PERIPHERAL VASCULAR DISEASE
ABDULAMEER M. HUSSEINFICMS, FACS
Peripheral arteries
• Arteries outside of chest and abdomen• Diseases
• Occlusive [OAD]
• Aneurysmal
• Inflamatory
• Others
WHAT IS THE PERIPHERAL VASCULAR SYSTEM?
• The veins and arteries in the arms, hands, legs and feet• Peripheral arteries supply oxygenated blood to the body
• Peripheral veins brings deoxygenated blood from the capillaries in the extremities back to the heart.
> for Intravenous therapy, it is the most common access for a peripheral intravenous (IV) line
DIFFERENCE BETWEEN PVD AND PAD
Peripheral Vascular Disease (PVD)
- There are problems altering the blood flow through both the arteries and veins.
Peripheral Artery Disease (PAD)
- is a type of PVD
- have problems only with arterial blood flow
Only 1 in 10 of thèse patients has classical symptômes of intermittent claudication (IC)
1 in 5 people over 65has PAD†
† ABI<0.9
Two types of PVD
FunctionalDoesn’t have an organic cause.
Doesn’t involve defects in blood vessels’ structure, usually short-term effects and come and go.
Ex: Raynaud’s disease.
Organic
Caused by structural changes in the blood vessels, such as inflammation.
Ex: Peripheral artery disease, caused by fatty buildups in arteries.
• Causes
• Atheromatous
Risk Factors• Smoking
• Diabetes
• Hypertension
• Overweight
• Inactive (sedentary) lifestyle
• Positive family history
• Hyperlipidemia
• Advanced age
• Inflammatory
• Trauma
• Structural defects
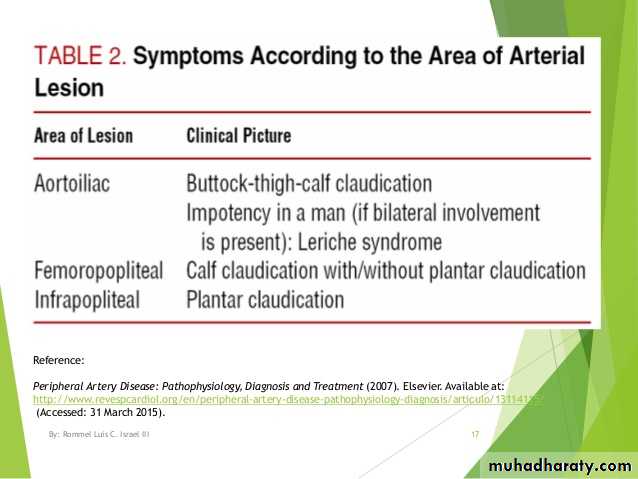
SYMPTOMS
depend on:• What artery is affected
• How severely the blood flow is reduced
1. Claudication (dull, cramping pain in hips, thighs or calf muscle)
2. Numbness or tingling in leg, foot or toes
3. Changes in skin color (pale, bluish or reddish discoloration)
4. Changes in skin temperature, coolness
5. Impotence
6. Infection/sores that do not heal
7. Ulceration or gangrene
8. Uncontrolled hypertension (high blood pressure)
9. Renal failure
Clinical presentation
Stage
Clinical
I
Asymptomatic
IIa
Mild claudication
IIb
Moderate to severe claudication
III
Ischemic rest pain
IV
Ulceration or gangrene
Critical limb ischemia
Fontaine classificationComparison of characteristics of Arterial & Venous Disorders
• Arterial Disease
• Venous Disease
• Skin
• cool or cold, hairless, dry, shiny, pallor on elevation, rubor on dangling
• warm, though, thickened,
• mottled, pigmented areas
• Pain
• sharp, stabbing, worsens w/ activity and walking, lowering feet may relieve pain
• aching, cramping, activity and walking sometimes help, elevating the feet relieves pain
• Ulcers
• severely painful, pale, gray base, found on heel, toes, dorsum of foot
• moderately painful, pink base, found on medial aspect of the ankle
• Pulse
• often absent or diminished
• usually present
• Edema
• infrequent
• frequent, esp. at the end of the day and in areas of ulceration
Investigations
GeneralCBP, FBS, RFT, LIPID PROFILE, ECG, ECHO
To localise and to plan intervention
Ankle Brachial Index (ABI)
Ultrasound Doppler Test
CT/MR ANGIOGRAPHY
Angiogram
Management
• Medical
• Graded exercises
• Aspirin
• Lipid lowering drugs
• Cilostazol
• Pentoxifylline
• Foot care
• Stop smoking
• Aggressive control of co-morbid diseases
MANAGEMENT
Non-invasive interventions1. Exercise and diet
Exercise• Supervised exercise programs to improve walking time and walking distance
• walk until pain is felt, take a rest until the pain subsides (For 3x a week, repeat this cycle to a total of 30 minutes, and progress to 60 minutes per day)
Diet
- low salt
- low fat
Non-invasive interventions
2. Positioning
- avoid crossing of legs (interferes blood flow)- elevate feet at rest (manages swelling)
> not above the heart level
> extreme elevation slows arterial blood flow
3. Promoting Vasodilation (increasing the diameter of blood vessels)
- provision of warmth to the affected extremity> maintain a warm environment at home
> wear socks or insulated shoes at all times
> Never apply direct heat to the limb (heating pad or extremely hot water) to reduce the risk of burns
TREATMENT
• Non-invasive interventions4. Avoid exposure to cold temperatures
5. Avoid or limit intake of caffeine- causes vasoconstriction.
6. Medications
- Given to patients with chronic PVD
> Antiplatelet medications (such as Aspirin and Plavix)
> Lipid lowering agents
> Cilostazol(a phosphodiesterase III inhibitor)
> Angiotensin converting enzyme inhibitor (ACEI)
> Calcium channel blockers
7. Hypertension - Controlling high blood pressure can improve blood flow through the blood vessels and reduce the constriction
8. Smoking cessation
- improvement of walking distance- 5 year survival rate is doubled
- Post-operative complications is reduced
9. Little evidence to support for the role of complementary therapies:
- vitamin E
- garlic
Indications for intervention
1. Disabling claudication2. Rest pain
3. Tissue loss
intervention
• Endovascular1.Angioplasty
2.Stenting3. Atherectomy
• Surgical
1. Bypass
2. Endarterctomy
3. Embolectomy
• Amputation
4.Thrombolytic Therapy5. Stent-Grafts
Endovascular
1. Angioplasty2. Stents
3. Atherectomy
- a minimally invasive intervention procedure
- excision and removal of blockages by catheters with miniature cutting systems.During these procedures: -the physician will periodically inject a contrast dye- x-ray pictures are taken to determine whether or not the artery is sufficiently open.
4.Thrombolytic Therapy
5.Stent-GraftsSurgery
-If blockage is extremely long
- If blockage has become very hard and calcified with time- If blockage may be resistant to atherectomy or angioplasty and stents
Purpose:
> to bypass the problem area.
Surgical intervention in – advanced disease
– ischemic changes and- pain severely impairs activity
Embolectomy
removal of a blood clot, done when large arteries are obstructed
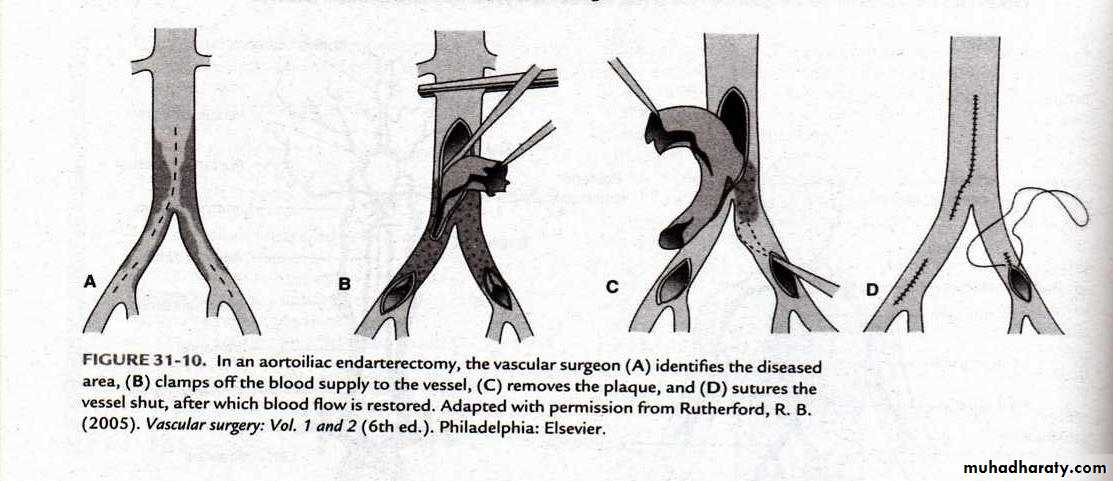
Endarterectomy
is removal of a blood clot and stripping of atherosclerotic plaque along with the inner arterial wall.
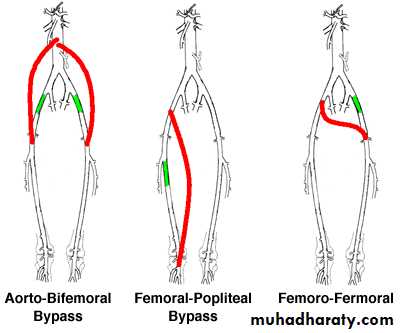
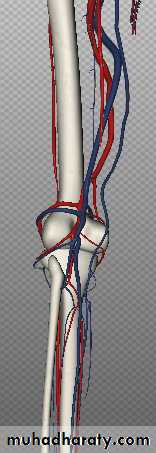
Arterial by-pass surgery
an obstructed arterial segment may be bypassed by using a prosthetic material (Teflon) or the pt’s. own artery or vein (saphenous vein)
Endarterectomy
Bypass
BypassConduits
1. Autogenoussaphenous vein
2. Synthetic
PTFEDACRON(polyester)
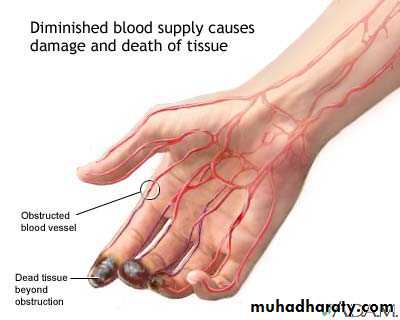
Amputation
• With advanced atherosclerosis & gangrene of extremities• Toes are the most often amputated part of the body
• The surgical goal is the remove the least amount of tissue possible and create a stump adequate for the fitting of a prosthesis
Post – operative care for arterial surgery
pt. is monitored for signs of circulation in the affected limb and interventions done to promote circulation & comfort• Assess and report changes in skin color and temperature distal to the surgical site, every 2-4 hrs.
• assess peripheral pulses
• sudden absence of pulse may indicate thrombosis
• mark location of pulse with a pen to facilitate frequent assessment
• use a dapper if pulse in difficult to palpate
• assess wound for redness, swelling and drainage
• promote circulation
• reposition pt. every 2 hrs.
• tell pt. not to cross legs
• encourage progressive activity when permitted
• medication with analgesics to reduce pain
Arterial by-pass surgery
Post-operative care• assess sensation and movement of the limb
• monitor extremity for edema
• monitor & report signs of complications – increase pain, fever, limitation of movement or paresthesia
• avoid sharp flexion in the area of the graft to prevent decreased circulation to the graft.
Outcome
Major cause of mortality in PVD is cardiac and cerebrovascular disease
Thromboangitis Obliterans ( Buerger’s Disease)
• Characterized by acute inflammatory lesions and occlusive thrombosis of the arteries & veins• Has a very strong assoc. with cigarette smoking
• Commonly occurs in male – bet. 20-40 y.• Usually affect the lower leg. toes, feet
• May involve the arteries of the upper extremities (wrists)Clinical Manifestation
• Intermittent claudication in the arch of the foot• Pain during rest – toes
• Coldness – due to persistent ischemia
• Paresthesia
• Pulsation in posterior tibial, dorsalis pedis – weak or absent
• Extremities are red or cyanotic
• Ulceration & gangrene are frequent complications – early can occur spontaneously but often follow trauma
Thromboangitis Obliterans
management
• Advise the person to stop smoking• vasodilators
• Prevent progression of disease
• Avoid trauma to ischemic tissues
• Relieve pain
• Provide emotional support
• Whiskey or brandy may be of some value during periods of exacerbations vasodilation
• Advise pt. to avoid mechanical, chemical or thermal injuries to the feet
• Amputation of the leg is done only when the ff. occurs:
gangrene extends well into the foot
pain is severe and cannot be controlled
severe infection or toxicity occurs
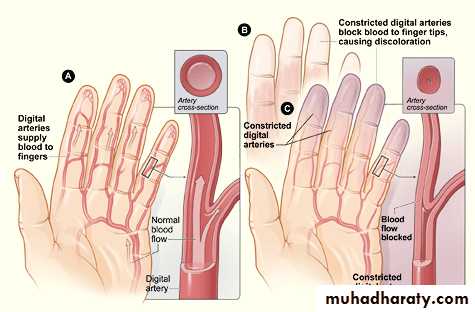
Raynaud’s phenomenon
• Refers to intermittent episodes during which small arteries or arterioles of L and R arm constrict (spasm) causing changes in skin color and temperature• Generally unilateral and may affect only 1 or 2 fingers
• May occur after trauma, neurogenic lesions, occlusive arterial disease, connective tissues disease
• Charac. by reduction of blood flow to the fingers manifested by cutaneous vessel constriction and resulting in blanching (pallor)
Raynauds’ Disease
• unknown etiology, may be due to immunologic abnormalities
• common in women 20-40 y.
• maybe stimulated by emotional stress, hypersensitivity to cold, alteration in sympathetic innervation
Raynauds’ Disease
Clinical Manifestations• Usually bilateral –(both arms or feet are affected)
• During arterial spasm – sluggish blood flow causes pallor, coldness, numbness, cutaneous cyanosis and pain• Following the spasm – the involve area becomes intensely reddened with tingling and throbbing sensations
• With longstanding or prolonged Raynaud’s disease – ulcerations can develop on the fingertips and toes
Raynauds’ Disease
Medical Management
• Aimed at prevention
• Person is advised to protect against exposure to cold
• Quit smoking
• Drug therapy –
• Calcium channel blockers, vascular smooth muscle relaxants
• Vasodilators – to promote circulation and reduce pain
• Sympathectomy ( cutting off of sympathetic nerve fibers)
to relieve symptoms in the early stage of advanced ischemia
• If ulceration/gangrene occur, the area may need to be amputated
Acute limb ischemia
Abulameer M. HusseinDefinition
• Sudden interruption of arterial blood supply the with no time for collateral to form .• The extent of ischemia & final outcome depends upon
• 1. Size & location of clot
• 2. Extent of collateral circulation
• 3. Time between onset of occlusion & treatment
Causes of acute arterial ischemia
• An arterial embolus - most common cause heart as a source - 70 %
• Thrombosis on an atheromatous plaque
• Thrombosis of an aneurysm
• Arterial dissection
• Traumatic disruption
• External compression e.g cervical rib , popliteal entrapment
Arterial embolus
• Abnormal undissloved material carried in the blood stream from one part of vascular system to impact in distance part .• Types
• 1-Thrombus
• It is the thrombus that dislodged from its source & circulate in blood stream & impact in BV
• 2-Air
• 3-Fat
• 4-Neoplastic
• Common source is mural thrombus that follow MI, mitral stenosis & aneurysm
• Emboli tend to lodge at bifurcation of vessels
• Large emboli straddling in aortic bifurcation Lower limb ischemia
Trauma
• Could be• 1. Penterating
• 2. Blunt
• 3. Iatrogenic
• Commonly in femoral or brachial artery at arterial catheterization
Symptoms and Signs ( Ps )
• Symptoms
• Painless ( numbness )
• Pain
• Paraesthesiae
• Paralysis
• Signs
• Pallor
• Pulslessness
• Perishingly cold to the touch
• * Muscle tenderness is bad diagnostic especially in muscle of anterior & posterior compartment of the calf
Physical Examination
• Heart rhythm:• Presence of atrial fibrillation or other arrhythmias
• Apex beat (ventricular aneurysm)
• Auscultation for evidence of valvular disease
• Inspection of limbs:
• Pallor of the skin
• Tense, tender calf with impaired dorsiflexion (compartment compression)
Physical Examination
• Venous guttering:
• Veins are so empty to appear as shallow grooves or gutters
• Buerger’s test: rapid pallor as arterial supply is poor.
• Delayed capillary refill.
• Skin temperature: a difference of as small as 1˚C can be ascertained.
Physical Examination
• Absent peripheral pulses:• Important to delinate a blockage in the arteries (e.g. presence of femoral pulse and absent distal pulses indicate superficial femoral block.
• Ankle brachial pressure index (ABPI)
• It is the ratio of pressure at foot pulse to that at the brachial artery. < 0.5 indicate significant ischemia.
complication
• Leg become mottled & marbled• Muscle hardness
• Skin become blister
• Gangrene which usually start in toes before spreading distally
Differential Diagnosis
• Arterial embolus• Acute arterial thrombosis
• Thrombosed aneurysm
• Aortic dissection
• Traumatic arterial disruption
• Cervial rib
• Acute venous thrombosis
• Spinal cord compression or infarction
Investigation
• Critical ischemia needs investigating with great urgency to relieve the patient’s pain and to prevent irreversible damage.
• They include:
• Duplex ultrasonography
• C-T Angiography
• Arteriography
• ECG to exclude associated coronary diseases
• Serum cholesterol: raised in atherosclerosis
• Urine for sugar and blood glucose: to exclude DM
Therapeutic Strategies in Acute Ischemia
Most common vascular emergency1. Intra arterial thrombolysis
2. Thrombo-aspiration with catheter
3. Mechanical thrombolysis
4. Surgical Embolectomy – Fogarty catheter
Initial treatment
• Ischaemia beyond 6 hours is usually irreversible and results in limb loss.• Stasis may cause a thrombus to extend distally and proximally to the embolus.
• The immediate administration of 5000 U of heparin intravenously can reduce this extension and maintain patency of the surrounding (particularly the distal) vessels until the embolus can be treated.
• IV fluid
• Analgesia
Thrombolysis
• At arteriography :, a narrow catheter is passed into the occluded vessel and left embedded within the clot.
• Tissue plasminogen activator (TPA) is infused through the catheter and regular arteriograms are carried out to check on the extent of lysis, which, in successful cases, is achieved within 24 hours.
• The method should be abandoned if there is no progression of dissolution of clot with time.
Contraindications to thrombolysis
recent stroke
bleeding diathesis
Pregnancy
results in those over 80 years old are poor.
OPERATIVE TREATMENT
Embolectomy• Local or general anaesthesia may be used.
• The artery (usually the femoral), bulging with clot, is exposed and held in slings.
• Through a longitudinal or transverse incision, the clot begins to extrude and is removed, together with the embolus
• Fogarty balloon catheter is introduced both proximally and distally until it is deemed to have passed the limit of the clot.
• Postoperatively, heparin therapy is continued until long-term anticoagulation with warfarin is established.
Compartment syndrome
Reduced organ / tissue perfusion as a result of increased intracompartmental pressureHappen in tight compartments
Results in vicious cycle of ischemia and swelling and eventual muscle death
peripheral Vascular TraumaMechanism
BluntOrthopaedic #
Dislocation (knee)
Isolated
Penetrating
High velocityLow velocity
Iatrogenic
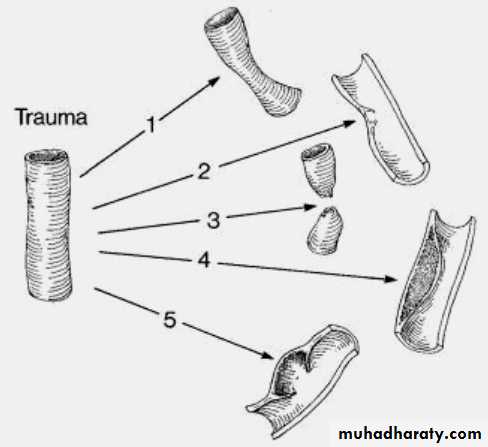
Types arterial damage• Spasm (or compression)
• Intimal injury
• Transection
• Intramural haematoma
• Pseudoaneurysm
Presentation
1.Bleeding / haematoma2.Ischaemia
3.Complications of vascular injury (Refer later)Complications
Ischemia reperfusion injuryCompartment syndrome
Arteriovenous fistula
False aneurysm
Death
Immediate treatment
• Control bleeding• Replace volume loss
• Cover wounds
• Reduce fractures/dislocations
• Splint
• Re-evaluate
•
Signs of arterial injury hard signs
1.External (arterial bleeding)2.Rapidly expanding haematoma
3.Palpable thrill/audible bruit
4.Obvious ischaemia
5 P’s
Index of suspicion soft signs
1. History of arterial bleeding2. Proximity of # / wound to artery
3. Diminished pulse (BP)
4. Small non-pulsatile haematoma
5. Neurologic deficit
6. Hypotension
Immediate referral
Hard signsImmediate (vascular) surgery referral
Early transfer to theatreImmediate exploration
Soft signs, other injuries
1. Resuscitate2. Apply compression
3. immobilize
4. Reduce
5. Reassess
asymmetry
Consult
Problems with diagnosing distal ischaemia after trauma
1.paincould be due to injury itself, may not have pain due to associated nerve injury
2.pallor
may be pale due to blood loss
3. Absent pulse
may be absent due to low blood pressure. Compare with other limb.
4.paresthesia , paresis
may occur due to associated nerve, muscle injury or unresponsive confused patientDoppler
No signal = no perfusionSignal ≠ normal arteries
Investigations
Caution ….No signal = no perfusion
Signal ≠ normal arteries
Investigations
2. Duplex scan3. CT ANGIOGRAPHY - Helps to locate, to assess the extent of injury, to identify associated injuries and to plan the treatment.
4. On table angiography - in cases needing urgent exploration and having multilevel injuries. i.e trap gun injury
In hospitals wherefacilities for repair is not available
Urgent transfer after stabilizing ABCDEFASCIOTOMY
Operative managementAngiography
In theatre
Diagnostic
Therapeutic
Covered stent
Embolization
Open exploration
Repair
Bypass
Operative strategy
PositionAccess
Angio
Maintain compression
Exposure & ControlSeparate (anatomical) incision
Distal
Damage limitation
intraoperative shuntProcedure
ThrombectomyHeparinize
Multisystem trauma
Coagulopathy
Repair deficit
• Lateral suture
• Resection and end-end• Interposition
• autologous vein
• Synthetic
• Ligation
Venous trauma
Repair (vs ligation)Popliteal
Massive soft tissue injury
Large veins
Key steps
Direct pressure
Subtle signsEarly transfer to theatre
Angiogram
Endovascular
Open
Fasciotomy
Ischemic and Reperfusion injuries
During ischemiaAnaerobic metabolism – lactic acidosis
Reduced ATP – reduced activity of ion pump – accumulation of intracellular Ca2+, Na+ and other ions, increased permeability
Ca2+ - activation of phospholipases and proteases
Activation of Xanthine oxidase
Increased membrane adhesiveness and Stasis leading to prothrombotic effects
Ischemic and Reperfusion injuries
Local
Influx of O2 and cells
resulting in production of oxygen radicals
Adhesion of cells leading to congestion and edema
Systemic
Acidosis
Acute kidney injury
ARDS
Hyperkalemia
Hypotension
DIC