Poisoning in children
DR.MOHAMMAD F. IBRAHEEMDEPARTMENT OF PEDIATRICS
FACULTY OF MEDICINE
objective
• Definition, circumstances, routes of Poisoning.• Definition of toxicology & toxidrome.
• Important history points in poisoning and specific management.
• Measures may be taken to prevent or decrease absorption
• Acetaminophen poisoning , features and management.
• Hydrocarbons poisoning , features and management.
• Caustics poisoning , features and management.
• Organophosphorous poisoning , features and management.
• Prevention of poisoning
Definition of Poisoning:
Exposure to a chemical or other agent that adversely affects functioning of an organism.
Circumstances of Exposure can be: -Intentional, accidental, environmental, medicinal or recreational.
Routes of exposure can be:-
Ingestion, injection, inhalation or cutaneous exposure.“All substances are poisons...the right dose separates poison from a remedy.”
Ingestion of a harmful substance is among the most common causes of injury to children less than six years of age.
Toxicology:-
Is the science that studies the harmful effects of drugs, environmental contaminants, and naturally occurring substances found in food, water, air and soil.Poisoning maybe a medical emergency depending on the substance involved.
A toxidrome is a syndrome caused by a dangerous level of toxin in the body, in 1970 by Mofenson and Greensher. It is often the consequence of a drug overdose, a systemic infection may also lead to a toxidrome. Major five toxidromes are:-
1-Anticholinergic
2-Sympathomimetic
3-Opiates
4-Cholinergic
5- Sedatives- Hypnotics/
Alcohol
Examples of poisoning:
ASAAcetaminophen
TCA
Narcotics & drugs of abuse
Benzodiazepines
Iron supplements
Alcohol
Organophosphorus
kerosene
Important history points
What toxic agent/medications were found near the patient?What medications are in the home?
What approximate amount of the “toxic” agent was ingested?
How much was available before the ingestion?
How much remained after the ingestion?
When did the ingestion occur ?
Were there any characteristic odors at the scene of the ingestion?
Was the patient alert on discovery?
Has the patient remained alert since the ingestion?
How has the patient behaved since the ingestion?
Does the patient have a history of substance abuse?
SPECIFIC management:
ABC’s of Toxicology:
Airway
Breathing
Circulation
Drugs:
Resuscitation medications if needed
Universal antidotes
Draw blood:
chemistry, coagulation, blood gases, drug levels
Decontaminate
Expose / Examine
Full vitals / Foley / Monitoring
Give specific antidotes / treatment
Decontamination:
Ocular:Flush eyes with saline
Dermal:
Remove contaminated clothing
Brush off
Irrigate skin
Gastro-intestinal:
Activated charcoal:
May Prevent /delay absorption of some drugs/toxins
Almost always indicated Only in the 1st hour !!!!
Naso/oro-gastric Lavage
Bowel Irrigation:
Recent ingestions
Awake alert patient
500 cc NS Children / 2000cc adults
Orally / Nasogastric tube
• PREVENTING ABSORPTION
• Activated Charcoal
• Cathartics
• Whole bowel irrigation
• Enhancing excretion
• Emesis
• Gastric Lavage
• Diuresis
• Dialysis
• Hemoperfusion
• Activated Charcoal:
• Decrease or prevent the intestinal absorption of a few drugs and toxins as well as enhance the elimination of drugs already absorbed and present within the systemic circulation .• specially prepared to have a very large adsorptive surface area.
• Many, but not all, toxins are adsorbed onto its surface.
Some toxins, including heavy metals, iron, lithium, hydrocarbons, cyanide, and low molecular weight alcohols, are not significantly bound to charcoal.
Dose of 10–50 g (≈1 g/kg) for a child and 50–100 g for an adolescent or an adult is administered. In practice.
Airway reflexes must be preserved or the airway
protected by endotracheal intubation.
it should only be considered for phenobarbital,
theophylline, phenytoin, carbamazepine, and
dapsone poisonings.
•
Specific toxidromes
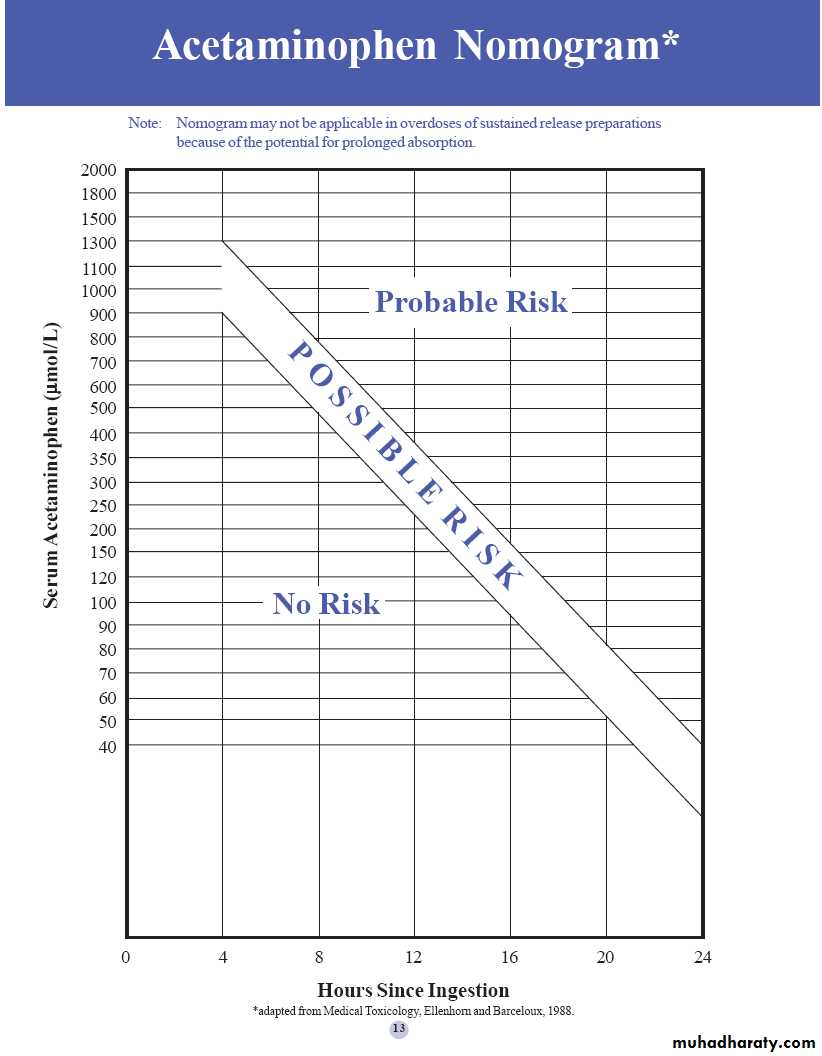
Acetaminophen:The chief target organ of acetaminophen poisoning is the liver, with the kidneys being involved in about 10 to 20% of those patients with hepatotoxicity.
Rarely, nephrotoxicity may occur without significant hepatic involvement. The dose required to produce significant hepatotoxicity in adults is 7.5 to 10.0 g.
The commonly stated hepatotoxic dose for children is 150 mg/kg.
Stage I: 0-24 hrs
Early symptomsMild
Serum acetaminophen level 4 hrs post ingestion
PLOT ON SPECIFIC NOMOGRAM.
If > 900 µmol/L ---> POSSIBLE RISK
Nausea, vomiting, malaise and diaphoresis.
Normal bilirubin Transaminases and PT.
Stage II: 24-48 hrs after ingestion.
Better, less symptoms.Elevated bilirubin, transaminases and PT
Stage III :48-96 hrs ( 2- 4 days) after ingestion
Hepatic dysfunction(Rarely hepatic failure)
Peak elevations in:
Bilirubin
Transaminases may reach > 1000 IU/L
Prolonged PT
Stage IV :168- 192 hrs (7-8 days)
Clinical improvementLFTs returning to normal
Probable toxicity should be treated with:-
N-acetylcysteine bolus 140 mg/kgThen 70 mg/kg Q 4 hrs for 17 doses.
Assess hepatic functions:-
On presentation
Daily
Continue other supports.
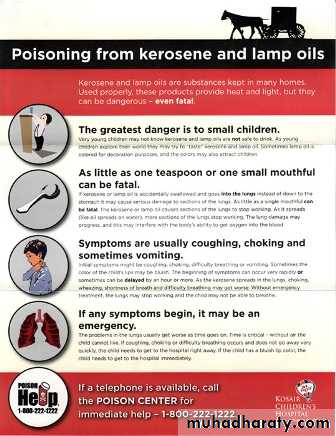
Hydrocarbons
Determination of the risk of aspiration pneumonitis :-1-low viscosity values, such as kerosene, gasoline, lighter fluid, turpentine, mineral seal oil, and mineral spirits, have the highest risk for aspiration. In contrast, more viscous hydrocarbons, such as petroleum, lubricating oil, and paraffin, represent a lower risk.
2-Surface tension. A low surface-tension chemical has the ability to creep or spread along a surface.
3-Volatility, the more volatile the agent, the greater the likelihood for adverse central nervous system effects.
Pathophysiology
These chemicals interfere with surfactant and directly irritate respiratory epithelium. The results are alveolar collapse, bronchospasm, direct damage to the airway epitheliumand endothelium, and
interstitial pneumonitis
resulting in ventilation
perfusion mismatch
and hypoxemia and
hypercapnia.
• Clinical Presentation :-
Kerosene ingestion:GIT effects Burning sensation, nausea, belching and diarrhea.
Respiratory effects Cough, tachypnoea ,tachycardia, cyanosis, pulmonary crepitations, rhonchi, chocking, gagging and grunting.CXR >6 hrs later: Pulmonary infiltrates or peri-hilar densities.
Pneumatoceles (2-3 w), pleural effusion or pneumothorax and bacterial super-infection( rare)
Resolution 2-7 days.
central nervous system effects may occur in at least a quarter of cases; lethargy and much less often semi-coma, coma and convulsions.
Bone marrow toxicity and haemolysis are not common but the clinician must be aware of the possibility of heart rhythm problems (such as atrial fibrillation and ventricular fibrillation).
hepatic and renal failure.
skin and mucous membranes Contact with the skin and mucous membranes may cause variable degrees of irritation up to the formation of bullae.
Management:-
1- Immediately remove the child from the source of the poisoning and ensure the airway is open (this is always the first priority).2- Remove contaminated clothing and thoroughly wash the skin with soap and water.
If possible perform pulse oximetry and give supplemental oxygen if indicated.
3- Intubation and mechanical ventilation may be needed in a patient with severe hypoxia, respiratory distress or decreased consciousness.
4- Avoid gastric lavage because of the risk of inhalation and hence pneumonitis. If very large amounts of kerosene have been ingested less than an hour earlier then lavage may be considered if the airway can be protected by expert intubation. 5- There is No evidence that corticosteroids are helpful. Some texts recommend the routine use of antibiotics but this remains controversial. 6- Admission to an intensive care unit is recommended for patients with early symptoms and signs of lower respiratory involvement because further deterioration of the respiratory function can be rapid.
Important points1- The vomiting should be discouraged ( bec. of risk of inhalation).2- CXR should not be done before 6 hours.3- No role of gastric lavage inhalation pneumonitis. 4- No role of steroid but antibiotics are controversial.
• Caustic or Corrosive Ingestion:-
The ingestion of strong alkalis or acids• The most commonly ingested alkali is sodium hydroxide.
The most commonly ingested acids are hydrochloric, phosphoric, and sulfuric acids.
They are found in (drain cleaners, oven cleaners, rust removers, toilet bowl cleaners, and tile cleaners).
Serious injury is associated with agents whose pH is >12 or <2.
Acids denature protein resulting in coagulation necrosis, while alkalis saponify fats and dissolve protein resulting in liquefaction necrosis.
Clinical presentation :-
The chief symptom is pain, which may be oral, thoracic, or abdominal depending on the site of caustic injury.Young children may manifest pain by crying, drooling, refusing to swallow, and vomiting.
Stridor or hoarseness usually indicates laryngeal injury. Rarely, hematemesis or melena may occur. Examination may find evidence of dermatologic or ocular burns. The presence of oral or pharyngeal burns does not predict the presence of esophageal or gastric injury. Conversely, the absence of oral or pharyngeal burns does not preclude distal injury, particularly if a liquid alkali or acid has been ingested. Full-thickness esophageal or gastric injury cause perforation or subsequent fistula formation.
• Management:-
• 1-support of vital functions, when these are threatened. Airway injury might necessitate endotracheal intubation or, in rare cases, performance of an emergency tracheostomy.• 2-Pain control with opioids and avoidance of fluid or solid ingestion are the principles of management.
3-Gastric decontamination with activated charcoal or gastric lavage is contraindicated. However, some clinicians advocate the administration of small volumes to dilute any remaining alkali or acid (controversy); If it is alkali vinegar or lemon juice diluted with an equal amount of water should be given, If it is acid one teaspoonful of the carbonate soda or washing soda mixed in a tumbler of water should be given.
4- Patients with alkali or acid caustic injury will require endoscopic evaluation and they may need surgical intervention. 5-Asymptomatic patients can be monitored for the development of symptoms. 6-A 12-hour symptom-free period usually indicates that no intervention will be needed.7-No role of ANTIBIOTICS nor STEROID.
Organophosphorus compounds
Organophosphorus compounds:Insecticides
Inhibition of Cholinesterase enzymes all over the body.
Muscarinic: N/V Abdominal pain/ fecal incontinence.
Cholinergic : cough, resp.secretions, crepitation and even pulmonary edema.
CVS : Tachycardia/ bradycardia/ block/ hypotension
Nicotinic: restlessness, confusion, coma, meiosis, flaccidity/convulsion.
C/F may be abbreviated by (DUMBBELS: Defecation , Urination, miosis, block(heart) bradycardia Emesis, Lacrimation and salivation).
Diagnosis: blood Cholinesterase levels
< 50% indicates poisoning.Atropine as test dose
Management:
A….B….C….. Stabilization
Wash hair and body with soap & water
Consider Gastric lavage if within 1hr
Atropine sulphate I.V. till pupils are normal size.
Dose = 0.02 mg/kg Q 15-20 mins
Atropine sulphate I.V. till pupils are normal size.
Remember…Atropine has no effect on muscle paralysis must support breathing
USE
Cholinesterase reactivator such as Pralidoxime
Dose = 1gm /kg IV Q 30 mins
Prevention:-
The reduction in the incidence of childhood poisonings in the past half-century has been dramatic.This reduction is largely the result of the combination of highly effective active and passive methods of intervention.
1- Passive interventions e.g.: introduction of child-resistant containers for drugs and other dangerous household products. Child-resistant containers have been particularly effective in reducing the incidence of death from the ingestion of prescription drugs by children.
2- Active interventions, which require a change in behavior by parents and caretakers, include the safe storage of household products.
Summary
1- Poisoning is exposure to a chemical or other agent that adversely affects functioning of an organism.2-ABC’s of Toxicology: Airway, Breathing, Circulation, Drugs, Draw blood,
3- Decontaminate,Expose / Examine, Full vitals / Foley / Monitoring, Give specific antidotes / treatment.
4-Acetaminophen poisoning mainly affect the liver.
5-Kerosene poisoning mainly affect the resp. system.
6-Prevention of poisoning (u) maintained by passive and active intervention
THANK YOU