Dr: Muhi Lec :3
Pediatric
BRONCHIAL ASTHMA
IN CHILDREN
Total : 37
Lec : 3
Dr: Muhi Lec :3
Dr: Muhi Lec :3
BRONCHIAL ASTHMA IN CHILDREN
Prof.Dr. Muhi K. Aljanabi
MRCPCH; DCH; FICMS
Consultant Pediatric Pulmonologist
OBJECTIVES
1. Understand the natural history of asthma during childhood.
2. Be familiar with the key features of history and examination that support a diagnosis of
asthma.
3. Be familiar with the other common clinical conditions that can mimic asthma
(gastroesophageal reflux, cystic fibrosis, viral induced wheezing, bronchiolitis, croup).
4. Be able to manage an acute exacerbation of asthma.
5. Know the details of the drugs used to treat acute and chronic asthma and understand their
mechanism of action.
6. Know the guidelines for the management of asthma.
7. Be able to advise parents about how to care for a child with asthma.
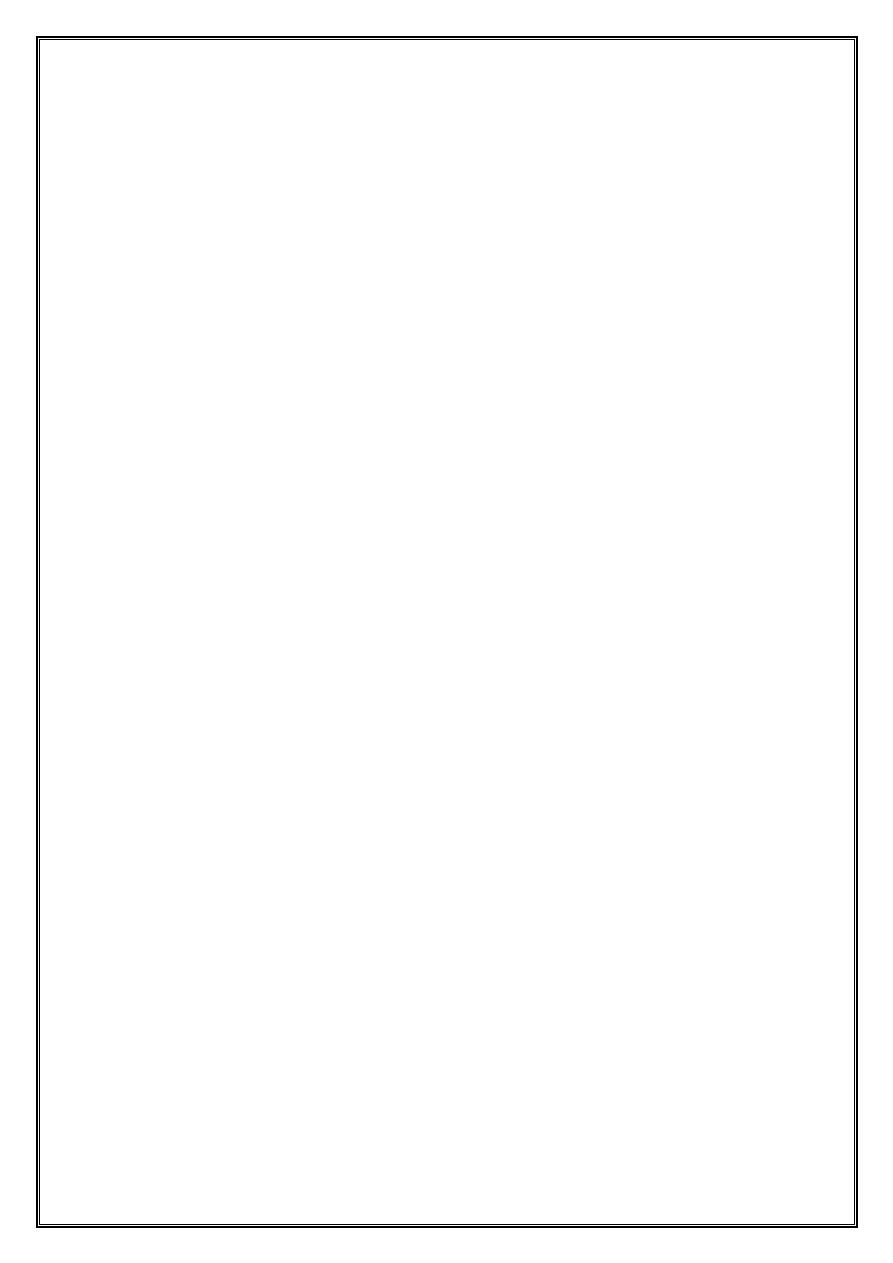
DEFINITION
Asthma is a chronic inflammatory condition of the lung airways resulting in episodic
airflow obstruction.
This chronic inflammation heightens the “twitchiness” of the airways—airways
hyperresponsiveness (AHR)—to provocative exposures.
ETIOLOGY
1- Genetics:
More than 22 loci on 15 autosomal chromosomes have been linked to asthma.
2- Environment :
Common respiratory viruses.
Indoor and home allergen exposures in sensitized individuals
Environmental tobacco smoke and air pollutants (ozone, sulfur dioxide)
Cold dry air and strong odors
Dr: Muhi Lec :3
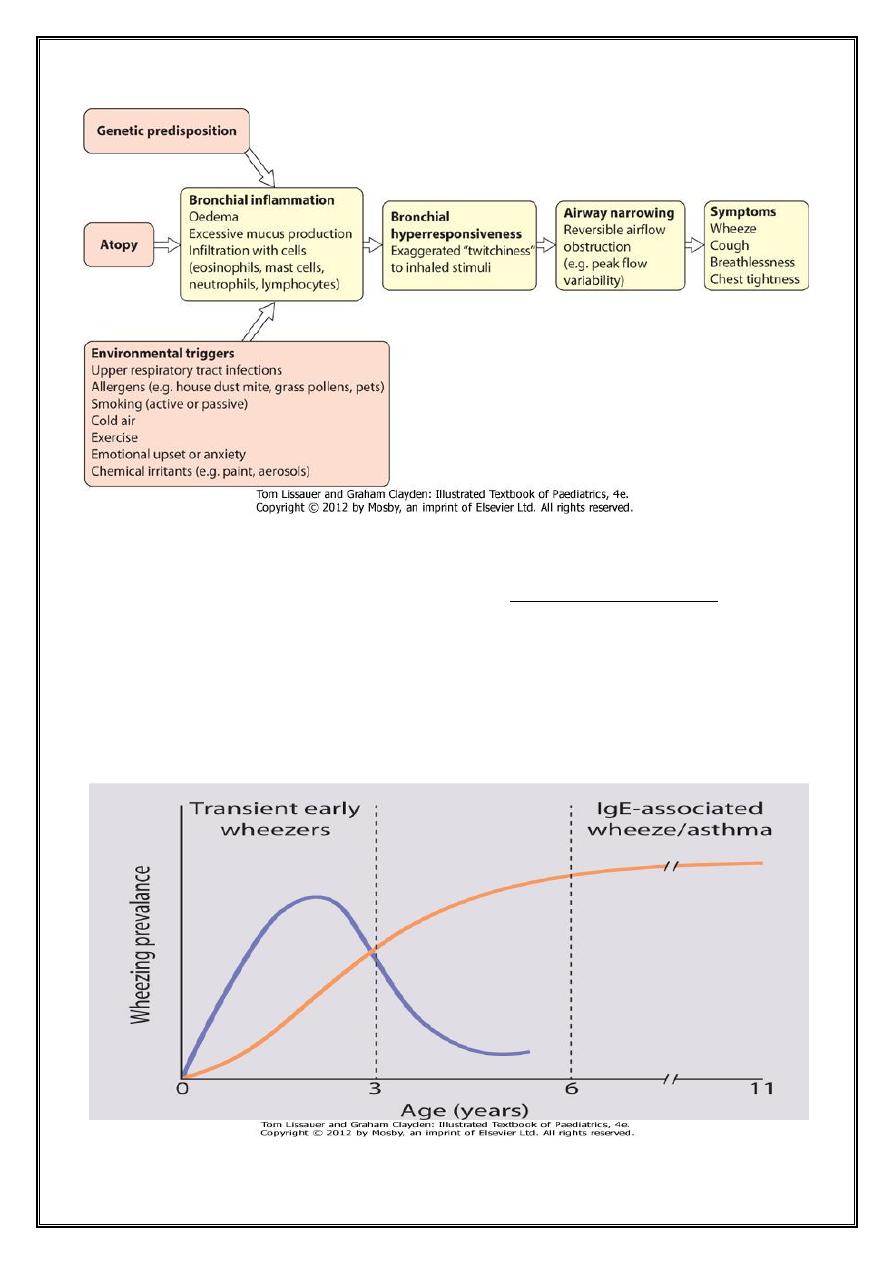
EPIDEMIOLOGY
Worldwide, childhood asthma appears to be increasing in prevalence, despite
considerable improvements in management.
In 56 countries found a wide range in asthma prevalence, from 1.6 to 36.8%.
Approximately 80% of all asthmatics report disease onset prior to 6 yr of age.
Only a minority will go on to have persistent asthma in later childhood.
Dr: Muhi Lec :3
CLINICAL MANIFESTATIONS
Intermittent dry coughing and/or expiratory wheezing are the most common
chronic symptoms of asthma.
shortness of breath
worse at night
Daytime symptoms, often linked with physical activities
RISK FACTORS
history of other allergic conditions (allergic rhinitis, allergic conjunctivitis,
atopic dermatitis, food allergies)
Parental asthma, and/or symptoms apart from colds, supports the diagnosis of
asthma.
LABORATORY FINDINGS
Lung function tests can help to confirm the diagnosis of asthma and determine
disease severity.
Chest radiographs in children with asthma often appear to be normal,
hyperinflation (flattening of the diaphragms) and peribronchial thickening.
Asthma masqueraders (aspiration pneumonitis, bronchiolitis obliterans)
Asthma exacerbations (atelectasis, pneumomediastinum, pneumothorax). CT
scans may be needed.
Other tests, such as allergy testing to assess sensitization to inhalant allergens,
help with the management and prognosis of asthma.
88% of asthmatic children had inhalant allergen sensitization by allergy prick
skin testing.
TREATMENT
Principles of Asthma Pharmacotherapy:
Treat all “persistent” asthma with anti-inflammatory controller medication
Daily controller therapy is not recommended for mild intermittent asthma.
Dr: Muhi Lec :3
The “three strikes” rule
Day time asthma symptoms at least 3 times per wk,
Awakens at night at least 3 times per mo,
Experiences asthma exacerbations that requires short courses of
systemic corticosteroids at least 3 times a yr.
Then that patient should receive daily controller therapy
(ICS) therapy is recommended as preferred therapy for all levels of asthma
severity except for the mild intermittent category.
Leukotriene pathway modifiers or sustained-release theophylline (only for
patients >5 yr of age) are alternatives for mild persistent asthmatics.
Combination of a low-to-medium dose ICS with a long-acting β-agonist or a
leukotriene modifier or theophylline is a mainstay therapy for moderate
persistent asthma in older children.
For infants and young children, medium-dose ICS alone it is considered a
preferred treatment for moderate persistent asthma.
Severe persistent asthmatics should receive high-dose ICS, a long-acting
bronchodilator, and routine oral corticosteroids if needed.
SABAs are the recommended quick-reliever medications for symptoms and
exercise pretreatment for all asthma severity levels
INHALED CORTICOSTEROIDS
Daily ICS therapy as the treatment of choice for all patients with persistent
asthma.
ICS reduce asthma symptoms, improve lung function, reduce “rescue”
medication use and, most important, reduce urgent care visits,
hospitalizations, and prednisone use for asthma exacerbations by about 50%
Dr: Muhi Lec :3
LONG-ACTING INHALED β-AGONIST
Although LABAs (salmeterol, formoterol) are considered to be daily
controller medications, not intended for use as “rescue” medication for acute
asthma symptoms or exacerbations,
nor as monotherapy for persistent asthma.
LEUKOTRIENE-MODIFYING AGENTS
leukotriene receptor antagonists (LTRA)
Montelukast > 1 yr.
Zafirlukast > 5 yr
Decrease need for rescue β-agonist use
NONSTEROIDAL ANTI-INFLAMMATORY AGENTS
Cromolyn and nedocromil are non-corticosteroid anti-inflammatory agents
that can inhibit allergen-induced asthmatic responses and reduce exercise-
induced bronchospasm.
THEOPHYLLINE
Although it is considered an alternative monotherapy controller agent for
older children and adults with mild persistent asthma,
It is no longer considered a first-line agent for small children in whom there
is significant variability in the absorption and metabolism of different
theophylline preparations, necessitating frequent dose monitoring (blood
levels) and adjustments.
SHORT-ACTING INHALED β-AGONISTS
SABAs (albuterol, levalbuterol, terbutaline, pirbuterol) are the first drugs of
choice for acute asthma symptoms (“rescue” medication) and for preventing
exercise-induced bronchospasm.
Dr: Muhi Lec :3
ANTICHOLINERGIC AGENTS
ipratropium bromide are much less potent than the β-agonists.
Inhaled ipratropium is primarily used in the treatment of acute severe
asthma.
When used in combination with albuterol, ipratropium can improve lung
function and reduce the rate of hospitalization in children who present to the
emergency department with acute asthma.
Home Management of Asthma Exacerbations
Immediate treatment with “rescue” SABA
Short course of oral corticosteroid therapy
Injectable forms of epinephrine
Portable oxygen at home.
Call for emergency support services.
ED Management of Asthma
Oxygen
Inhaled β-agonist
Systemic corticosteroids
Inhaled ipratropium
Intramuscular injection of epinephrine or other β-agonist
Close monitoring of clinical status, hydration, and oxygenation
Intubation and mechanical ventilation
Dr: Muhi Lec :3
PROGNOSIS
Recurrent coughing and wheezing occurs in 35% of pre–school-age children.
⅓ continue to have persistent asthma into later childhood.
⅔ improve on their own through the preteen years.
That entire wheeze is not asthma
&
Asthma does not always wheeze
