Fifth stage
pediatricLec-1
د.اثل
7/3/2016
EndocrinologyDiabetes Mellitus
Diabetes mellitus (DM) is a common, chronic, metabolic syndrome characterized by hyperglycemia as a cardinal biochemical feature.
ETIOLOGIC CLASSIFICATIONS OF DM
Type I diabetes: caused by deficiency of insulin secretion due to pancreatic β-cell damageImmune mediated
Idiopathic
Type 2 diabetes: a consequence of insulin resistance occurring at the level of skeletal muscle, liver, and adipose tissue, with various degrees of β-cell impairment.
Neonatal diabetes mellitus:
Transient—without recurrence
Transient—recurrence 7-20 yr later
Permanent from onset
Gestational diabetes mellitus.
Other specific types:
Genetic defects of β-cell function: MODY
Genetic defects in insulin action
Diseases of the exocrine pancreas: pancreatitis, trauma, pancreatectomy, neoplasia, cystic fibrosis, others.
Endocrinopathies: cushing disease, glucagonoma, pheochromocytoma, hyperthyroidism, others
Drug- or chemical-induced: glucocorticoids
Infections: congenital rubella, CMV
Uncommon forms of immune-mediated diabetes: Stiff-man syndrome
Genetic syndromes sometimes associated with diabetes: Down syndrome
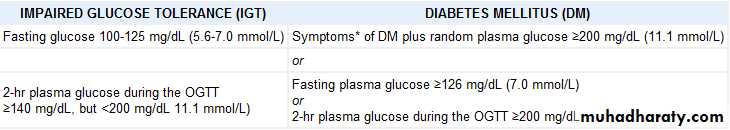
DIAGNOSTIC CRITERIA FOR IMPAIRED GLUCOSE TOLERANCE AND DIABETES MELLITUS
The criteria for making the diagnosis of diabetes are the same, regardless of the etiology
*In absence of unequivocal hyperglycemia, elevated plasma glucose concentration should be confirmed by repeat testing on different day.
*OGTT: 2 hr plasma glucose is obtained after1.75g/kg glucose(maximum of 75g) is ingested orally in the fasting state.
Clinical Presentation
The symptoms of hyperglycemia are similar regardless of the underlying cause and include:
Polyuria: typical complaints that suggest polyuria include the reemergence of bedwetting, new or increased nocturia, and disruption of class work in school for frequent visits to the bathroom or requests to get water to drink. These symptoms are typically only present for less than a month. This acute presentation most common in T1DM.
Polydipsia
Polyphagia
In cases of severe insulin deficiency weight loss, blurry vision, and fatigue.
May be asymptomatic if mild hyperglycemia is present.
The physiology that explains the sign & symptoms of diabetes:
Glucosuria serve as an osmotic force that increase water excretion. As urinary fluid losses increase, the thirst center is activated to work to maintain normal hydration.
The glucosuria also lead to loss of calories, this combined with the loss of the anabolic actions of insulin results in weight loss.
Evaluation
In evaluation a child for diabetes it is important to obtain:
Thorough history
Review of symptoms
Full physical examination
to ensure that the diagnosis of DM is made accurately as possible.
History should focus on:
Acuity of symptoms, as patient with diabetes resulting from insulin resistance often have an insidious course where as diabetes owing to insulin insufficiency is usually more acute in onset.
Insulin resistance adolescent may exhibit other signs of insulin resistance such as obesity, acanthosis nigricans of the neck, axillary area, knees, or inguinal creases, hypertension & in female a history of oligomenorrhea or even amenorrhea. (Calculation of BMI may help to quantify the degree of overweight)
Drug Hx.: to determine if the diabetes is as a result of medication.
Detailed family history: will allow detection of similarly affected family members, which become especially important when trying to ascertain if T2DM, MODY, or mitochondrial diabetes are possible diagnosis.
Presence of dysmorphic features especially in infant which can seen in various genetic & endocrine disorders that have diabetes as one of their manifestations.
Hx. of nausea, vomiting, abdominal pain, volume of urine output, fluid intake, difficulty of breathing, & alteration in mental status should be made, because patient may develop nonketotic hyperosmolar syndrome or ketosis.
The initial physical assesment should include:
Vital signs, with specific attention paid to the heart rate and blood pressure, as these may be abnormal if dehydration is present.
The presence of kussmaul respirations can serve as indicators of the patient’s acid/ base balance and suggest the presence of a significant metabolic acidosis.
Type 1 Diabetes Mellitus
Formerly called insulin-dependent diabetes mellitus (IDDM) or juvenile diabetes, T1DM is characterized by low or absent levels of endogenously produced insulin and dependence on exogenous insulin to prevent development of ketoacidosis, an acute life-threatening complication of T1DM.
Epidemiology
T1DM accounts for about 10% of all diabetes.
It accounts for most cases of diabetes in childhood.
Girls and boys are almost equally affected .
Peaks of presentation occur in 2 age groups: at 5-7 yr of age and at the time of puberty. The 1st peak may correspond to the time of increased exposure to infectious agents coincident with the beginning of school; the 2nd peak may correspond to the pubertal growth spurt induced by gonadal steroids and the increased pubertal growth hormone secretion (which antagonizes insulin).
Pathogenesis & natural history
DM1 is a chronic, T-cell mediated autoimmune disease that results in the destruction of the pancreatic islets. Genetic predisposition (HLA DR3 and HLA DR4 increase the risk of developing DM1).
and environmental factor lead to an initiation of an autoimmune process against the pancreatic islets. The autoimmune attack on the pancreatic islets leads to a gradual & progressive destruction of B-cells, with loss of insulin secretion.
Greater than 80% of the pancreatic B-cell must lost before a patient becomes sufficiently insulinopenic to develope hyperglycemia.
Regeneration of new islets has been detected at onset of T1DM, & it is responsible for the honey moon phase.
Environmental Influences:
Infections: viruses like coxsackie B3&B4, mumps, rubella &CMV can infect human B-cell. There is no convincing correlation between childhood vaccination & risk of T1DM.
Seasonal associations: seasonal variations are most apparent in the adolescent years, with greater frequency in autumn &winter months.
Dietary factors:
cow’s milk consumption has been found to be associated with a higher incidence of DM possibly because of the molecular mimicry between bovine serum albumin & B-cell antigen.
N-nitoso compounds derived from meat & vegetables in the gut increase the incidence of DM.
Body mass index: greater risk of DM1 among individuals who were heavier as young children.
Chemicals: some drugs & vacor are directly cytotoxic to B-cells.
Lower vitamin D levels increasing the risk of DM1.
Psychosocial stress may contribute as triggering for DM 1.
Multiple infections during the 1st year of life are associated with decreased risk of T1DM because exert modulatory effect on the immune system.
Exclusively breast fed infants are at lower risk of developing DM1.
Autoimmunity:
The immune reaction in DM1 includes the development of antibodies & T lymphocytes.
While B-cell autoantibodies are found in greater than 80% of patients at the time of diagnosis of DM1, they do not appear to play a direct role in B-cell destruction, which is T-cell mediated process.
Many different antibodies to beta cell antigens can be detected, including islet cell antibodies, insulin autoantibodies, antibodies to tyrosine phosphatase IA-2, and antibodies to glutamic acid decarboxylase.
Presentation of these autoantibodies considered important in priming then differentiation of T cells which secrete cytokines that cause destruction of B-cell progressively & also inhibit insulin secretion by the remaining healthy B-cells.
The risk of developing diabetes is highest in individuals with multiple B-cell autoantibodies, with a risk of developing diabetes within 5 years greater than 25% in those with two autoantibodies, & greater than 50% in those with three or more autoantibodies.
The natural history includes 4 distinct stages:
Preclinical β-cell autoimmunity with progressive defect of insulin secretion.
Onset of clinical diabetes.
Transient remission “honeymoon period”
Established diabetes associated with acute and chronic complications and decreased life expectancy.
Pathophysiology
Glucose and lipid metabolism are regulated by the pancreatic hormone Insulin,
and its Counter-regulatory hormones:
Glucagon
Growth hormone
Catecholamines
Cortisol
Insulin (anabolic(
Glucose used for energy substrate or stored as glycogen
Protein formation
Fats stored as triglycerides
Counter regulatory hormones (catabolic)
Glycogenolysis
Proteolysis-gluconeogenesis
Lypolysis-FFA & ketone bodies
To develop DM there must be both a relative lack of insulin and a relative over activity of counter-regulatory hormones
With moderate insulinopenia, glucose utilization by muscle and fat decreases and postprandial hyperglycemia appears. At even lower insulin levels, the liver produces excessive glucose via glycogenolysis and gluconeogenesis, and fasting hyperglycemia begins.
Hyperglycemia produces an osmotic diuresis (glycosuria) when the renal threshold is exceeded (180 mg/dL; 10 mmol/L). The resulting loss of calories and electrolytes, as well as the persistent dehydration, produce a physiologic stress with hypersecretion of stress hormones (epinephrine, cortisol, growth hormone, and glucagon).
These hormones, in turn, contribute to the metabolic decompensation by further impairing insulin secretion, by antagonizing its action, and by promoting glycogenolysis, gluconeogenesis, lipolysis, and ketogenesis while decreasing glucose utilization and glucose clearance.
The combination of insulin deficiency and elevated plasma values of the counter-regulatory hormones is also responsible for accelerated lipolysis and impaired lipid synthesis, with resulting increased plasma concentrations of total lipids, cholesterol, triglycerides, and free fatty acids. The hormonal interplay of insulin deficiency and glucagon excess shunts the free fatty acids into ketone body formation; the rate of formation of these ketone bodies, principally β-hydroxybutyrate and acetoacetate, exceeds the capacity for peripheral utilization and renal excretion. Accumulation of these keto acids results in metabolic acidosis (diabetic ketoacidosis)