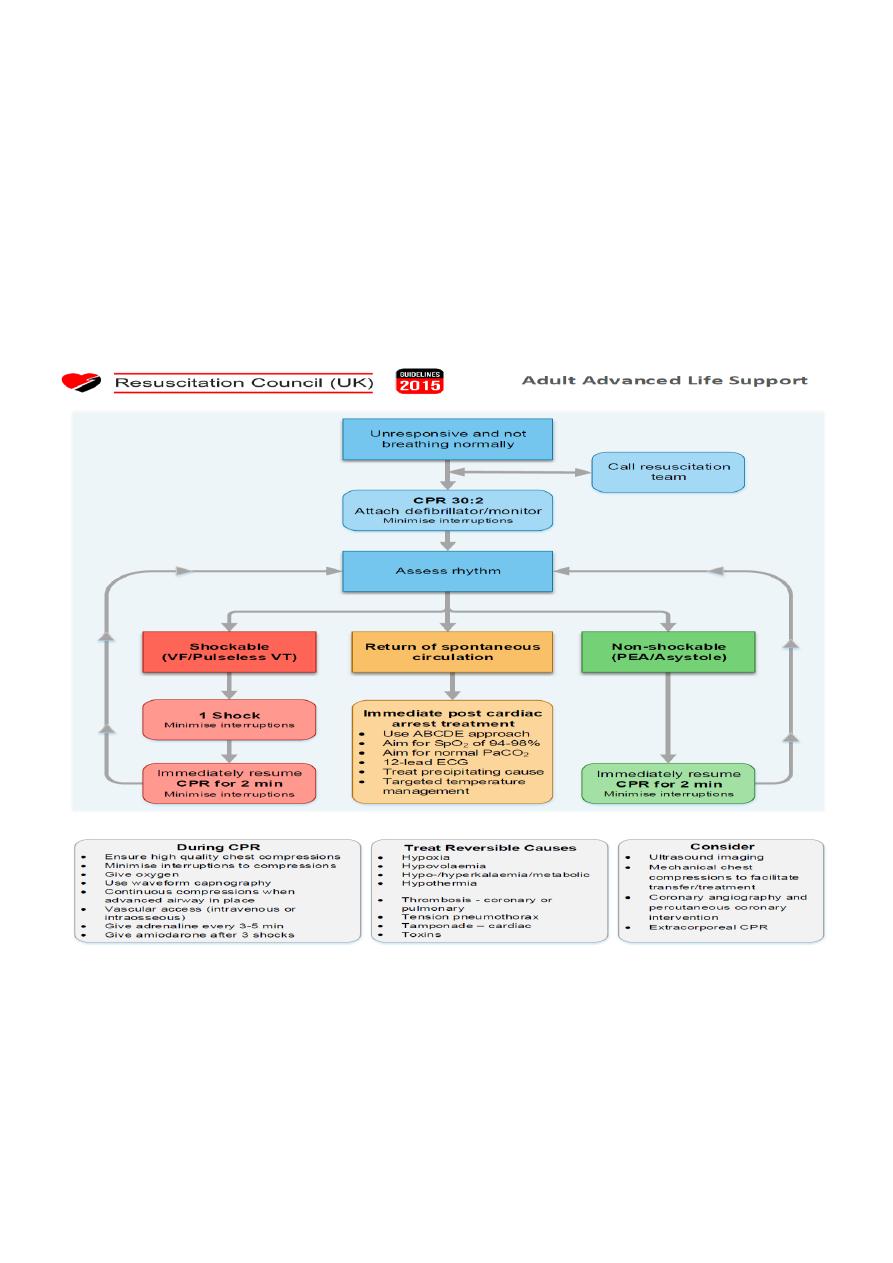
Advanced Cardiac Life Support ACLS
BLS alone will rarely result in successful resuscitation. The purpose of BLS is to maintain
organ blood flow until techniques can be applied to restore spontaneous circulation
• Maintain CPR/BLS.
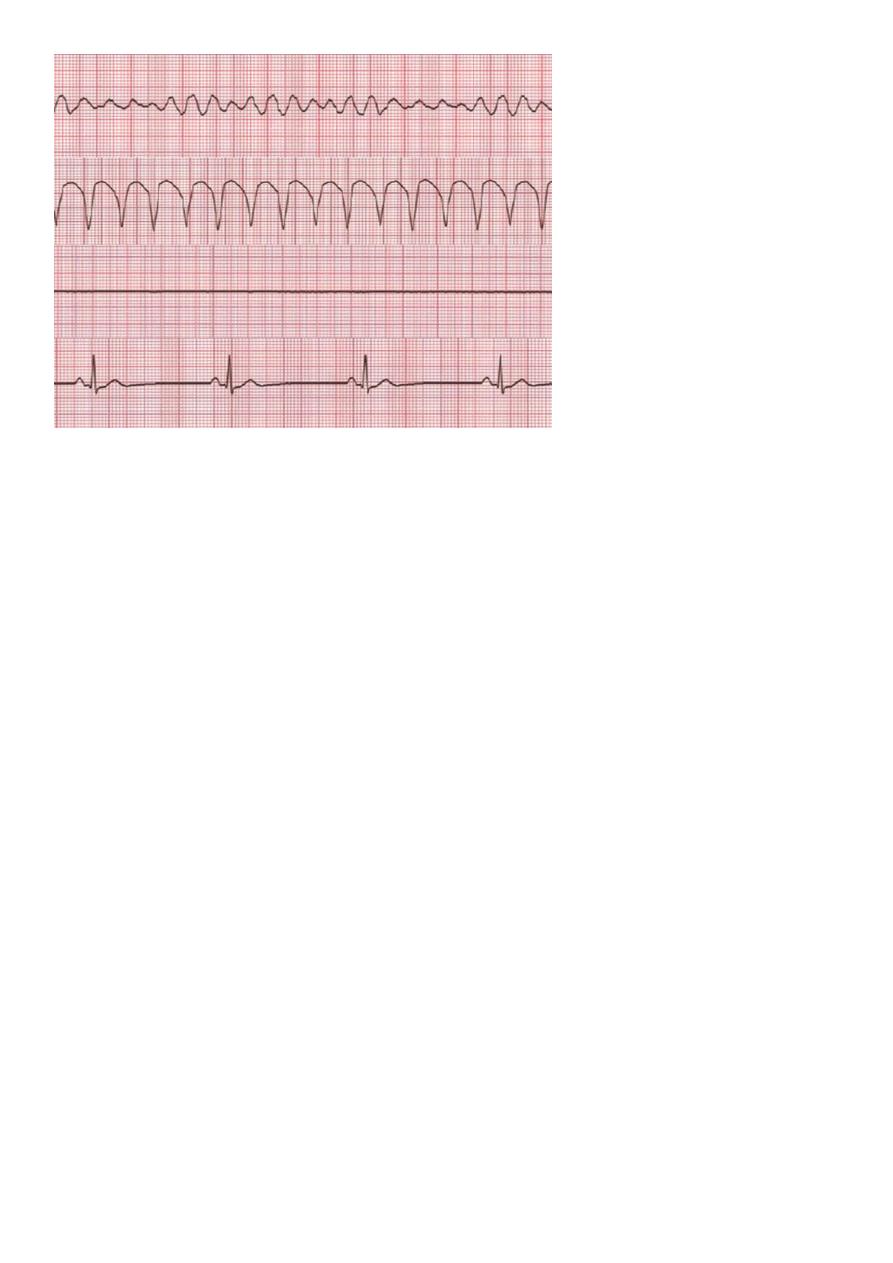
• Defibrillator/monitor attached →Verify rhythm
• Appropriate intravenous access
• Ensure oxygenation (O2 →100%) and intubation if appropriate personnel present
5
Adrenaline (epinephrine) Give adrenaline 1 mg (adults) IV , IO repeat the adrenaline every
3-5 min
Pediatric Dose 0.01 mg/kg IV or IO
Effects :Increases perfusion to myocardium and to brain by increasing peripheral vascular
resistance
Amiodarone ( Anti-arrhythmic drug)
If VF/VT persists after three shocks, give amiodarone 300 mg by bolus injection. A further
dose of 150 mg may be given for recurrent or refractory VF/VT, followed by an infusion of
900 mg over 24 h.
Assisting the circulation
• Intravenous access
Peripheral versus central venous drug delivery
Peripheral venous cannulation is quicker, easier to perform, and safer. Drugs injected
peripherally must be followed by a flush of at least 20 ml of fluid. Central venous line
insertion must cause minimal interruption of chest compression.
• Intraosseous route IO
If intravenous access is difficult or impossible, consider the intraosseous route for both
children and adults. The intraosseous route also enables withdrawal of marrow for venous
blood gas analysis and measurement of electrolytes and haemoglobin concentration.

6
Signs of life
• If signs of life (such as regular respiratory effort or movement) reappear during CPR,
or readings from the patient’s monitors (e.g. exhaled carbon dioxide or arterial blood
pressure) are compatible with a return of spontaneous circulation (ROSC), stop CPR
and check the monitors briefly.
• If an organised cardiac rhythm is present, check for a pulse. If a pulse is palpable,
continue post-resuscitation care, treatment of peri-arrest arrhythmias, or both. If no
pulse is present, continue CPR.
Post-resuscitation care
• Return of spontaneous circulation is just the first step towards the goal of complete
recovery from cardiac arrest. Interventions in the post-resuscitation period influence
the final outcome significantly.
• The post-resuscitation phase starts when return of spontaneous circulation is
achieved. Once stabilized, the patient should be transferred to the most appropriate
high-care area (e.g. intensive care unit or cardiac care unit) for continued monitoring
and treatment
