PULMONARY FUNCTION TEST(PFT)
Proff. Amjad Fawzi
2016Objectives
By the end of the present lab, students should be able to:• Define different lung volumes and capacities.
• Define, perform and interpret the SPIROMETRY test.
• Obtain some of the significant spirometric parameters(FVC,FEV1,FEV1%) and compare them with those of a typical person of the same gender, height and age.
• Differentiate between normal, obstructive, and restrictive pattern spirograms.
Introduction
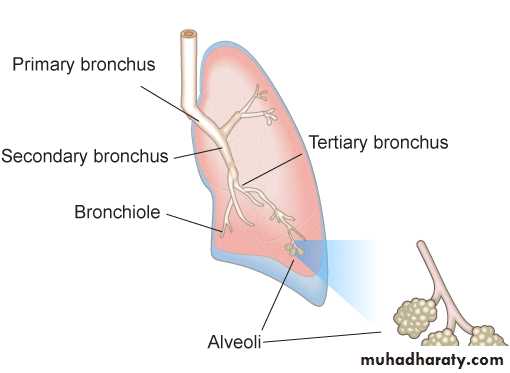
The efficiency of gas exchange between air and blood, which occurs in the alveoli, is dependent on ventilation (ulternating inflation and deflation of the lungs).The efficiency of ventilation, on the other hand, is dependent on the integrity of
airwaysalveoli
thoracic cage(bones and muscles)
respiratory control mechanisms.
Lung Volumes and Capacities
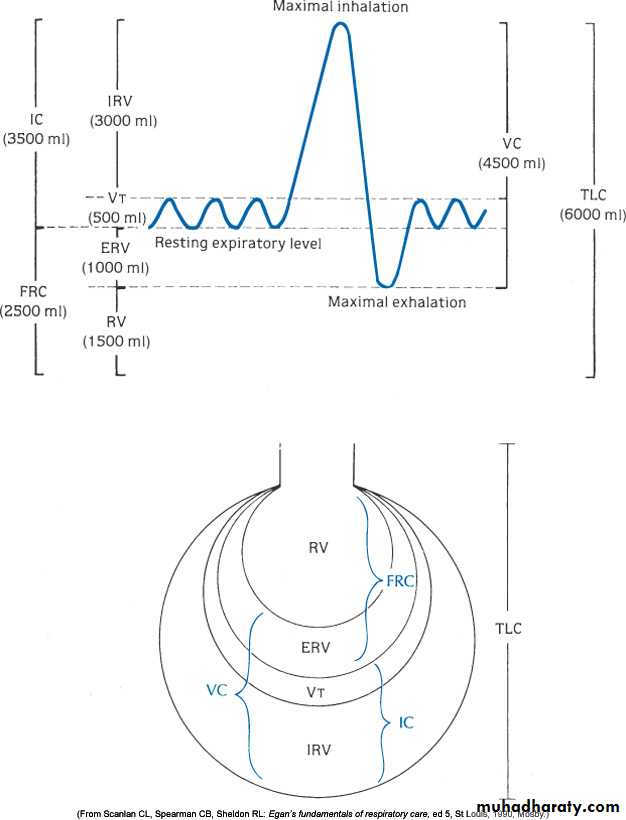
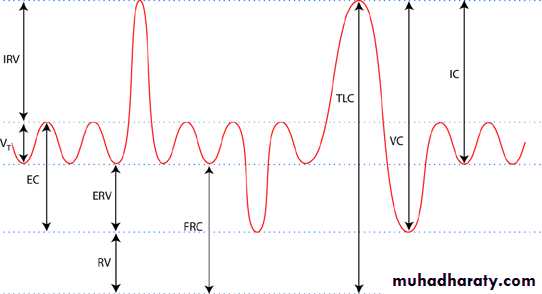
Volume of air that is moved in and out of the lung( ventilation) can be recorded by using the spirometer and the process called spirometry.Lungs volumes and capacities of are:
[1] The tidal volume (TV): Is the volume of air inspired or expired with each normal breath and it is about 500 ml in average young adult man.
[2] The inspiratory reserve volume (IRV): Is the extra volume of air that can be inspired over and beyond tidal volume and it is about 3000 ml.
[3] The expiratory reserve volume (ERV): Is the amount of air that can be expired after the normal tidal expiration, which is about 1100 ml.
[4] The residual volume (RV): Is the volume of air still remaining in the lungs after the most forceful expiration, which is about 1200 ml. This is important because it provides air in the alveoli to aerate the blood even between breaths.
This volume cannot be measured directly by spirometer. Therefore, an indirect method must be used usually the helium dilution method and body plethysmogrph.
Once the functional residual capacity (FRC) has been determined, the residual volume can then be determined by subtracting the expiratory reserve volume from the functional residual capacity, i.e. RV = FRC - ERV.
[5] The inspiratory capacity (IC) = TV +IRV = 500 +3000 = 3500 ml. This is the amount of air that a person cans breath beginning at the normal expiratory level and distending the lungs to the maximum amount.
[6] The functional residual capacity (FRC)= ERV + RV = 1100 + 1200 = 2300 ml. This is the amount of air remaining in the lungs at the end of normal expiration.
***[7] The vital capacity (VC)
The vital capacity (VC) = IRV + TV + ERV = 3000 + 500 + 1100 = 4600 ml.This is the maximum amount of air that a person can expel from the lungs after max filling.
VC can be decreased in restrictive lung diseases (paralysis of the respiratory muscles, pulmonary fibrosis) and may be normal in obstructive lung diseases (asthma, bronchitis, emphysema).
When the vital capacity is reduced to about 40% of normal, the patient feel breathless even with simplest movements.
[8] The total lung capacity (TLC) = VC + RV = 4600 + 1200 = 5800 ml. This is the maximum volume to which the lungs can be expanded with the greatest possible inspiratory effort.
All pulmonary volumes and capacities are
about 20-25% less in women than men
greater in large athletic persons that in small and asthenic persons.
Pulmonary volumes and capacities change with the position of the body, most of them decreasing when the person lies down and increasing on standing, this change with position is caused by two factors:
[A] - a tendency for the abdominal contents to press upward against the diaphragm in the lying position.
[B] - an increases in the pulmonary blood volume in the lying position, which correspondingly decreases the space available for pulmonary air.
PFT includes:
Test for ventilation (SPIROMETRY).
Test for gas exchange(lung diffusing capacity-Dlco).
Blood gas analysis.
Exercise test.
Special tests like bronchodilator test, PFT for children…..
Spirometry is used for:
Check upRotine health check up.
Physical fitness for certain jops(eg. Military).
Preoperative.
Diagnosis of lung diseases
Obstructive lung disease(asthma and chronic bronchitis).Restrictive lung disease(pulmonary fibrosis).
Follow up of treatment in chronic lung diseases.
Spirometry (measurement of breath)The most common PFT.
It measures the volume and/ or the flow of air that can be inhaled and exhaled.
Spirometry is becoming more and more important, as respiratory diseases are increasing word wide.
Studies suggest that Chronic Obstructive Pulmonary Disease (COPD) could climb to be the 3rd leading killer by 2020.
Most COPD cases are completely avoidable; 85-90% of cases are caused by tobacco smoking.
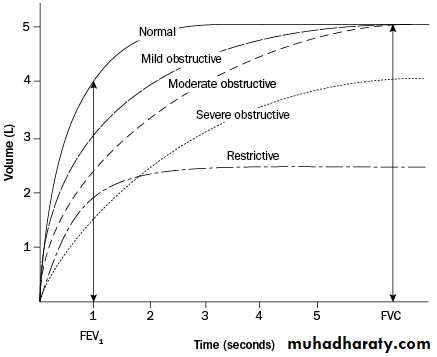
Classification of Lung DefectsOBSTRUCTIVE
Expiratory flow is below normal(reduced FEV1%)
Diseases:
Bronchitis
Asthma
Emphysema
RESTRICTIVE
Lung volumesare reduced(eg. FVC)Diseases:
Neuromuscular disease
Cardiovascular disease
Pulmonary fibrosis
Obesity
Development of Spirometry
The water spirometer measuring vital capacity was developed by a surgeon named John Hutchinson, in 1846.
Spirometer was then developed into dry types.
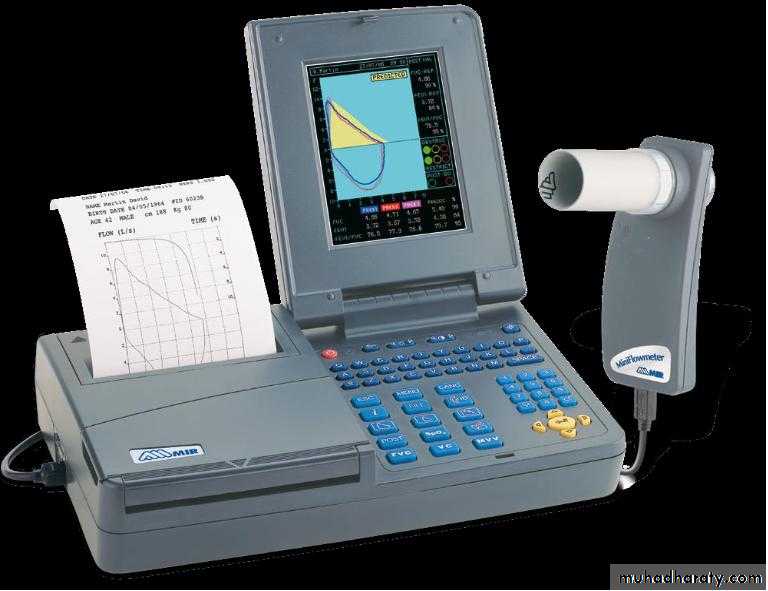
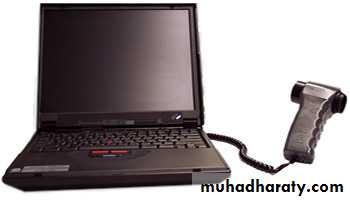
eg. VitalographModern Spirometers*Computer based*More accurate
Modern, computer based
spirometerTurbine
Whole body plethysmograph
more accurate measurement for the all lung volumes.In resting adult, the normal rate of breathing (breaths/minute or BPM) is approximately 15 .
15 X VT = minute ventilation (ml/min)…...the amount of air exhaled in one minute of breathing.
The volume of air remaining in the lungs after a full expiration, (residual volume RV), cannot be measured by spirometry because volunteer is unable to
exhale any further.
RV is can be measured by:
Gas dilution method
Body Plethysmography
Normal Values of PFT
Depends on the following factors:
Height
Weight
Age
Gender
Race
Effort dependent
Normal values is obtained from special charts(NOMOGRAM) or special prediction equation depending on hight,weight and gender.
SUBJECTS, APPARATUS AND PROCEDURE
SubjectsPre-test instructions and demonstration.
Apparatus
Use Spirometer to obtain the (forced expiratory flow measurements(FVC,FEV1,FEV1%).
Spirometer chart(spirogram).
Nose clip.
Tape measure(measurement of body hight).
Balance(measurement of body weight)
Nomogram chart to obtain the normal predicted value of FVC depending on high(Cm) and age(years) in order to compare it with the measured value.
Contraindication
Recent abdominal, thoracic, or eye surger
Symptoms of acute or severe illness
Chest pain, nausea, vomiting, high fever, dyspnea
Pneumothorax
Recent history of abdominal, thoracic, or cerebral aneurysm
Patient Instructions Prior to Testing
Should not smoke at least one hour before testDo not eat a large meal two hours prior to test
No vigorous exercise 30 minutes before test
Do not wear tight form fitting clothes
May need to remove loose dentures for test
Should wait at least one month post MI
Stop bronchodilators, corticosteroids
Procedure of Forced expiration maneuver
Ask the subject to take max inspiration then followed by a single as forceful and as deep as possible expiration(from TLC to RV).Subjects should wear nose clip. Repeat each test three times in order to choose the best trial.
Spirogram
MEASUREMENTS AND CALCULATIONS
2.Obtain the FVC from the spirogram.Correct the FVC from ATPS(ambient temperature and pressure saturated with water vapour) to BTPS ( body temperature and pressure saturated with water vapour) by multiplying it with the correction factor obtained from special chart depending on lab. temperature.
Temp.ºC Corr.factor
16 1.123 21 1.097 26 1.069 31 1.03917 1.118 22 1.091 27 1.063 32 1.033
18 1.113 23 1.086 28 1.057 33 1.026
19 1.107 24 1.080 29 1.051 34 1.020
20 1.102 25 1.074 30 1.045 35 1.013
Conversion from ATPS to BTPS conditions
Compare the corrected FVC with the predicted FVC obtained from the nomogram (depending on age , height and gender).Normal measured values differs from the predicted ideal values by about( ±10-15%).
In restricted lung disease(eg. Pulmonary fibrosis)
FVC is decreasednormal FEV1%.
In obstructive lung disease(eg. Asthma)
FVC may be normal
Decreased FEV1%.
Obtain the FEV1 from the spirogram.
Calculate the FEV1%from the following equation:FEV1%= FEV1/FVC X100