
1
4th stage
Surgery
Lec
Dr.Smair
28/2/2016
Gastritis
Type A gastritis :
Autoimmune Ab against parietal cell
Gastric atrophy----achlorhydria
Malabsorption of B12 Pernicious anaemia
Sparing of antrum ----hypergastrinaemia----
Hypertrophy of ELC
Predispose to gastric cancer
Type B gastritis :
Due HP infection
Affect the antrum
Prone to peptic ulceration
Reflux Gastritis:
Enterogastric reflux
Common after gastric surgery
Occasionally found after cholecystectomy
Treatment:
Bile chelating or prokinetic agent
Revisional surgery
2
Erosive gastritis:
Caused by agents that disturb the gastric mucosal barrier; like NSAIDs and
alcohol.
NSAID inhibition of Cox1 PG
Cox2 inhibitors type of NSAID act as anti inflammatory without affection on
gastric barrier
Stress gastritis
A common sequel of serious illness or injury
May follow cardiopulmonary bypass
Attributed to a reduction of blood supply to superficial mucosa of stomach
May lead to stress ulceration that may bleed
Treatment: Prevention; routine use of H2 antagonists, + -mucosal barrier agents
like sucralfate
Peptic Ulcer
Not related to pepsin
All can be healed by using proton pump inhibitors
Can occur in the:
1. 1stpart of duodenum,
2. lesser curve of stomach
3. stoma of gastrojejunostomy,
4. oesophagus,
5.
Meckel’s diverticulum
3
Aetiology:
Gastric acid secretion:
In DU usually above normal
In Gu normal
Gastrinoma”Zollinger-Ellison syndrome”
Healing can occur only in the absence of acid
H.pylori infection:is the most important factor
NSAIDs ingestion
Cigarette smoking, predispose to peptic ulcer
Duodenal Ulceration
Incidence
:
Decrease in its incidence
Peak incidence is now in a much older ages
Less marked difference between male and female.
Bleeding and perforation is seen more in the elderly.
Pathology
:
Most common in the 1stpart of duodenum
Penetrates the mucosa and into the muscle coat
Healing by fibrosis deformity stenosis
Healed ulcer leave a permanent scar
May be more than one ulcer
Anterior ulcer perforate
Posterior ulcer bleed

4
Histopatholgy:
Destruction of muscular coat
Base of ulcer is covered with granulation tissue
Endarteritis obliterance of surrounding arteries
Gastric Ulcers
Incidence
:
Less common than DU
Sex incidence is equal
Affected patients are older than DU patients
More prevalent in low socioeconomic groups
More common in developing world than the west
Aetiology
:
H.pyloriinfection
NSAIDs
Smoking
Pathology:
Similar to that of DU
Fibrosis Hour glass deformity
Penetration
Lesser curve of the stomach

5
Malignancy in gastric ulcers:
GU may be associated with gastric malignancy
Benign Gu may change into gastric cancer
A malignant gastric ulcer from the start
All GU should be regarded as being malignant until proved otherwise usually
by well targeted multiple biopsis “as many as10”
Clinical features of peptic ulcers
Pain: epigastric, gnawing, may radiate to back, eating may relieve the
discomfort, intermittent
Periodicity:intermittent, spring and autmen
Vomiting:indicates stenosis
Alteration in weight: wt loss or gain may occur ,,, wt loss more with GU
Bleeding: all may bleed; may be:
chronic anaemia
acute presentation with hematemesis and melaena
Clinical examination
Epigastric tenderness
Investigation :
Gastroduodenoscopy:
Investigation of choice
Highly specific and sensitive
Diagnosis:
Visual
Biopsy for any abnormal lesion in the stomach
Antral biopsy for H.pylori “CLO test, histology”
6
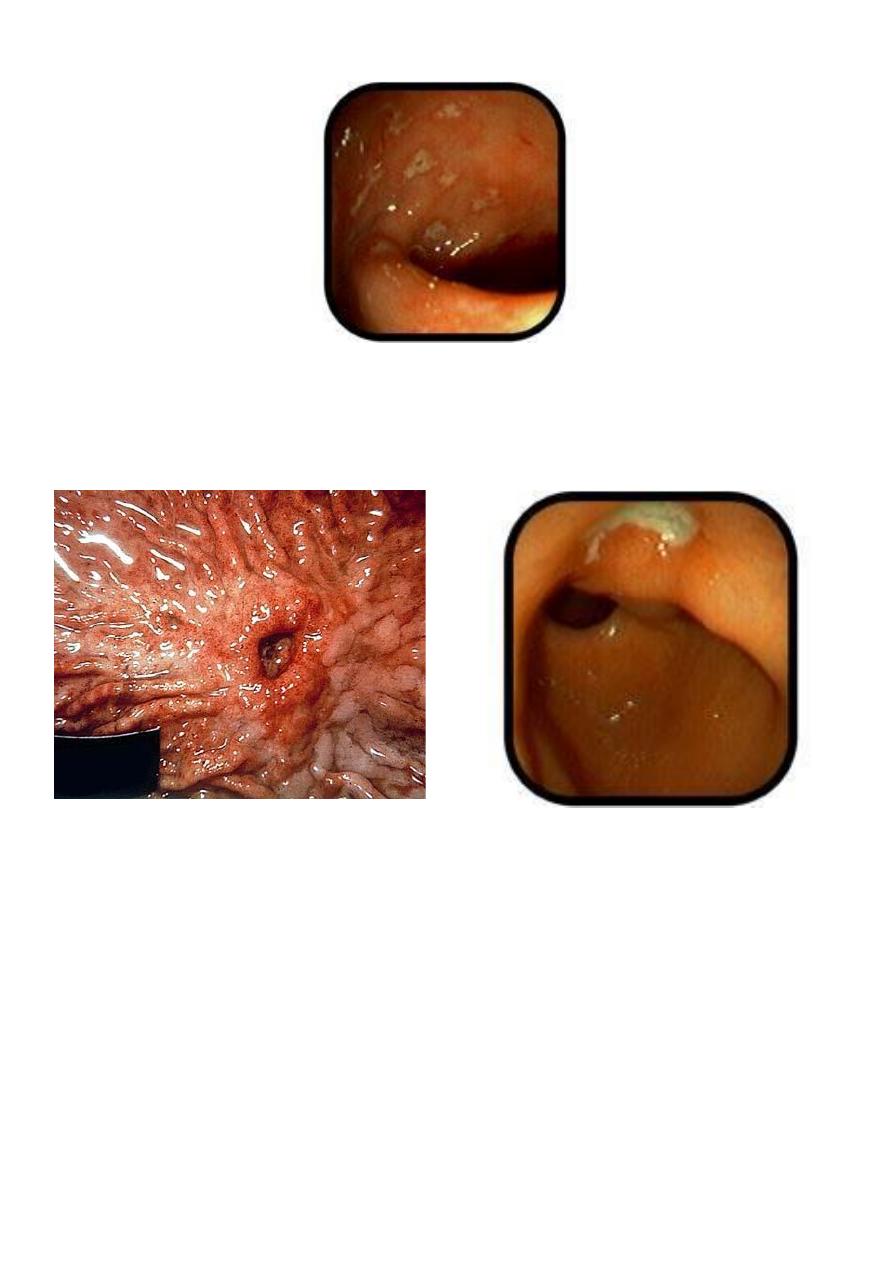
Dudenal ulceration
Gastric Ulcer
Endoscopic view
Treatment of peptic ulceration :
Medical treatment:
Proton pump inhibitors; omeprazol, lansoprazol
Eradication therapy; is now routinely given to patients with peptic ulceration
except in patients with :
NSAID induced ulcers.
Stomal ulcers
Zollinger-Ellison syndrome

7
Surgical treatment of uncomplicated DU ulceration :
Peptic ulcer surgery is now of little more than historical interest
Operations for duodenal ulcer
1. Truncal vagotomy and drainage
2. Highly selective vagotomy
3. Truncal vagotomy and antrectomy
4. Billroth II gastrectomy
Protocol for GU :
Dx of benign ulcer must be confirmed by Biopsy
Give Medical treatment
Endoscopic checking to ensure complete healing of the ulcer 6-8 wks later
If un-healed ------Surgery
Operations for gastric ulcer :
1. Billroth I gastrectomy
2. Billroth II gastrectomy
3. Vagotomy, pyloroplasty and ulcer excision
Sequelae of peptic ulcer surgery :
Recurrent ulceration
Small stomach syndrome
Bile vomiting
Early and late dumping

8
Post-vagotomy diarrhoea
Malignant transformation
Nutritional consequences
Gall stones
Complications of peptic ulceration
Perforation
Bleeding
stenosis
Perforated peptic ulcer
Epidemiology:
Increase in the age
Increase in the incidence in females
Pathology:
The ulcers that are liable for perforation are:
Anterior Du
Anterior or incisuralgastric ulcers
Clinical features
:
History of peptic ulceration
Sudden onset of severe generalised abdominal pain
Avoid movement
May be shocked with tachycardia
The abdomen dose not move with respiration

9
Board like rigidity
Investigations:
Erect plain chest radiograph
Air under the diaphragm in about 50
–70 % of cases
Serum amylase
Ct scan for both perforated DU and pancrititis
Water soluble contrast swallow --free peritoneal leak
Diagnostic peritoneal lavage
Treatment:
Resuscitation
Analgesia
Surgery
Laparotomy
Laparoscopy
Peritoneal toilet
Closure of perforation
