
1
4th stage
باطنية
Lec-7
د.ظاهر
6/12/2015
Pleural Effusion
Pleural Effusion
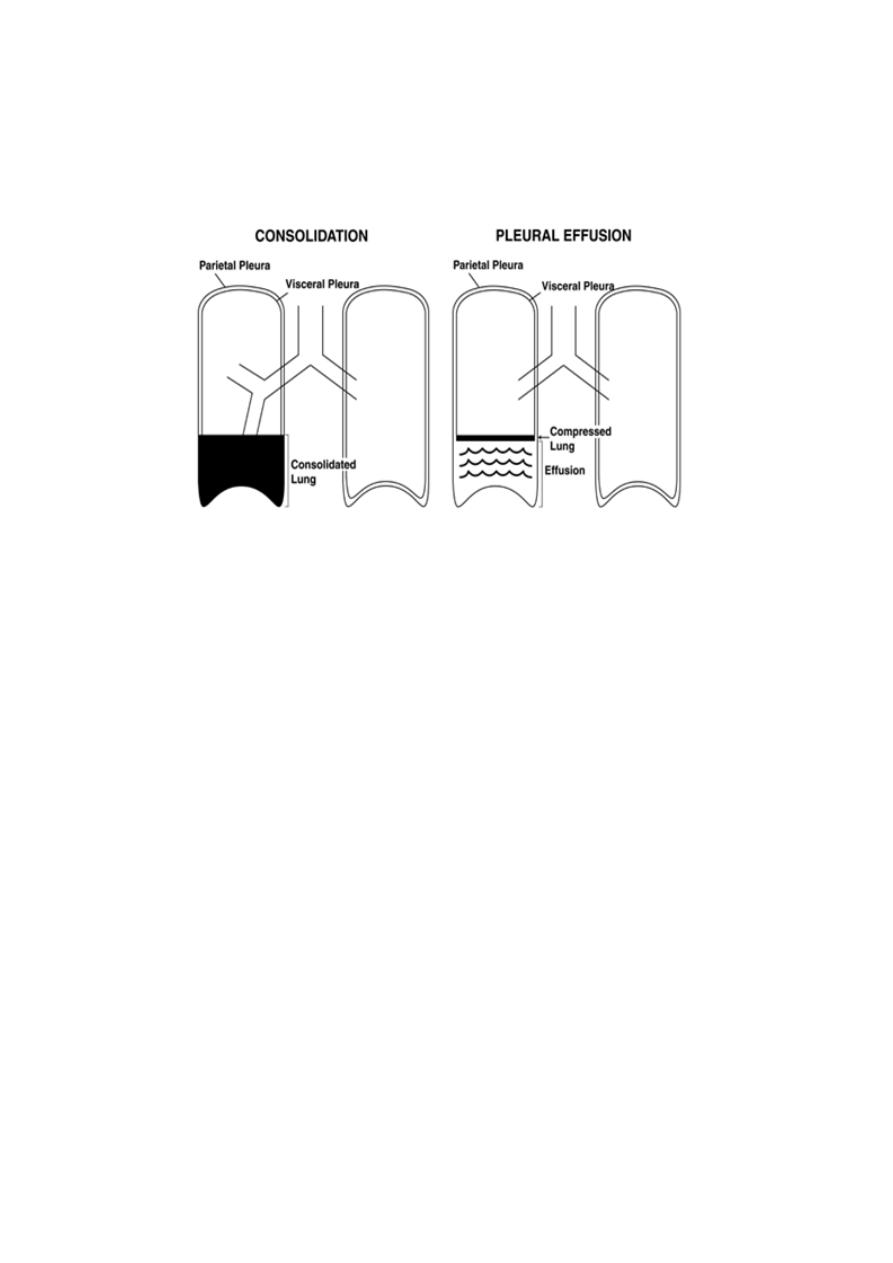
Pleural Cavity and Space
Visceral pleurae envelop all surfaces of the lungs, including the
interlobar fissures.
This lining is absent at the hilus, where pulmonary vessels,
bronchi, and nerves enter the lung tissue.
The mediastinum completely separates the right and left
pleural spaces.
Pleural Effusion
• Accumulation of fluid within the visceral and parietal layers of the
pleura when there is an imbalance between formation and
absorption in various disease states.
• Normal amount 8.4 ml per hemithorax with a WBC count of 1700
per c.mm 75% of which are macrophages and 23% lymphocytes.
• Protein concentration is low about 15% of plasma protein
concentration

2
Pleural Effusion
Exudative Pleural Effusions :
Neoplastic diseases Metastatic disease Mesothelioma •
Infectious diseases
Bacterial infections
Tuberculosis
Fungal infections
Viral infections
Parasitic infections
3
Clinical features
Symptoms and signs of pleurisy often precede the development
of an effusion especially in patients with underlying
pneumonia, pulmonary infarction or connective diseases.
Frequently the onset is insidious.
Breathlessness is the only symptom related to the effusion
depending on the size and the rate of accumulation of the
fluid.
The physical signs
[usually manifest when the pleural effusions exceed 300 mL]
Reduced chest movement on the affected side.
Absence or Decrease tactile vocal fremitus
Absent or Decrease vocal resonance.
Stony dullness on percussion.
Absent or reduced breath sounds.
Large effusion causes displacement of trachea and
mediastinuim to the opposite side.
Pleural Effusion
Clues in the physical Exam. to the common etiologies
A- Distended neck veins, an S3 gallop, or peripheral edema suggests
congestive heart failure.
B- A right ventricular heave or thrombophlebitis and sinus
tachycardia suggests pulmonary embolus.
C- The presence of lymphadenopathy or hepatosplenomegaly may
suggests neoplastic disease.
D-Ascites may suggest a hepatic cause.
E-Signs of consolidation above the level of the fluid in a febrile
patient suggests parapneumonic effusion .
4
Investigations
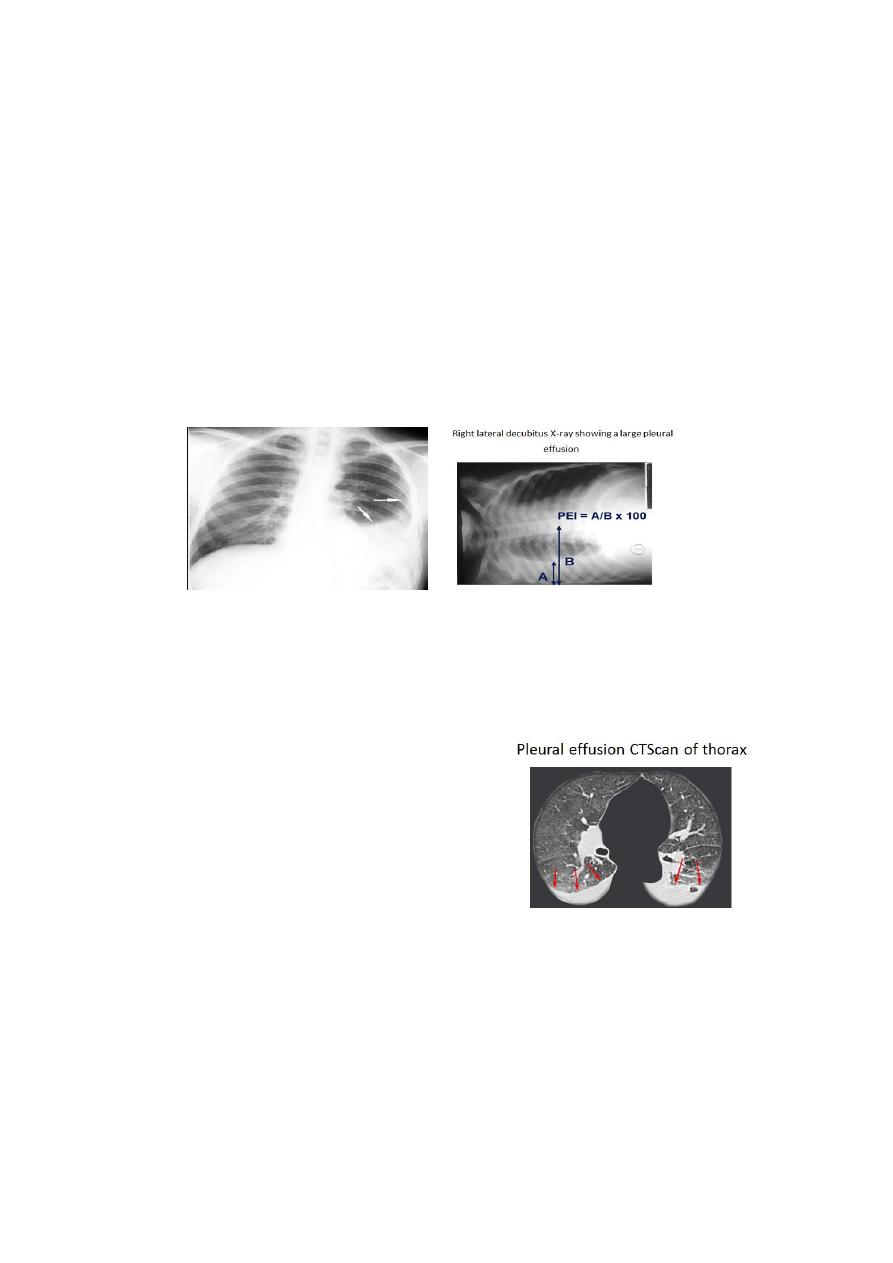
Radiological examination shows dense uniform opacity in
the lower and the lateral parts of the hemi thorax.
Upper margin high in axilla in PA view
*Upper margin high anteriorly and posteriorly in lateral view.
This is just an illusion.
The fluid some times loculated in the interlobular fissure or
below the lower lobe (subpulmonary effusion) simulating
an elevated diaphragm.
Pleural Effusion Role Of Imaging
conventional radiographic methods used are frontal, lateral,
oblique and decubitus radiographs.
Because of gravity, fluid accumulates in subpulmonic
location and then spills over into the costophrenic sulcus
posteriorly, anteriorly, and laterally and then surrounds the
lung forming a cylinder, seen as a meniscoid arc.
5
Amount of fluid – 75 mL-subpulmonic space without spillover,
can obliterate the posterior costophrenic sulcus,
175 mL is necessary to obscure the lateral costophrenic sulcus
on an upright chest radiograph
500 mL will obscure the diaphragmatic contour on an upright
chest radiograph;
1000 ml of effusion reaches the level of the fourth anterior rib,
On decubitus radiographs and CT scans, less than 10 mL, and
possibly as little as 2 mL, can be identified
Pleural Effusion Role Of Imaging
Role of CT scan – Visualization
of underlying lung
parenchymal processes that are
obscured on chest radiographs
by large pleural effusions.
Role of ultrasonography free vs
loculated pleural effusions, and
loculated effusions vs solid
masses.
Thoracentesis of loculated pleural effusions is facilitated by
ultrasound marking or guidance.

6
Role of MRI
Can display pleural effusions, pleural tumors, and chest wall
invasion.
Can characterize the content of pleural effusions.
Can determine the age of the hemorrhage.
Pleural effusion CTScan of thorax
Pleural aspiration and pleural biopsy
1-Pleural fluid aspiration provides the absolute prove for the
presence of pleural effusion, for which 50ml of fluid should be
with-drawn.
Current guidelines recommend the use of a fine bore (21g
green) needle and a 50 ml syringe to gather an adequate
sample.
In cases of pleural effusion of unknown aetiology all aspiration
and biopsy sites should be marked with
Indian ink
, as local
radiotherapy is recommended to prevent tumour invasion of
the chest wall in patients who are subsequently diagnosed with
malignant effusion.
Pleural aspiration Cont..
a- In suspected pulmonary tuberculosis a large volume of fluid
should be aspirated and send for laboratory study.
Pleural fluid usually send for cytological, bacteriological (e.g.
mycobacteriumTB) and biochemical analysis
Pleural fluid aspiration cont..
b- The pleural fluid can be straw-coloured, blood-stained,
purulent or chylous.
c- The most useful indices are protein, lactate dehydrogenase,
Glucose and PH.
The predominate cell type [neutrophils, eosenophils, lymphocyte,
red blood cell].
7
The fluid should also be examined for malignant cells.
Exudative pleural effusion
1-Pleural fluid/ serum protein ratio more than 0.5 . pleural fluid
protein level of >30 g/ l
2- Pleural fluid/ serum LDH ratio more than 0.6 or Pleural fluid
LDH more than two-thirds of the upper limit of normal serum
LDH
3- Pleural fluid glucose is very low(<1.4).
The differential cell count in pleural aspirates
A predominance of polymorphonuclear cells seen in effusion
caused by;
A parapneumonic effusion.
In effusion caused by pulmonary embolus, tuberculosis and
Benign Asbestos Pleural Effusion (BAPE).
The differential cell count in pleural aspirates
An eosinophilic pleural effusion (>10% eosinophils) is of little
use in differentiating aetiology.
It is often associated with air or blood in the pleural space, and
does not exclude malignancy as a possible cause.
A lymphocytic pleural effusion is most often the result of
tuberculosis or malignancy. Up to 10% of tuberculosis effusions
are polymorph predominant.
lymphocyte-rich exudates may also be caused by sarcoidosis,
rheumatoid pleuritis and chylothorax.

8
Specific tests of pleural fluid
Pleural fluid amylase levels are raised (pleural fluid levels
higher than the normal range for serum or pleural-to-serum
ratio >1) in oesophageal rupture, acute pancreatitis and
malignancy (especially adenocarcinoma).
Pleural fluid triglyceride and cholesterol levels should be
measured in cases of suspected chylothorax and
pseudochylothorax.
Adenosine deaminase levels can be helpful in the diagnosis
of tuberculous pleurisy
Transudate pleural effusion
Ultrafiltrates of plasma in the pleura caused by a small, defined
group of etiologies. Pleural fluid protein level is <30 g/l
The following cause transudates ;
◦ Congestive heart failure
◦ Cirrhosis (hepatic hydrothorax)
◦ Atelectasis (which may be due to malignancy or
pulmonary embolism)
◦ Hypoalbuminemia, Nephrotic syndrome, Peritoneal
dialysis, Myxedema and Constrictive pericarditis
The pleural biopsies
Should be taken after the pleural fluid sample is drawn.
Diagnostic yield from pleural biopsy material are greater than
that of pleural effusion examination alone.
The pleural biopsy needle usually inserted in the intercostal
space with the maximum dullness on percussion and at the
maximum radiological opacity.

9
Other investigation
a-Total & differential peripheral blood leucocyte count and ESR.
b-Tuberclin test and sputum for AFB.
c- Biopsy or aspiration of any mass lesion or regional lymph node
enlargement.
d-Bronchoscopy
Management of Pleural effusion
Aspiration should not be performed for bilateral Pleural
effusions in a clinical setting strongly suggestive of a
pleural transudates, unless there are atypical features or
they fail to respond to therapy.
An accurate drug history should be taken during clinical
assessment
Management ..Contin..
1-Pleural Fluid aspiration often necessary especially to relieve
breathlessness.
2-You should not remove more than one (I litre) litre in the first
attempt ,because re-expansion pulmonary oedema may occurs.
3-Chest radiograph should be taken after aspiration to assess the
size of the effusion and to check for secondary pneumothorax.
Management cont…
4-Para-pneumonic effusion requires complete aspiration of the
effusion to avoid the development of Empyema.
5-Tuberculous pleural effusion should be aspirated as much as we
can.
To promote rapid absorption of the effusion prednisolone
20mg/daily by mouth for 4-6 weeks plus the usual course of
anti-tubercolous treatment.

11
6-Malignant pleural effusion should be aspirated completely.
To prevent the re-accumulation the fluid usually aspirated via
chest tube
b-Then the pleural space is obliterated by the injection of
substances which cause sever inflammatory reaction and promote
fibrosis (pleurodesis) e.g. Tetracycline.
