SURGERY
Anaesthesia
DR. SABAH
AFTER MID
TOTAL LEC:3 LEC: 2
Dr. Sabah
Pre-Operative
testing

Page
2
of 10
Page
3
of 10
Anaesthesia
د
.
صباح نوري السعد
M.B.Ch.B, D.A,
F.I.M.S, C.A.B.A & I.C
P
RE
-
OPERATIVE TESTING
1. Haemoglobin:
History of or anticipated blood loss, major surgery, cardio-respiratory
diseases, routinely for female patient.
2. Blood Urea, Serum Creatinine & Serum Electrolytes:
Hypertension, heart failure, renal failure, major gut or urological surgeries,
diabetic patient, diuretic therapy.
3. Urine Exam: urinary tract infection, diabetes mellitus.
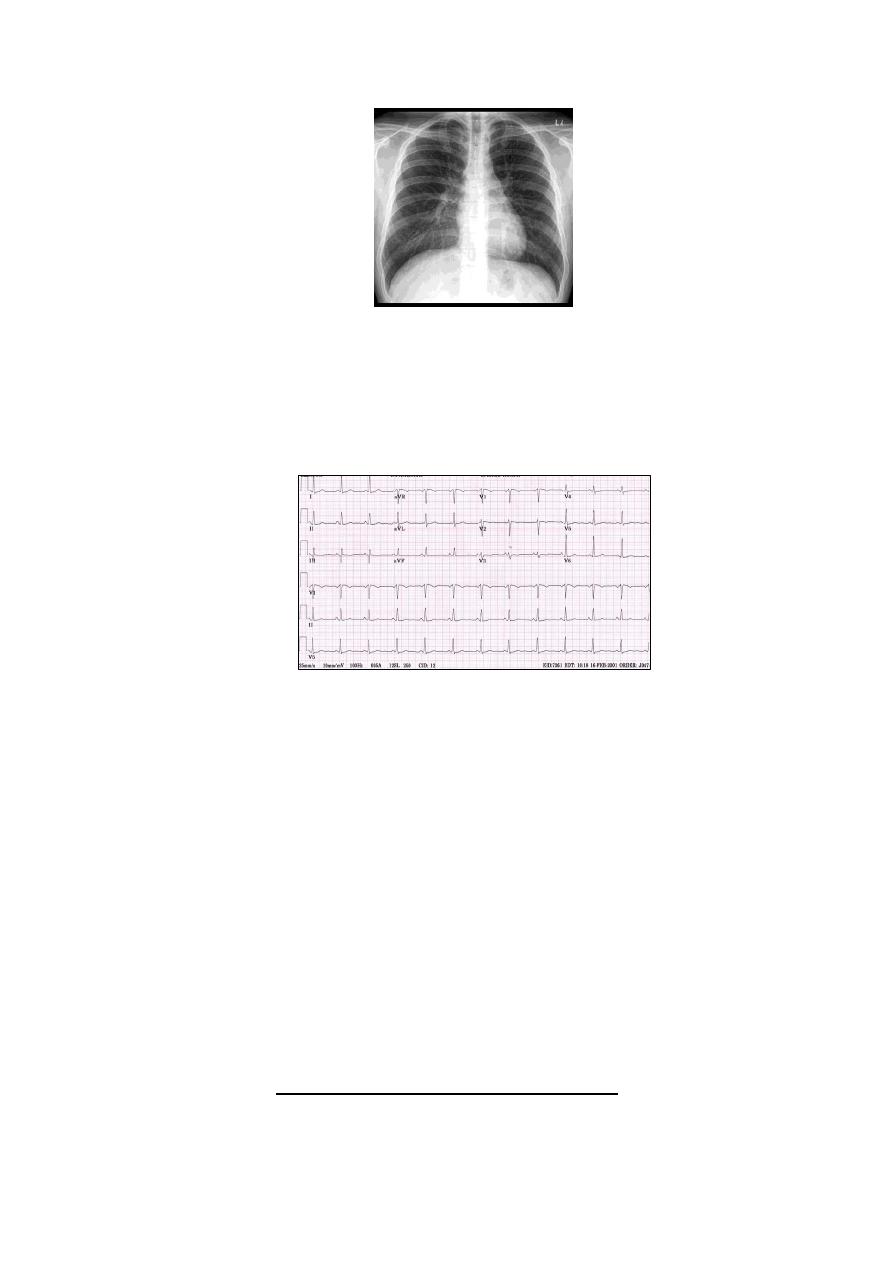
4. Chest X-Ray:
Heart failure, pulmonary disease with localising sign, hypertension, other
cardiac diseases.
Lecture: 2
Page
4
of 10
5. Electrocardiography (ECG):
Arrhythmia, angina pectoris, history of
myocardial infarction,
hypertension, heart failure.
6. Thoracic Inlet X-Ray: Thyroid enlargement.
7. Pulmonary Function Test:
Asthma, chronic obstructive airway disease, thoracic surgeries.
8. Liver Function Test, Albumin, Bilirubin: Liver disease, alcoholics.
9. Coagulation studies:
Liver disease, anticoagulant drugs, plan for spinal or epidural anaesthesia.
10. Echocardiography:
Heart failure, congenital heart diseases, valvular heart diseases.
S
PECIAL
S
ITUATIONS
Page
5
of 10
Day-Case-Surgery:
Patient can be discharged home few hours after operation.
Patient criteria for day-case-surgery:
1. Otherwise completely fit patient, or have minor, well-controlled condition.
2. Has undergone proper pre-operative assessment (regarding history,
physical examination, and testing).
3. Has undergone a proper period of starvation.
4. Has a responsible adult to act as an escort home and for overnight
supervision.
5. The patient must be advised not to drive or operate machinery for 24
hours.
Emergency Surgery:
The patient general medical condition should be ascertained.
In the case of abdominal emergencies or acute haemorrhage, a period of
resuscitation may be required to restore circulating volume and/or
extracellular fluid, because anaesthesia whether general or regional is
hazardous in hypovolemic patient, so it is usual to complete rehydration
and resuscitation before surgery takes place. Requirement for fluid
resuscitation may be easily gauged by the clinical approach:
o
Tachycardia, hypotension, cool peripheries, low urine output → low
circulating volume.
o Breathlessness, raised jugular venous pressure, and basal
crepitation → excessive fluid replacement.
o Clinical judgement can be supported by central venous pressure (CVP)
measurement.
Page
6
of 10
N.B: only in cases of ongoing blood loss (e.g. trauma, rupture ectopic gestation,
leaking aortic aneurysm), speed is important, and resuscitation must proceed at
the same time as surgery and anaesthesia.
Fasting:
For elective surgery: Non Per Os (NPO, nothing by mouth) from midnight
for patient having operation in the morning, while patient having operation
in the afternoon have been thus starved from 7:00 a.m.
For emergency surgery: starvation depends on the urgency of the case.
Premedication:
Premedicants: drugs that are given in the surgical ward mainly to allay
patient fear and anxiety (like benzodiazepines orally or intramuscularly) or
to relief pain like morphine.
Other drugs:
o Antiemetics: metoclpramide, ondansetron
o H
2
-receptor antagonist
o Transdermal glyceryl trinitrate patch
o Steroids
o Atropine
o Heparin
o Antihypertensive, anti-ischemic, anti-epileptics
Page
7
of 10
اخذولكم سنكرز والتوكفون المحاظرة:D
L
OCAL AND
R
EGIONAL
A
NAESTHESIA
Local: normally means the use of a drug to produce anaesthesia by topical,
infiltration or ring block.
Regional: a term reserved to describe major nerve blocks, spinal and epidural
techniques.
Advantages of Loco-Regional anaesthesia versus General anaesthesia:
1. Avoids adverse effects of general anaesthetic agents like, respiratory
depression, cardiovascular depression, nausea and vomiting, and hangover.
2. Avoids potential hazards of unconsciousness: ●loss of airway, ●aspiration
of gastric contents, ●damage to joints, skin, etc through malpositioning.
3. Minimize endocrine stress response to surgery.
4. Decreased post-operative pain.
5. Earlier discharge from hospital.
Disadvantages:
1. Toxicity of local anaesthetics
2. Often difficult techniques: failure, partial success, more discomfort while
performing block, may take longer time to establish anaesthesia.
3. Greater cooperation needed from patient.

Page
8
of 10
4. Sets time limit for surgery.
5. Restricts surgeon flexibility if operation needs to be more extensive.
Topical Anaesthesia
Rapid absorption of local anaesthetic from mucous membrane → rapid rise of
plasma concentration. (e.g. application of local anaesthesia to the mucous
membrane of pharynx, larynx, urethra). Nowadays topical anaesthesia for skin
by EMLA (Eutectic Mixture of Local Anaesthetics).
Infiltration anaesthesia:
Subcutaneous infiltration of local anaesthetic 1cm from the edge of a wound
(elliptical infiltration), or subcutaneous infiltration of an area covering
superficial masses.
Most commonly used local anaesthetic: Lidocaine (xylocaine) 1% or 2%,
1% solution → 1g/100ml or 10mg/ml, which is fair enough for infiltration
Maximum safe dose: 3mg/kg (plain solution)
7mg/kg (with adrenaline)
Page
9
of 10
N.B: Adrenaline added to local anaesthetics to: local vasoconstriction → less
systemic absorption (less toxicity), and more prolonged effect of local
anaesthesia.
But addition of adrenaline is contraindicated in areas supplied by end
arteries: fingers, toes & penile block → irreversible pharmacologic
tourniquet → gangrene.
Other local anaesthetic is Bupivacaine (Marcaine ®) 0.125%, 0.25% and 0.5%,
maximum dose: 2mg/kg (plain solution). Its onset is slower than lidocaine, but
has longer duration.
Ring Block:
Circumferential infiltration of a digit or toe proximal to the wound (without
adrenaline).
خلدون كافي حقن وسج:D
Local Anaesthetic Toxicity:
Causes:
1. Inadvertent intravenous injection of local anaesthetic.
2. Local anaesthetic infiltration with an amount that exceeds maximum safe
dose.
Signs & Symptoms of local anaesthetic toxicity:
1. Central Nervous System
Paraesthesia especially around the mouth.

Page
10
of 10
Anxiety
Tremor
Fitting
Coma
2. Cardiovascular System
Bradycardia
Fall in cardiac contractility → hypotension
Cardiac arrest
Management:
Support for ventilation and circulation with close monitoring.
Diazepam or small dose thiopentone to control fit.
Coma and cardiac arrest → Proper cardiopulmonary resuscitation.
Thank you
Done by :Hussein Sadun Al-Nuaimy
