1
DISEASES OF THE SMALL and LARGE INTESTINE

2
\
Ulcerative colitis: Active proctitis
• Most patients with ulcerative proctitis respond to a 1 g
mesalazine suppository but some will additionally require oral 5-
aminosalicylate (5-ASA) therapy.
• Topical corticosteroids are less effective and are reserved for
patients who are intolerant of topical mesalazine.
• Patients with resistant disease may require treatment with
systemic corticosteroids and immunosuppressants.
Active left-sided or extensive ulcerative colitis
• In mild to moderately active cases, the combination of a oral and
a topical 5-ASA preparation.
• The topical preparation is typically withdrawn after 1 month. The
oral 5-ASA is continued long-term to prevent relapse.
• In patients who do not respond to this approach within 2–4
weeks, oral prednisolone (40 mg daily, tapered by 5 mg/week
over an 8-week total course) is indicated. Corticosteroids should
never be used for maintenance therapy. At the first signs of
corticosteroid resistance or in patients who require high
corticosteroid doses to maintain control, immunosuppressive
therapy with a thiopurine should be introduced.

3
Severe ulcerative colitis
• Patients who fail to respond to maximal oral therapy and
those who present with acute severe colitis are best
managed in hospital and should be monitored jointly by a
physician and surgeon:
• clinically: for the presence of abdominal pain,temperature,
pulse rate, stool blood and frequency.
• by laboratory testing: haemoglobin, white cell count,
albumin, electrolytes, ESR and CRP
• radiologically: for colonic dilatation on plain abdominal X-
rays.
Medical management of fulminant ulcerative colitis:
1. Admit to hospital for intensive therapy and monitoring
2. Intravenous fluids and correction of electrolyte imbalance
3. Transfusion if haemoglobin < 100 g/L (< 10 g/dL)
4. IV methylprednisolone (60 mg daily) or hydrocortisone (400 mg
daily)
5. Antibiotics until enteric infection excluded
6. Nutritional support
7. Subcutaneous low-molecular-weight heparin for prophylaxis of
venous thromboembolism
8. Avoidance of opiates and anti diarrhoeal agents
9. Consider infliximab (5 mg/kg) or ciclosporin (2 mg/kg) in stable
patients not responding to 3–5 days of corticosteroids
10. Patients who develop colonic dilatation (> 6 cm), those whose clinical and
laboratory measurements deteriorate and those who do not respond after 7–
10 days’ maximal medical treatment usually require urgent colectomy.

4
Maintenance of remission
• Life-long maintenance therapy is recommended for all patients
with left-sided or extensive disease but is not necessary in those
with proctitis.
• Once-daily oral 5-aminosalicylates are the preferred first-line
agents. Sulfasalazine can be considered in patients with
coexistent arthropathy.
• Patients who frequently relapse despite aminosalicylate drugs
should be treated with thiopurines.
Crohn’s disease
• Crohn’s disease is a progressive condition which may result in
stricture or fistula formation if suboptimally treated.
• It is therefore important to agree long-term treatment goals with
the patient; these are to induce remission and then maintain
corticosteroid-free remission with a normal quality of life.

5
Crohn's disease : Induction of remission
• Corticosteroids remain the mainstay of treatment for
active Crohn’s disease.
• The drug of first choice in patents with ileal disease is
budesonide, since it undergoes 90% first-pass metabolism
in the liver and has very little systemic toxicity. If there is
no response to budesonide within 2 weeks, the patient
should be switched to prednisolone , which has greater
potency.
• As an alternative to corticosteroid therapy, enteral
nutrition with either an elemental (constituent amino
acids) or polymeric (liquid protein) diet may induce
remission.
• Some patients with severe colonic disease require
admission to hospital for intravenous corticosteroids. In
severe ileal or panenteric disease, induction therapy with
an anti-TNF agent is appropriate, provided that acute
perforating complications, such as abscess, have not
occurred.
• Randomised trials have demonstrated that combination
therapy with an anti-TNF antibody and a thiopurine is the
most effective strategy for inducing and maintaining
remission in luminal Crohn’s patients.
6
Maintenance therapy
• Immunosuppressive treatment with thiopurines (azathioprine
and mercaptopurine) forms the core of maintenance therapy, but
methotrexate is also effective and can be given once weekly,
either orally or by subcutaneous injection.
• Combination therapy with an immunosuppressant and an anti-
TNF antibody is the most effective strategy but costs are high and
there is an increased risk of serious adverse effects.
• Cigarette smokers should be strongly counselled to stop smoking
at every possible opportunity. Those that do not manage to stop
smoking fare much worse, with increased rates of relapse and
surgical intervention.

7
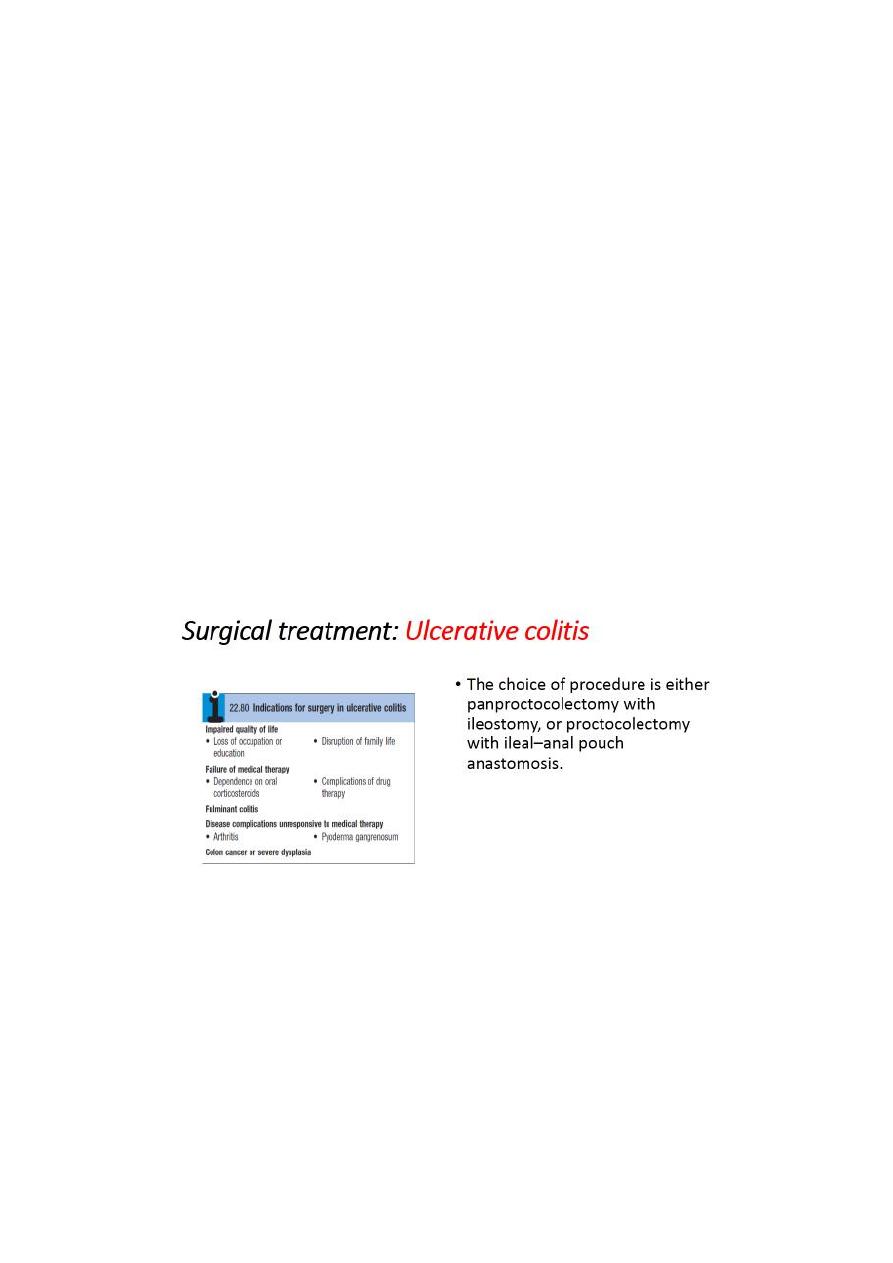
Surgical treatment: Crohn’s disease
• The indications for surgery are similar to those for ulcerative
colitis. Operations are often necessary to deal with fistulae,
abscesses and perianal disease, and may also be required to
relieve small or large bowel obstruction. In contrast to ulcerative
colitis, surgery is not curative and disease recurrence is the rule.
• Surgery should be as conservative as possible in order to minimize
loss of viable intestine and to avoid creation of a short bowel
syndrome.
Microscopic colitis
• Microscopic colitis, which comprises two related conditions,
lymphocytic colitis and collagenous colitis, has no known cause.
• The presentation is with watery diarrhoea. The colonoscopic
appearances are normal but histological examination of biopsies is
abnormal.
• Collagenous colitis is characterized by the presence of a
submucosal band of collagen, often with a chronic inflammatory
infiltrate.
• The disease is more common in women and may be may be
associated with rheumatoid arthritis, diabetes, coeliac disease and
some drug therapies, such as NSAIDs or PPIs.
• Treatment with budesonide is usually effective but the condition
will recur in some patients on discontinuation of therapy.
8
من هوني الخير المحاضرة مامهمة
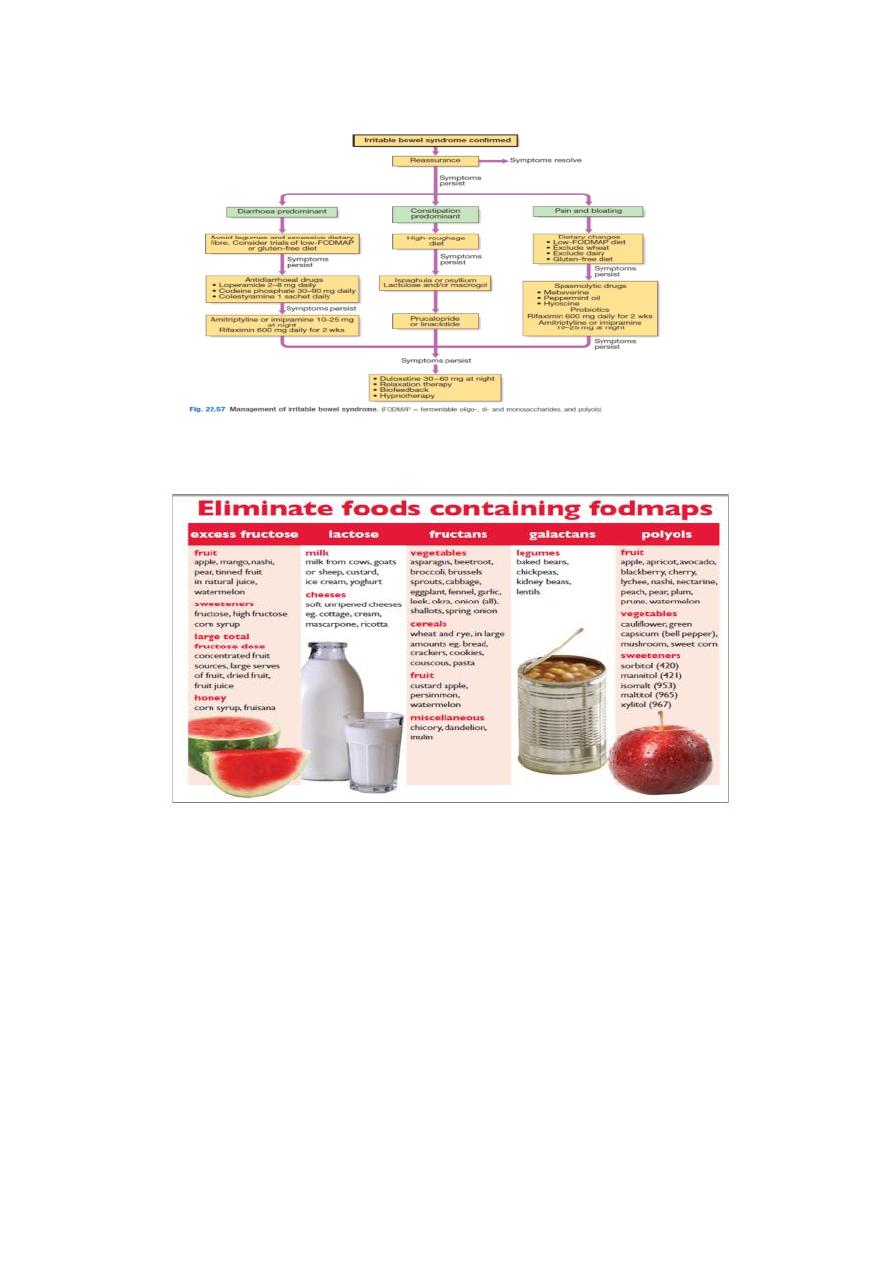
IRRITABLE BOWEL SYNDROME(IBS)
• About 10–15% of the population are affected at some time but only 10% of
these consult their doctors .
• Young women are affected 2–3 times more often than men.
• Coexisting conditions, such as non-ulcer dyspepsia, chronic fatigue
syndrome, dysmenorrhoea and fibromyalgia, are common.
• Between 5 and 10% of patients have a history of physical or sexual abuse.
9
11
11
12
13
14
