Dr: Nibal Lec:1
Neurology
MENINGITIS
Total :38
Lec : 1
Dr: Nibal Lec:1
Dr: Nibal Lec:1
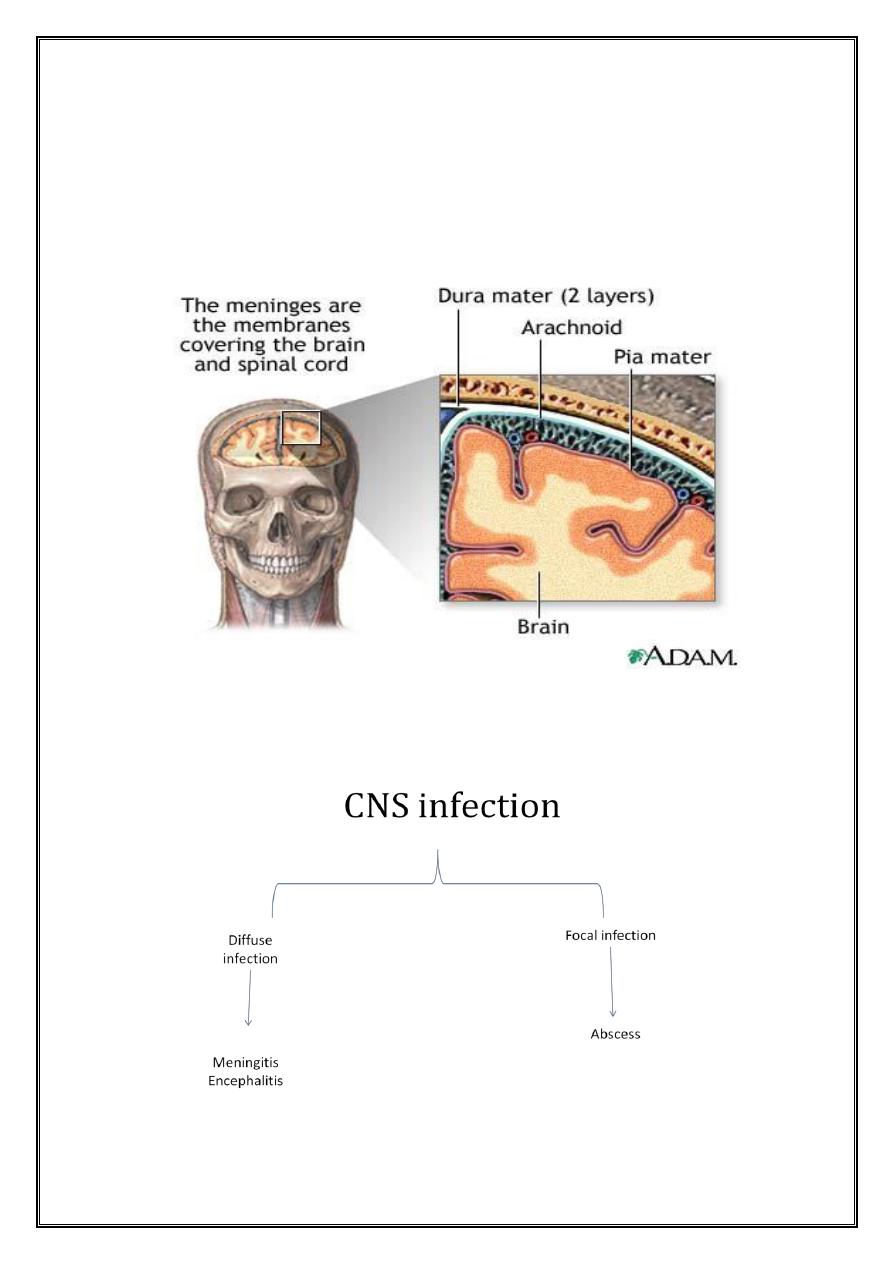
Central Nervous System Infection
Dr Nebal Waill
Pediatric neurology unit
CWTH
Viral infection > Bacterial > Fungal & parasitic > Ricketsial
Dr: Nibal Lec:1
Acute bacterial meningitis
Clinical scenario 1
5-month old infant brought by her parent to the outpatient clinic for fever of 7
days duration that did not respond to oral antibiotics prescribed by the physician. The
mother thought that her baby is not as active and playful as before and her feeding was
reduced. On examination you found that she was feverish and had bulging of fontanel.
Clinical scenario 2
13-month old female child who had history of fever with runny nose of 2 days
duration. Her mother brought her because she developed funny movements in her
arms and legs during which her baby was not responding. She thought that was fit
because she is aware of that as her older brother had history of febrile convulsion.
That occurred twice with 30 minutes apart. When you examined her you found
irritable baby with facial weakness [right side] and paucity of movement of the right
arm and leg. That part of the limbs was spastic. Her fontanel was closed
Clinical scenario 3
6-year old boy presented to the ER for fever and headache during the previous 3
days. On examination his temperature was 38.7 degrees centigrade. There was neck
stiffness & Kernig’s sign was positive. Lumbar puncture was performed and the result
was [turbid fluid, sugar=40 mg/dl, protein=80mg/dl, cells= 125 (95% neutrophiles)].
CSF was sent for culture and you were informed that it takes 10 days to get the result.
What do you think about the proper management of this child?
Dr: Nibal Lec:1
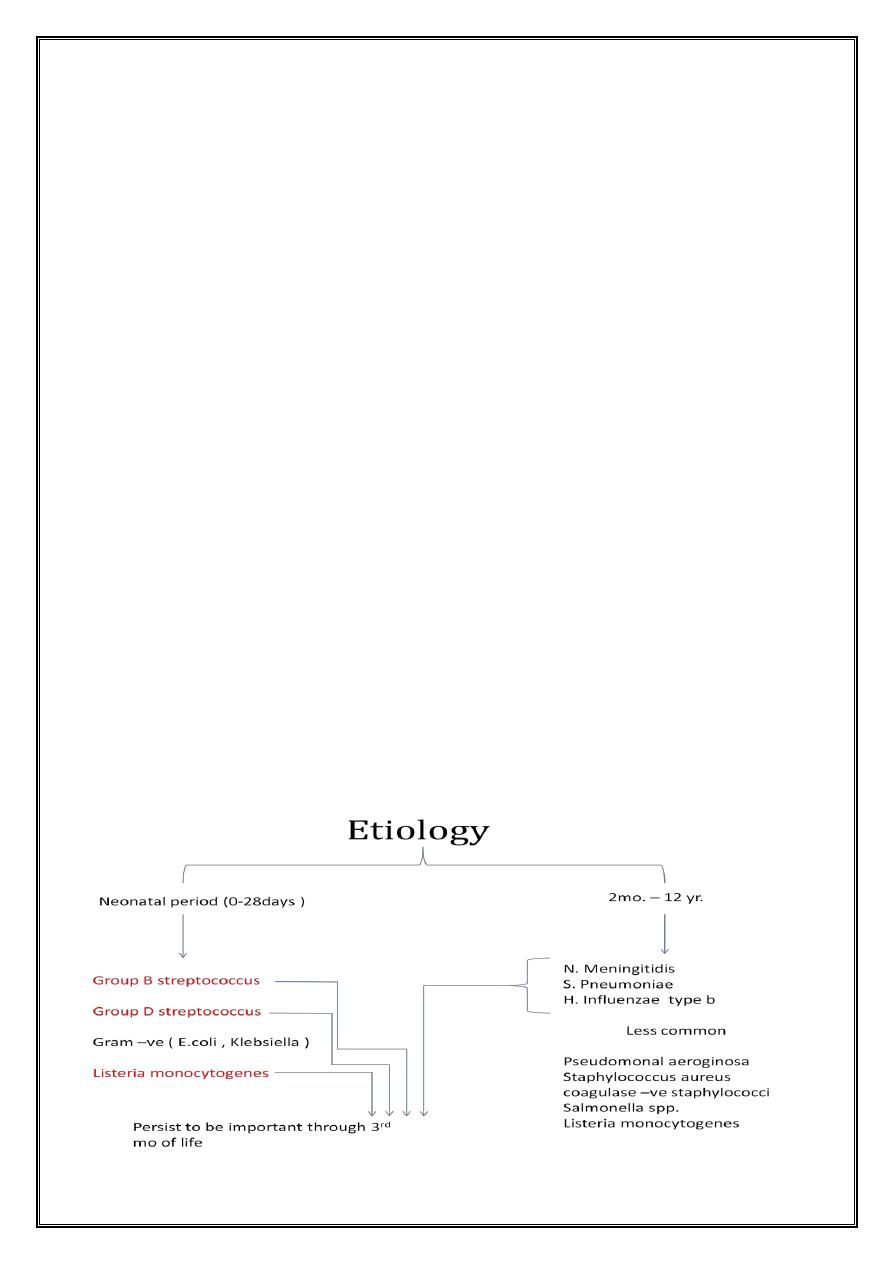
• S. pneumoniae & H. influenzae type b has become much less common in
developed countries since the introduction of universal immunization against
these pathogens beginning at 2 mo of age
• So these infection is considered in incompletely vaccinated individuals or those
in developing countries
Epidemiology
• Major risk factor for meningitis is the lack of immunity ( young age group )
• Recent colonization with pathogenic bacteria
• Close contact ( household, daycare centers , college dormitories ) with
individuals having invasive disease cause by N. meningitidis & H. influenzae
• Crowding
• Poverty
• Mode of transmission person-person through respiratory tract secretion or
droplets
Host defense defects
1. Altered Ig production (encapsulated bact.)
2. Complement system (C5-C8) ( meningococcus)
3. Asplenia ( pneumococcal , H. influenzae type b)
4. T-lymphocyte ( L. monocytogenes)
5. Congenital or acquired CSF leak across a mucocutaneous barrier ( cribriform
plate
6. Basal skull fracture into the cribriform plate ( pneumococcal meningitis )
7. Cochlear implants
8. Meningomyelocele ( staphylococcal , gram –ve )
9. CSF shunt infections ( staphylpcoccal esp. coagulase –ve )
Dr: Nibal Lec:1
Clinical manifestations
2 patterns:
1. Dramatic
2. Less commonly rapidly progressive ( of shock , DIC , purpura , level of
consciousenss , coma & death within 24 hr
Fever
Anorexia & poor feeding
Headache
Symptoms of URTI
Myalgias
Arthralgias
Tachycardia
Hypotension
Various cutenouse signs ( purpura , macular rash & petechiae )
ICP
Papilledema
Focal neurologic signs
Cranial neuropathies
Seizures
Alterations of mental status
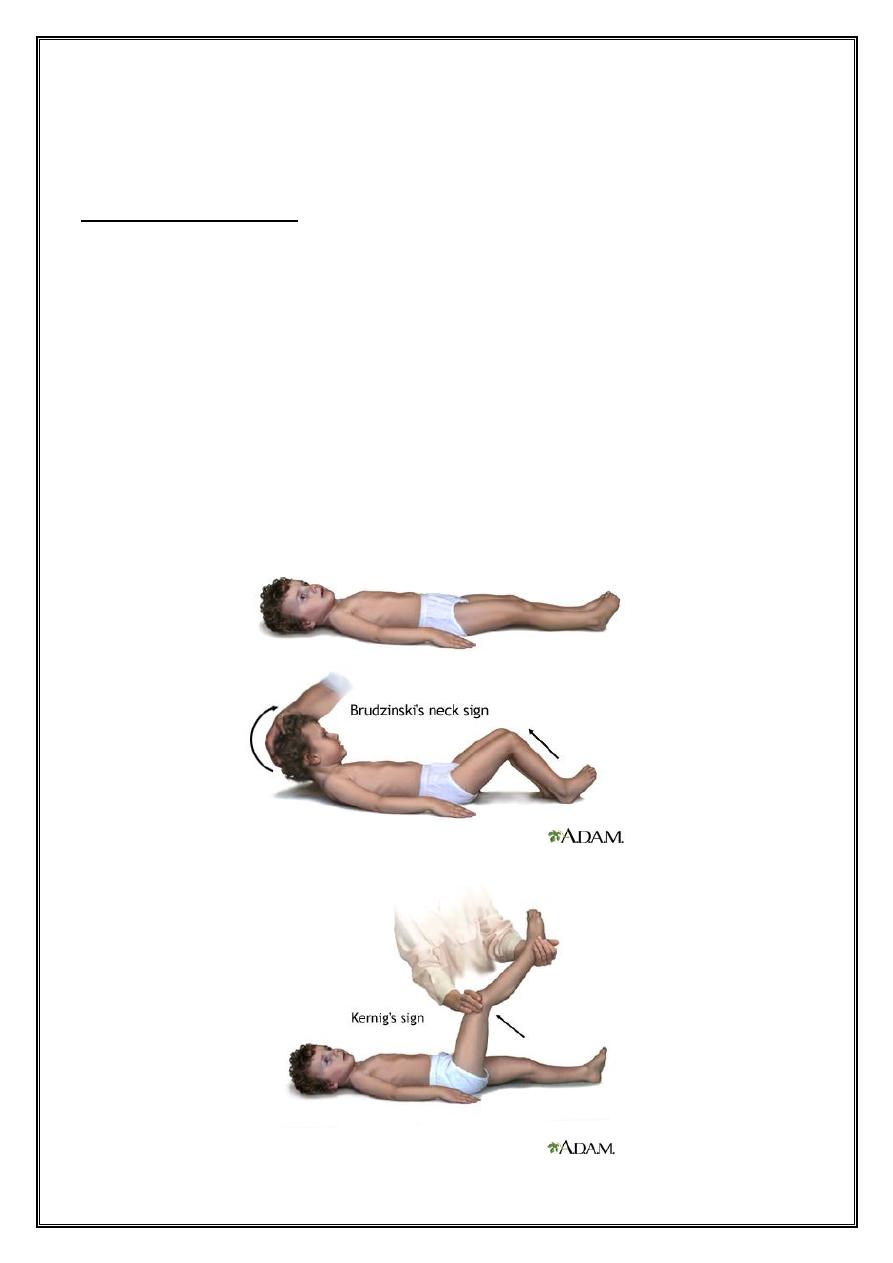
Meningeal irritation
Nuchal rigidity
Kernig sign
Brudzinski sign
Dr: Nibal Lec:1
Photophobia
Meningeal irritation signs
1. Nuchal rigidity
2. Back pain
3. Kernig sign ( flexion of the hip 90˚ with subsequent pain with extension of the
leg )
4. Brudzinski sign ( involuntary flexion of the knees and hips after passive flexion
of the neck while supine )
In some children particularly those younger than 12-18mo, kernig and brudzinski
signs are not consistently present
Dr: Nibal Lec:1
Fever , headache & nuchal rigidity are present in only 40% of adults with
bacterial meningitis
Increased ICP suggested by
1. Headache
2. Emesis
3. Bulging fontanel or diastasis of the sutures
4. Oculomotor ( anisocoria , ptosis )
5. Abducent nerve paralysis
6. HPT with bradycardia , apnea or hyprventilation
7. Decorticate or decerebrate posturing
8. Stupor , coma or signs of herniation
Papilledema is uncommon in uncomplicated meningitis and should suggest
1. a more chronic processes: presence of intracranial abscess
2. subdural empyema
3. occlusion of dural venous sinus
Focal neurologic signs due to vascular occlusion and occur in 10-20% of
children with bacterial meningitis
Cranial neuropathies ( ocular , occulomotor , abducent , facial and auditory
nerves ) may be due to focal inflammation
Dr: Nibal Lec:1
Seizures ( focal or generalized ) 20-30%
1. Cerebritis
2. Infarction
3. Electrolyte disturbances
• On presentation or within 1
st
4 days of onset = has no significant prognosis
• After the 4
th
day of illness and difficult to treat = poor prognosis
Alteration of mental status may be due to :
1. Increased ICP
2. Cerebritis
3. Hypotension
C/F
1. Irritability
2. Lethargy
3. Stupor
4. Obtundation
5. Coma
Diagnosis
• Lumbar puncture ( CSF analysis )
• Blood cultures ( 80-90% +ve )
• CT or MRI of brain
• Serologic tests
• Rarely brain biopsy
Dr: Nibal Lec:1
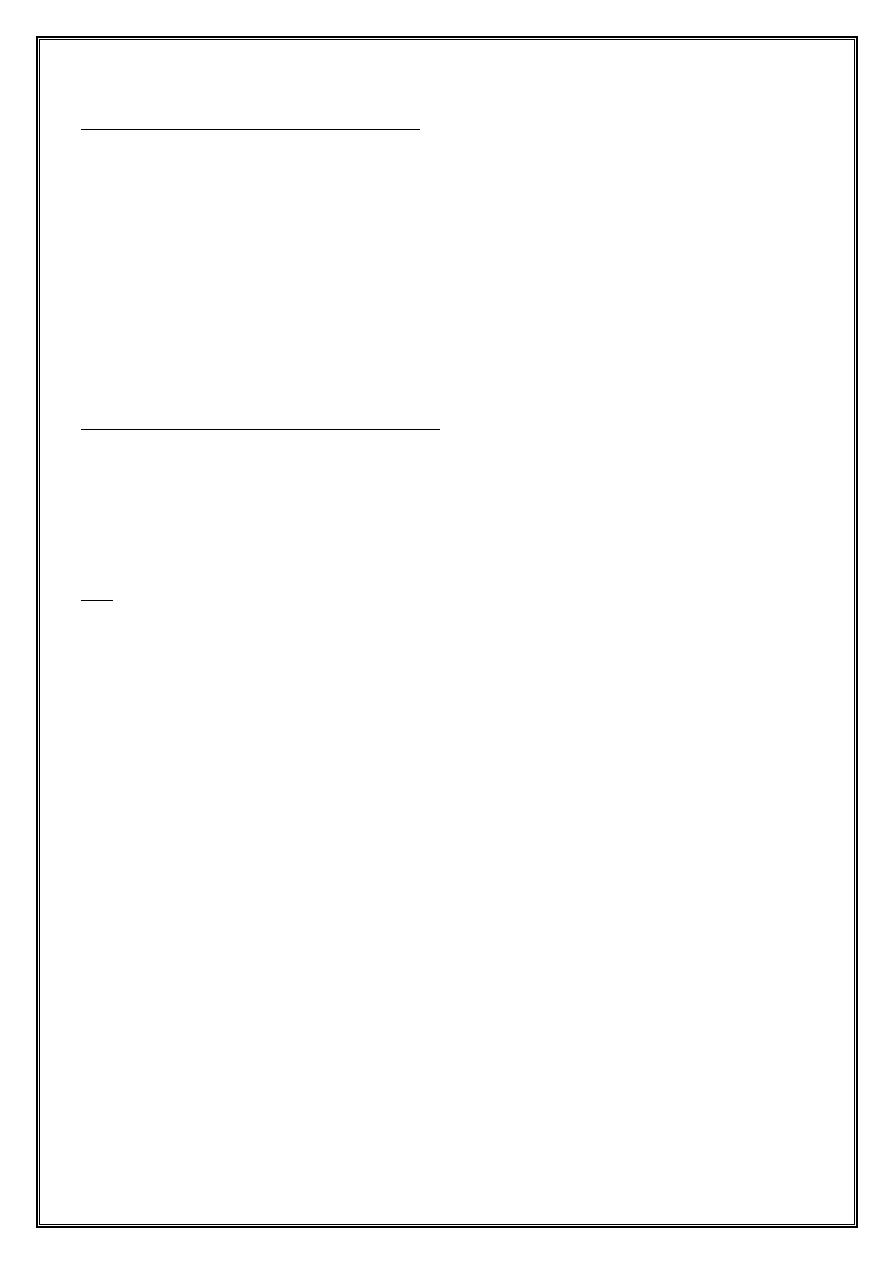
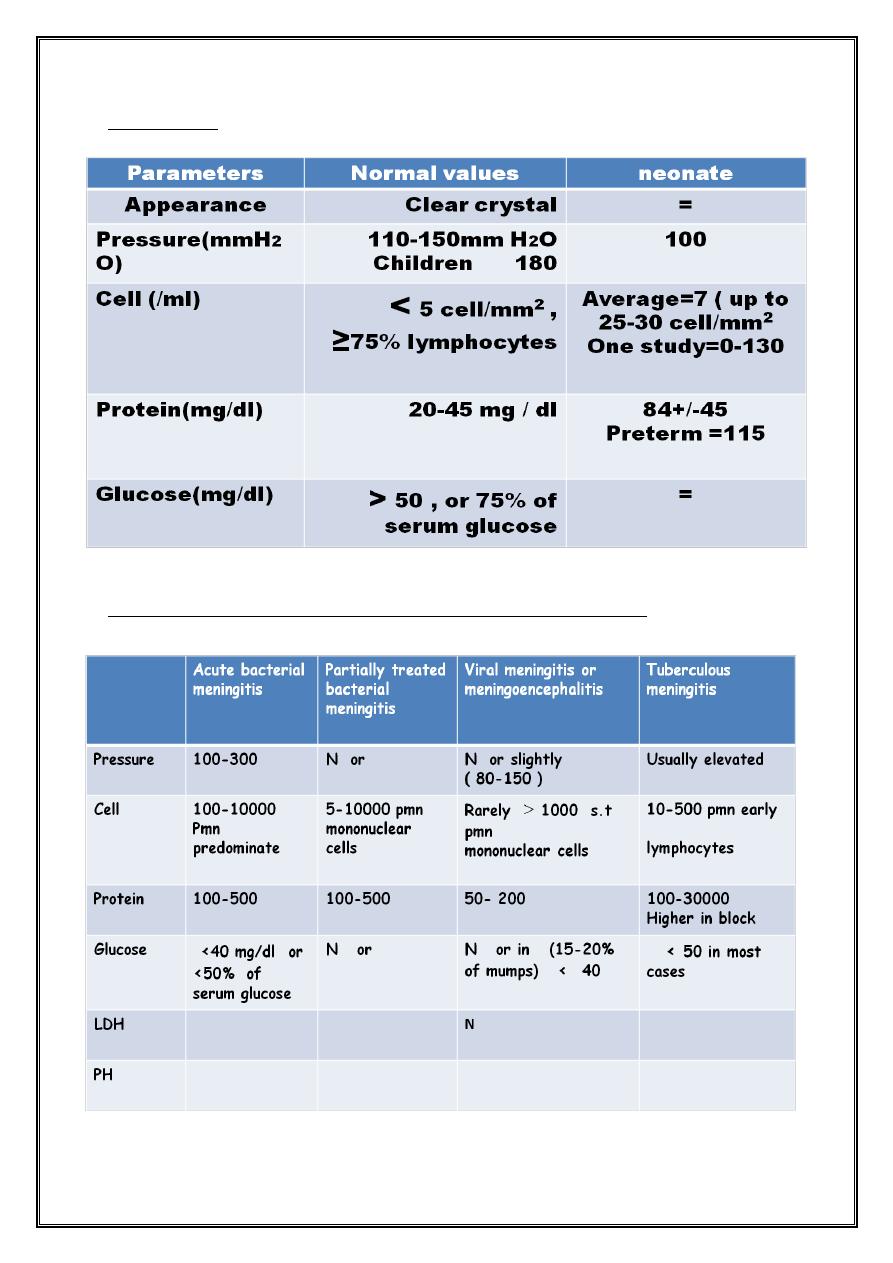
CSF analysis
Cerebrospinal fluid findings in central nervous system disorders
Dr: Nibal Lec:1
Indications of neuroimaging
• Signs of increase ICP
• Focal neurologic deficit
• Prolonged fever
• Increase head circumference
• Suppurative parameningeal lesions
Treatment
• Rapidly progressing disease + no signs of ICP = give AB after performing LP
• Signs of ICP = give AB before LP & obtain brain CT scan
1. AB
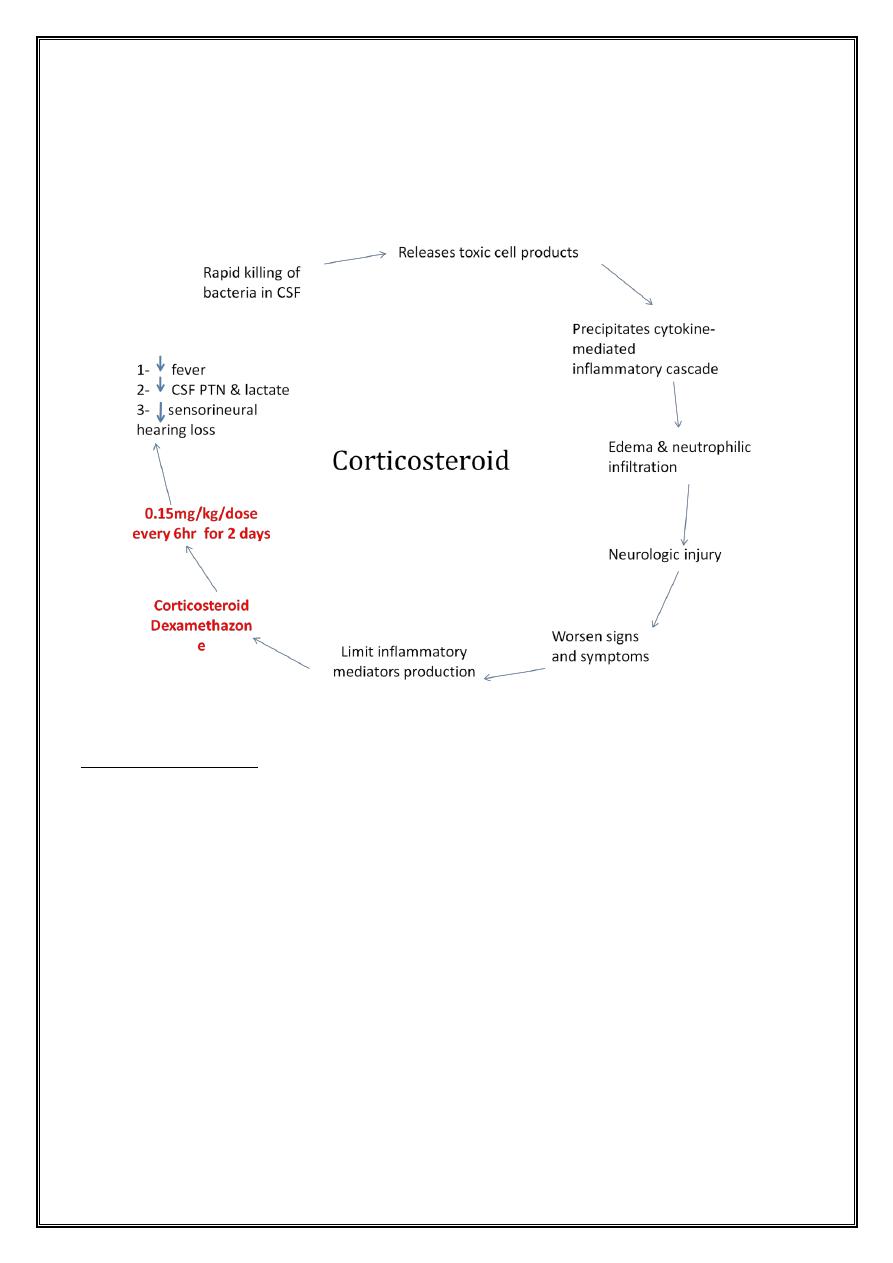
2. Corticosteroid
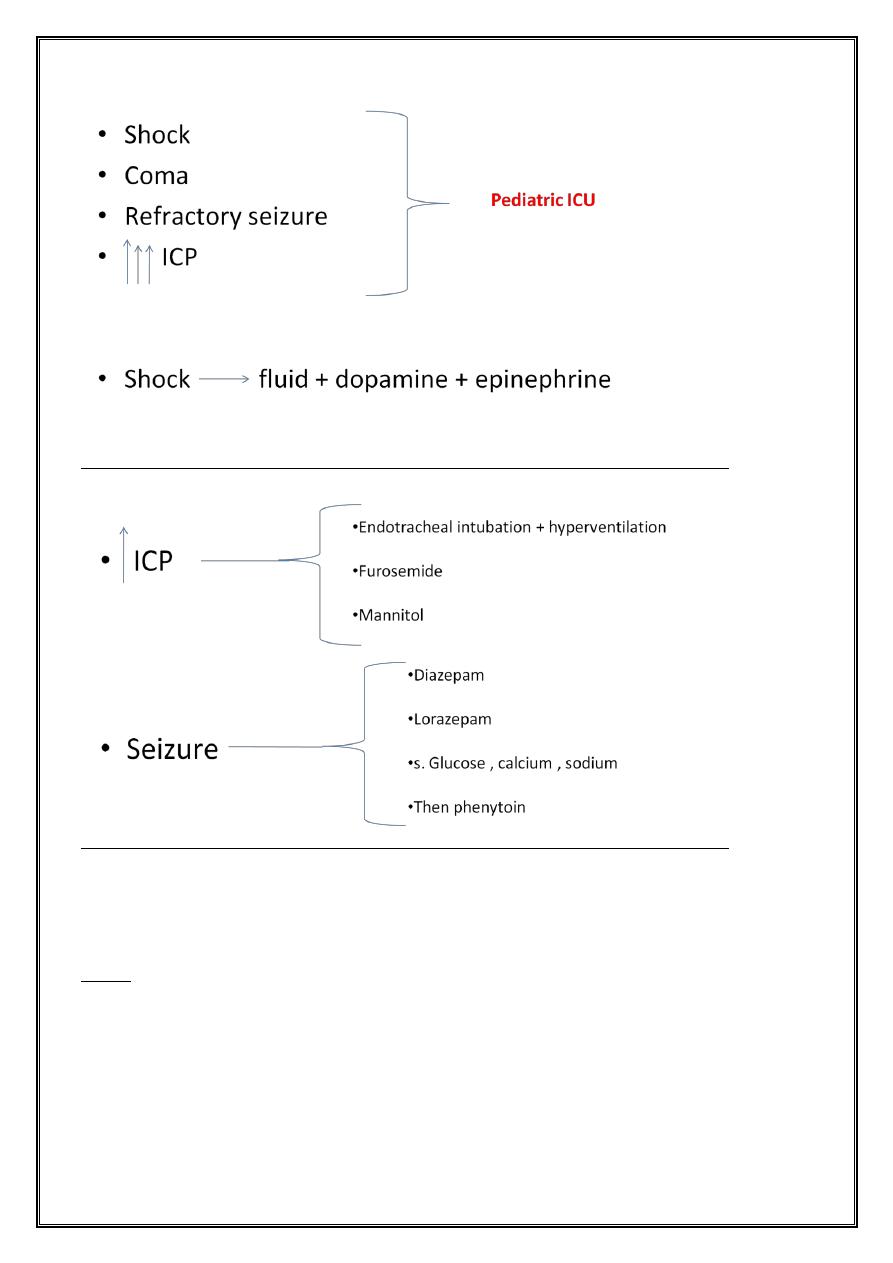
3. Supportive treatment
Dr: Nibal Lec:1
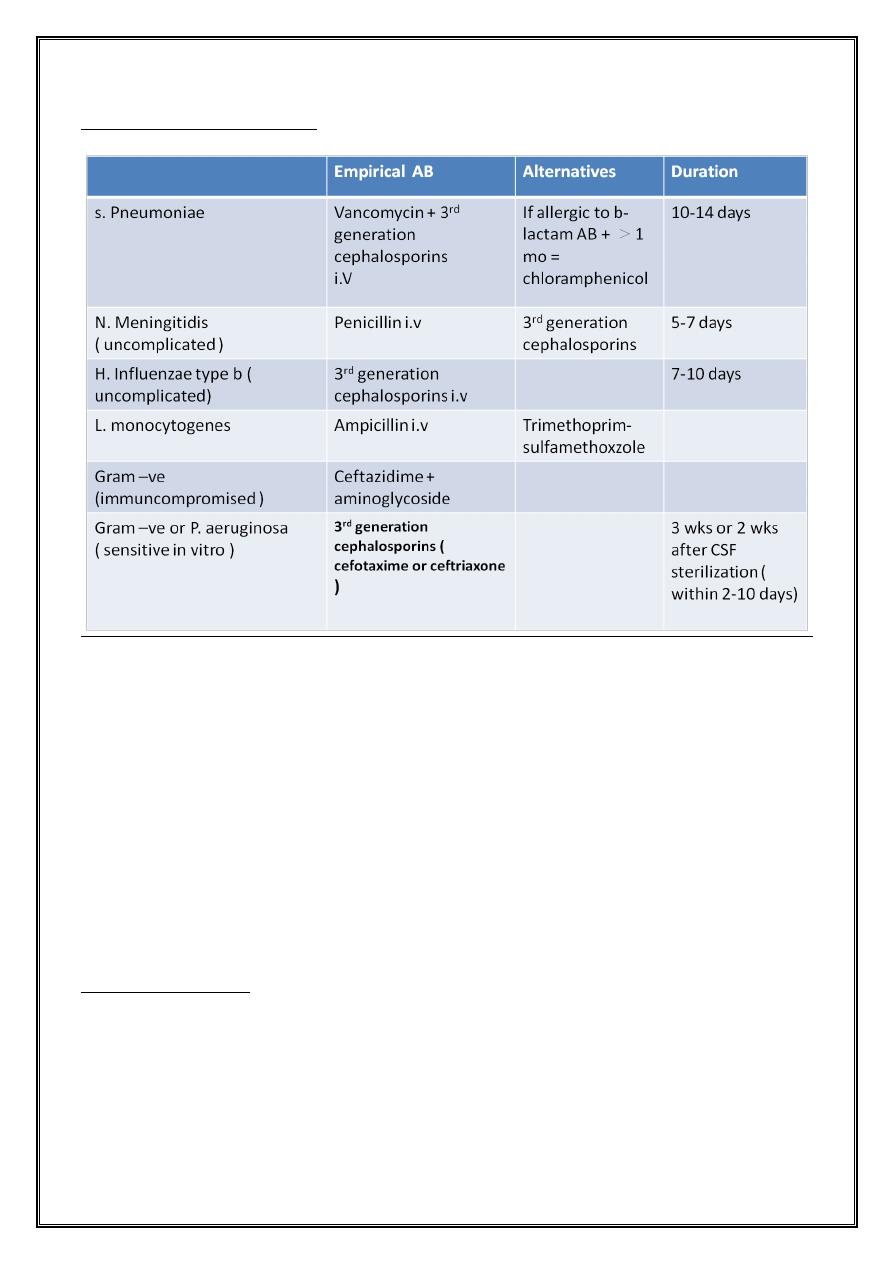
Empirical antibiotic therapy
• 25-50% of S.pneumoniae strains resistant to penicillin
• 25% of S. pneumoniae strains resistant to 3
rd
generation cephalosporins
• If isolates of S.pneumoniae resistant to penicillin or cephalosporins , therapy
should be completed with vancomycin
• If focal signs are present or the child does not respond to treatment , a
parameningeal focus may be present and need CT or MRI scan to be performed
Shall we repeat LP?
• Don’t repeat LP if uncomplicated meningitis due to AB sensitive S.pneumoniae
, N. meningitidis or H. influenzae
• Repeat LP if :
1. Some neonates
Dr: Nibal Lec:1
2. Patients with gram –ve bacillary meningitis
3. Infection by b-lactam resistant S.pneumoniae
Supportive treatment
Monitor patient frequently during 1
st
72 hr
1. Vital signs
2. Neurologic assessment
3. Laboratory studies
• Nothing by mouth
• ICP or SIADH ½ - 2/3 of maintenance
• Then change to maintenance [ 1500-1700 ml/m
2
/24hr ]
Dr: Nibal Lec:1
Complications
Acute
• Seizure s
• ICP
• Cranial nerve palsies
• Cerebral or cerebellar herniation
Dr: Nibal Lec:1
• Thrombosis of dural venous sinuses
• Subdural fluid
• SIADH
• Fever
• Thrombocytosis
• Eosinophilia
• Anemia
• DIC
Long – term sequelae
• Hearing loss
• Mental retardation
• Recurrent seizure
• Delay in acquisition of language
• Visual impairment
• Behavioral problems
Prevention
1. Vaccination
2. Antibiotics
Dr: Nibal Lec:1
Viral meningoencephalitis
Acute inflammatory process involves brain meninges & to variable extent brain tissue
Etiology
• Enterovirus 80% of pathogenes
• Arbovirus [ by tick + mosquitos ]
• HSV-1 severe sporadic
• HSV-2 neonate
• VZV chickenpox
• CMV ICP , congenital infection
• Measles , rubella , mumps
• EBV
Clinical features
• Prodromal non-specific febrile illness
• Progressive CNS deterioration [ disturbed level of consciousness , seizure ,
focal neurologic deficit ]
• Exantheme [measles, rubella, VZV, echo, coxsahievirus ]
DDx
1. Acute bacterial meningitis
2. T.B meningitis
3. Syphilis
4. Lyme disease
Dr: Nibal Lec:1
5. Cat- scratch disease
6. Fungi , rickettsiae , parasite
7. Malignancy , CVD , drugs & toxins
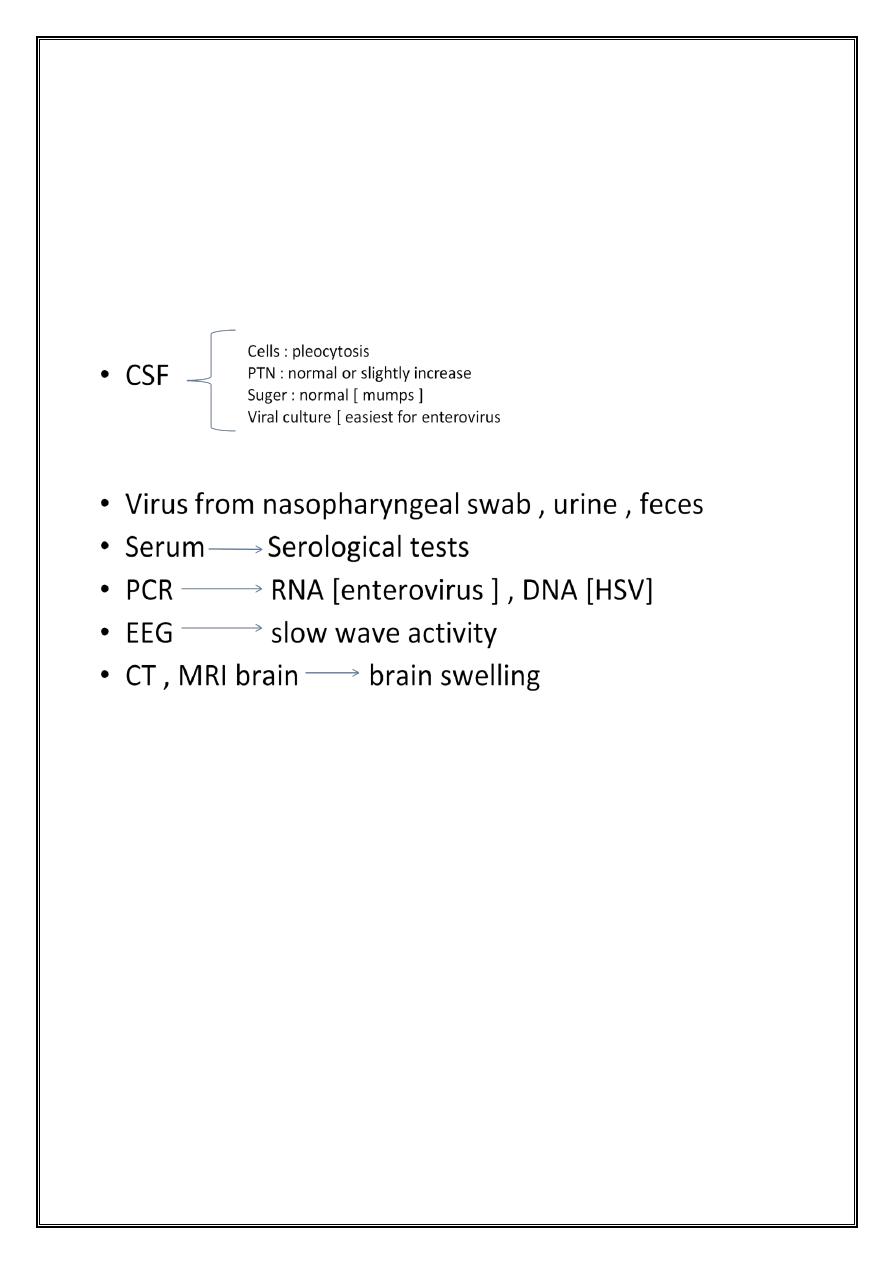
Diagnosis
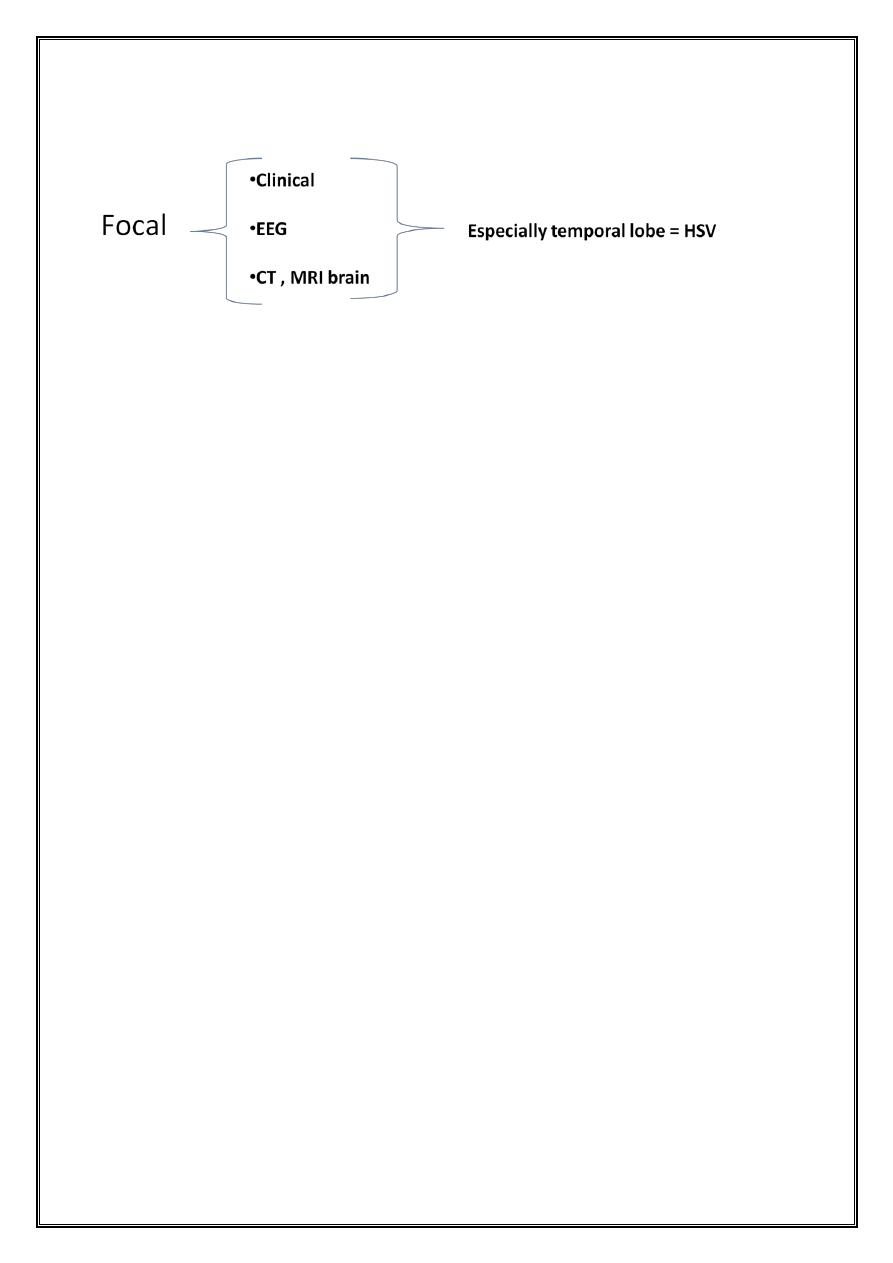
Dr: Nibal Lec:1
Treatment
1. Acyclovir HSV
2. Supportive
• Rest , room light + noise
• Pain non-aspirin containing analgesia
• Fever acetaminophine
• Vomiting codeine , morphine , phenothiazine
• i.v fluid poor oral intake
• Severe hospitalization
1. Rx convulsion
2. Rx cerebral edema
3. Rx aspiration + asphyxia
4. Rx fluid + electrolyte disturbance
5. Rx cardio-respiratory arrest

Dr: Nibal Lec:1
Long term sequelae
1. Motor incooridination
2. Behavioral disturbances
3. Visual disturbance
4. Convulsive disorders
5. Partial or complete hearing loss
