Urinary Tract InfectionsUTI
Dr. Mohammed Hannon Al Sodani C.A.B.M., F.I.C.M.S.For 5th year students 2014-2015
College of Medicine , University of Baghdad
March,9th,2015
UTI definition
-Multiplication of organisms in the urinary tract.
It is usually associated with the presence of neutrophils
and > 100 000 organisms/ml in a midstream sample of urine
The most common bacterial infection in medical practice Incidence 50 000 / million persons / year
In women > men - relatively short urethra
- absence of bactericidal prostatic secretions.
- sexual intercourse ( minor urethral trauma )
- Uncommon in males , except in first year of life & over 60.
- Common source of life-threatening G - ve septicemia -
UTI Etiology and pathogenesis
When the UT is anatomically and physiologically normal with intact local and systemic defense mechanisms , bacteria are confined to the lower end of the urethra.
local and systemic defence mechanisms
Neutrophil & Complement
Urine osmolality and pH > 800 mOsm/kg and low or high pH
reduce bacterial survival.
Commensal organisms – ( lactobacilli, bacteroides)
Urine flow and normal micturition wash out bacteria..
Uroepithelium - IgA production
- Tamm-Horsfall proteins (in the mucus ) covering
uroepithelium, have antibacterial properties.
UTI Etiology and pathogenesis
UTI is most often due to bacteria from the patient's own bowel flora (Transfer to UT: - Ascending transurethral route (most often- Bloodstream & Lymphatics
- Direct extension (e.g. vesicocolic fistula)
Organisms causing UTI
Organism Approximate frequency (%)E. coli and other 'coliforms‘’ from GIT 75 %
Proteus mirabilis 12%
Pseudomonous
Klebsiella aerogenes *
Enterococcus faecalis *
Staphylococcus 10%
†
UTI Risk Factors
- Incomplete bladder emptying;-
- Bladder outflow obstruction, e.g BPH
- Neurological problems (e.g. multiple sclerosis, diab.neuropathy) - Gynaecological abnormalities(e.g. uterine prolapse)
- Vesico-ureteric reflux
- Foreign bodies - Urethral catheter
- Ureteric stent
- Cystoscopy
- Loss of host defenses
- Atrophic urethritis & vaginitis in post-menopausal women
- Diabetes Mellitus
- Others PKD , Renal stones
UTI The Spectrum Of Presentations
- Asymptomatic bacteriuria- Acute urethritis and cystitis
- Acute pyelonephritis
- Acute prostatitis
- Septicemia (usually Gram-negative bacteria
Acute urethritis and cystitis Lower UT
Clinical Presentation- Frequency Abrupt onset ,Dysuria Scalding pain, Suprapubic pain during and after voiding ,Urgency intense desire to pass more urine after micturition – cloudy urine an unpleasant odour . Haematuria microscopic or visibl.
Systemic symptoms are usually slight or absent.
However infection can spread up ( acute pyelonephritis in 30 % ) -Minimal or no symptoms :-
Atypical symptoms ;- abdominal pain, backache ,fever or hematuria,
in the absence of frequency or dysuria
The DDX
urethritis due to STD, notably chlamydia , Reiter’s syndrome.
urethral syndrome , post-menopausal atrophic vaginitis.
Acute pyelonephritis
- Triad of - loin pain, fever with tenderness over kidneys.
- Pathology –etiology ;-- Pelvis; Inflamed, parenchy. small abscesses , PMN infiltration .
- Route ;- Ascending form lower UT (almost always)
- Bacteremia (rarely)- renal / perinephric abscesses
- Staphylococci mostly
- Pre existing renal damage by cyst or stone or scar.
- Medulla> cortex – low O2 tension, high osmolality, high H+
&ammonia , impaired WBC function
- - Rarely,, CT scaning can show wedge-shaped areas of inflammation in the renal cortex and hence damage to renal function.,( rare with antibiotics, with normal urinary tracts)
Acute pyelonephritis
Clinical features;-- Acute loin(s) pain , radiated to IF or SPA /tender lumbar region
( - 30% with cystitis (frequency …..
- Systemic symptoms are usually present ;- Fever, rigor, vomiting
&hypotension.
Rarely, complicated by papillary necrosis;- Fragments of renal papillary tissue are passed per urethra . +/_ ureteric obstruction acute renal failure.
Predisposing factors include DM
Chronic urinary obstruction,
Analgesic nephropathy and
Sickle-cell disease..
Acute pyelonephritis
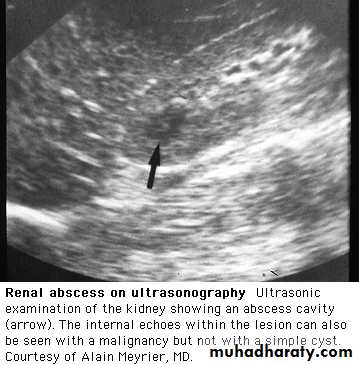
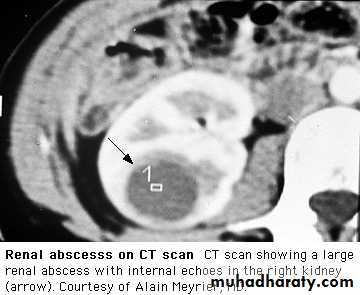
Perinephric abscess marked pain and tenderness and bulging of the loin , extremely ill, with fever, leucocytosis and positive blood cultures. Urinary symptoms are absent, and urine contains neither pus cells nor organisms.
Emphysematous pyelonephritis;- A necrotizing form of pyelonephritis with gas formation, is occasionally seen in diabetics
Xanthogranulomatous pyelonephritis
is a chronic infection that resemble a tumour. It is usually associated with obstruction, is characterised by accumulation of foamy macrophages and generally requires nephrectomy...
The D.DX of pyelonephritis includes;-
acute appendicitis, diverticulitis, cholecystitis and
Salpingitis ,ruptured ovarian cyst ectopic pregnancy
UTI Diagnosis
- Definitive diagnosis ( clinical features with findings in the urine)G U E:- Macro. Turbid with debris, filaments , bad smell
Micro Pus cells +/- RBC, Bacteria Gram + ve or - ve
Urine C/S Culture of MSU/ suprapubic aspiration
is necessary, in patients with:-- recurrent infection or after failure of initial treatment, pregnancy, or serious infection ( Diabetics, immunocompromised , Indwelling catheter & elderly)
while in healthy woman with a single lower UTI non complicated infection, urine culture prior to treatment is not mandatory
Full blood count RFT FBG Blood culture.
Gram stain of urine shows numerous Gram-negative rods.E.coli grew from this urine specimen
UTI Investigation
KUB Radio oapquestone , emphesemaRenal ultrasound or CT To identify obstruction, cysts, calculi perinephric collection.
-Infants, children, men after single UTI, Women who have
(1) acute pyelonephritis;
(2) recurrent UTI after antibiotic treatment;
(3) UTI or asymptomatic bacteriuria in pregnancy
IVU :- particularly to image the collecting system after voiding
Micturating cysto-urethrogram (MCU) or radioisotope study to identify and assess severity of vesico-ureteric reflux or impaired bladder emptying Selected infants and children; Cystoscopy;-
Patients with haematuria or a suspected bladder lesion.
UTI Treatment
Antibiotics are recommended in all cases of proven UTI
-Trt to be started while awaiting the result of C/S.
- Trt for 3 days is the norm. for lower UTI
- Trimethoprim (200 mg 12 hrly) is DOC for initial Trt.
Other effective ABC :-
- Nitrofurantoin, 50mg 6 hourly .
- Quinolone (ciprofloxacin / norfloxacin, levofloxacin)
- cefalexin. - Co-amoxiclav or amoxicillin
- Penicillins and cephalosporins are safe to use in pregnancy
but not trimethoprim, sulphonamides, quinolones &tetracyclines
-Trt is modified after C/S , &or the clinical response
- Adequate fluid intake, 2 L /day during trt & for few wk.
- Symptomatic - Urinary alkalinizing (potassium citrate )
- Analgesia & antipyretics
.
Acute pyelonephritis
Management
- Adequate fluid intake, oral / intravenous.
- Antibiotics are continued for 7-14 days.
Severe cases require I.V ABC , with a cephalosporin, quinolone or gentamicin), later switching to an oral agent.
In less severe cases, oral ABC can be used throughout.
Penicillins and cephalosporins are safe in pregnancy; other antibiotics should usually be avoided.
Urine should be cultured during and after treatment.
If obstruction is present, drainage by a percutaneous nephrostomy should be considered
.
Bacterial prostatitis
- Common in middle & young age males- > 90 % of febrile UTI have asymptomatic prostatitis
(high PSA & increased prostate volume )
- Acute - UTI symptoms plus fever, rigor, constitutional symptoms
- perianal & low back pain,
- Rectal ex. - ?? sepsis
- tenderness, hot, swollen prostate
- pus in expressed prostatic secretion.
-GUE, C/S as in UTI
-Treatment ;- 4-6 weeks - trimethoprim or ciprofloxacin
- Chronic - Relapsing UTI, perianal & low back pan,
- no fever or constitutional symptoms
- PR non remarkable
Recurrent UTI
Relapse :- Recurrence of bacteriuria with the same organism within 7 days of completion of antibacterial treatment
-Implies failure to eradicate infection,
- Usually in conditions such as stones, scarred kidneys, PKD
Reinfection;-
- When bacteriuria is absent after treatment for at least 14 days,
- Followed by recurrence of infection with the same or different organisms.
- the result of reinvasion with new organisms.
PERSISTENT OR RECURRENT UTI
Prophylactic measures to be adopted by with recurrent urinary infectionsFluid intake of at least 2 L/day
Regular complete emptying of bladder
If vesico-ureteric reflux is present, practice double micturition (empty the bladder then attempt micturition 10-15 minutes later
Good personal hygiene
Emptying of the bladder before / after sexual intercourse
Cranberry juice may be effective
Drug
UTI3days
women 7days
A.Pyelonephritis
7-14 days
B.prostatitis
• 4-6weeks
Prophyl-actic
Trimethoprim200 mg daily
200 mg daily
200 mg 12 hr
100 mg night
Nitrofurantoin
50 mg 6 hr
50 mg 6-hr
50-100 mg
night
Co-amoxiclav
250/125 mg 8hourly
250/125 mg 8hourly
250/125 mg night
Ciprofloxacin
100 mg 12 hr
250-500 mg 12hr 100 mg 12hr IV
250mg /12hr
Norfloxacin
400 mg 12 hr
400 mg 12 hourly
400 mg / 12 hr
Cefuroxime
250 mg/ 12 hr 750mg 6-8hrly IVCefalexin
500mg 12 hr500mg 12 hr
250mg night
Gentamicin
3-5mg/kg IV daily
UTI in the presence of an indwelling catheter
After urinary catheterization > few days colonization of the bladder by a urinary pathogen, an increases the risk of Gram-ve bacteraemia fivefold .,.Infection by Candida is a frequent in DMTreatment
is usually avoided in asymptomatic patients. ABC indicated only if - symptoms or evidence of infection, - immunocompromised pt
- removal or replacement of the catheter.
- in candiduria urinary alkalinazation and in severe infections intra vesical amphotericin
Prevention
- Catheters should not be used unnecessarily
- Sterile insertion, to be removed as soon as it is not required
- Closed drainage systems .
.
Asymptomatic bacteriuria
This is defined as > 100 000/ml organisms in the urine of apparently healthy asymptomatic patients.
1% < 1yr, 1% of schoolgirls,
0.03% of schoolboys & men,
3% of non-pregnant and 5% of pregnant
30% --- symptomatic infection within 1year.
- In general, treatment is not indicated only In :-
Infants
Pregnant women
Abnormal urinary tract. n.
Bacteriuria in pregnancy
.- Urine C/S is a must in pregnancy
- 2- 6% asymptomatic bacteriuria. With Risk of severe symptomatic pyelonephritis & premature labour.
-previous renal dis., - pre-eclamptic toxaemia, anaemia of pregnancy & small or premature babies.
Must always be treated and eradicated.
Reinfection may require prophylactic therapy.
Amoxicillin and ampicillin, Nitrofurantoin &
Cephalosporins may be safely be used in pregnancy
WHILE
Tetracycline, trimethoprim, sulphonamides and 4-quinolones must be avoided in pregnancy
.
Urethral Syndrome
- Abacteriuric frequency or dysuria Usually female,
- Symptoms of urethritis and cystitis
- No bacteria are cultured from the urine. 'sterile pyuria',
Causes include:-
- postcoital bladder trauma,
- post menopausal atrophic vaginitis or urethritis in the elderly,
- interstitial cystitis
- infection with organisms not cultured by ordinary methods
(e.g. Chlamydia, certain anaerobes ,TB),
- intermittent or very low-count bacteriuria,-
- Incomplete trt by ABC. – Malignancy- Stones- Vasculitis
reaction to toilet preparations or disinfectants
Antibiotics are not indicated
.
Tuberculosis of the urinary tract
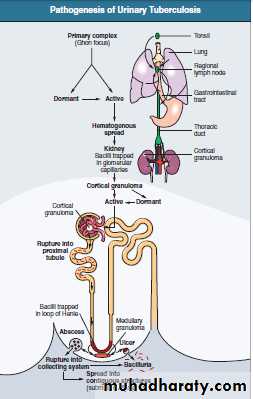
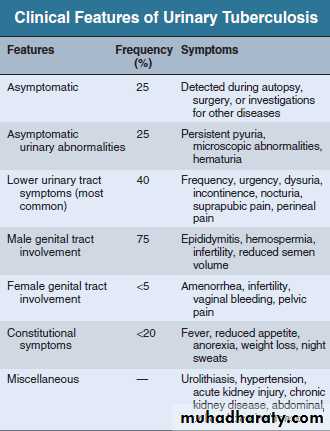
Pathology Cortical lesions from haematogenous spread in the primary phase. – Either heals (most ) or persists - spreads to the papillae, cavitating lesions ,discharge of mycobacteria into the urine, Infection of the ureters and bladder, ( ureteral stricture , a contracted bladder)Rarely, cold abscesses may form in the loin.
- In males the disease may present with testicular or epididymal discomfort and thickening.
A high index of suspicion age 20 and 40 years male to female ratio of 2:1..
High risk ;-
close contact with sputum smear–positive pts,
social deprivation, neglect,
Immunosuppression, HIV infection or (AIDS), DM CRF
Transplanted kidneys may also transmit TB to the recipients
TB ofthe urinary tract
Tuberculosis of the urinary tract
Diagnosis ;- Constant awareness, ??? sterile pyuria. -- Active infection -
AFB culture of mycobacteria from early-morning urine samples
- CBP , RFT , FBG
Excretion urography may show;-
- Cavitating lesions in the renal papillary areas, commonly with calcification.
- Evidence of ureteral obstruction with hydronephrosis.
- may be normal in diffuse interstitial renal TB
Tuberculosis of the urinary tract
- Renal biopsy.Some patients present with small unobstructed kidneys, when the diagnosis is easy to miss.
- Renal ultrasonography or excretion urography
should be carried out 2-3 months after initiation of treatment as ureteric strictures may first develop in the healing phase.
Plain x-raycalcified kidney
Multiple ureteral strictures. Strictures associatedwith dilated ureter, infundibular stenosis and caliectasis
Renal tuberculosisCT scan shows an enlarged leftkidney with multiple cavities present bilaterally (
Contrast-enhanced CT image showing contractedcalcified right kidney and normal opposite side
Renal tuberculosis. A cut section of kidney showingareas of cavitation and caseation necrosis (white chalky material).
Tuberculous granuloma. The granuloma comprisesLanghans giant cells (two large cells in the center), surrounding epithelioidcells, and a rim of lymphocytes
Treatment
usually amenable to medical treatment.Many anti-TB drugs reach kidneys, urinary tract, urine, and cavitary lesions in high concentration, and there are
fewer organisms compared with cavitary lung lesions.
A short-course regimen is recommended.
The treatment is as for pulmonary TB
Daily rifampin (600 mg), isoniazid (300 mg), pyrazinamide (1500mg) in the morning. pyrazinamide is discontinued after 2 months, and isoniazid and rifampin are continued for another 4months.
Treatment
If the patient is very sick with irritative bladder symptoms,streptomycin in daily doses of 1 g may be added during the first 2 months
Longer courses of anti TB treatment 9 months to 2 years are useful in patients
who do not tolerate pyrazinamide,
those responding slowly to a standard regimen,
those with miliary or CNS disease,
and children with multiple-site involvement
Treatment
Surgical treatment. For
ureteral strictures,
- Stents across the narrow segment.
- Reconstructive surgery involves the correction of obstruction to the ureter pyeloplasty,….
- ??? Removal of a unilateral nonfunctioning kidney is controversial.