
AFTER MID
TOTAL LEC: 15
Dermatology
Lichen Planus
DR. SABEEH LEC: 2
Dr. Sabeeh


Dermatology
Dr. Sabeeh, Lec 2
March 2, 2016
Lichen Planus
Objectives :
• To define and list the common papulo squamous diseases.
• Able to recognise clinical features, diagnosis complications and treatment of lichen
planus.
• Able to define ,diagnose and treat pityriasis rosea.
Common Papulo-Squamous diseases
(scaly rashes or scaly erythematous rashes)
A.
Psoriasis
B.
Lichen planus
C.
Pityriasis rosea
D.
Tinea corporis
E.
Pityriasis versicolor
F.
Discoid eczema
G.
Seborheic dermatitis
H.
Secondary syphilis
I.
Drug eruptions
Lichen planus
Lichen planus (Greek leichen, “tree moss” , Latin planus “flat” )
is a common inflammatory disorder that affects the skin, mucous
membranes, nails, and hair
The four Ps—purple, polygonal, pruritic, papule
How common is Lichen planus?
At least two-thirds of cases occur between the ages of 30 and 60 years of age.
Male to female ratio is one (equal).
LEC : 2
!1
طحالب
Aetiology :
It is an immunologic mechanisms mediate the development of lichen planus.
Cell-mediated immunity plays the major role in triggering the clinical
expression of the disease.
(Both
CD4+
and
CD8+
)T cells are found in lesional skin.
CD8+
T cells are cytotoxic cells attacking basal keratinocytes.
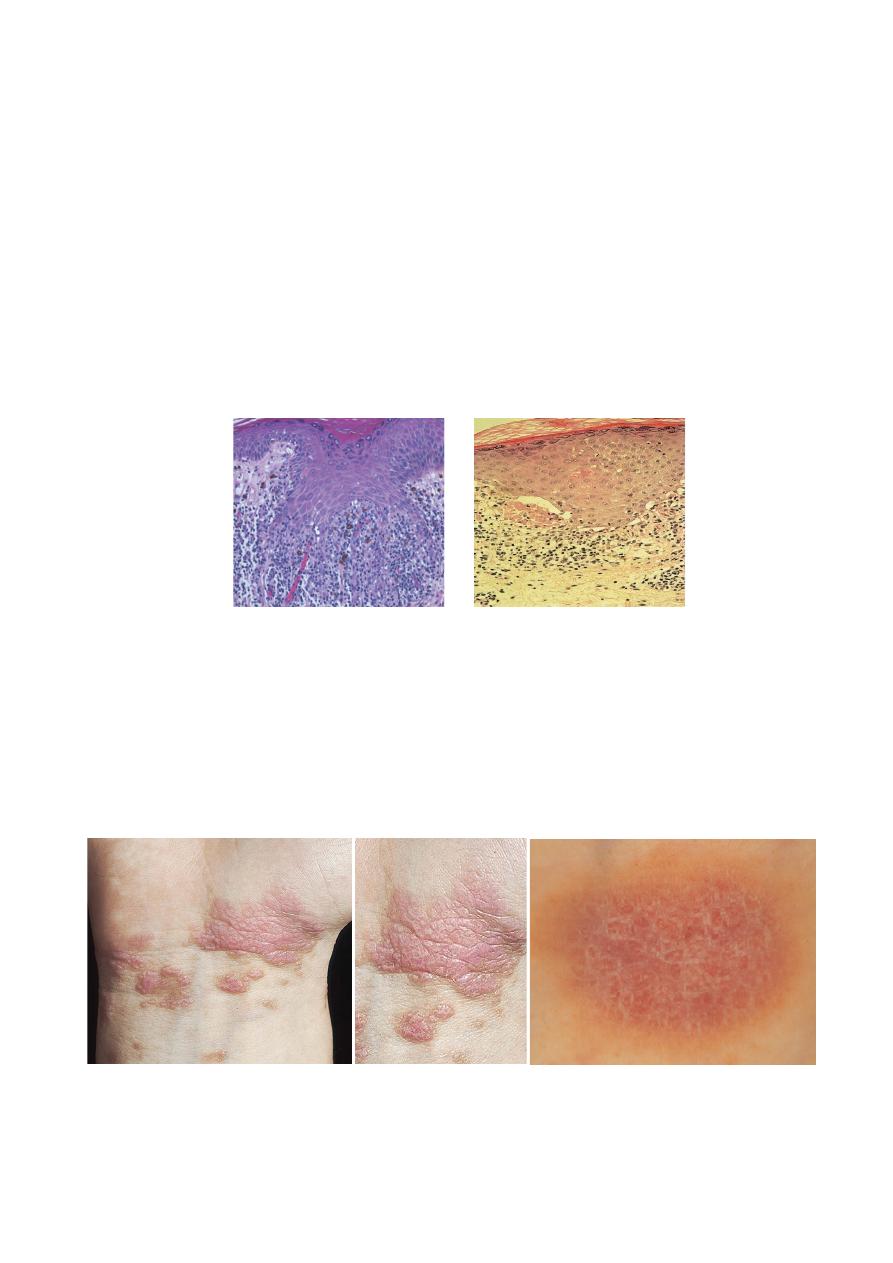
Pathology:
Basal epidermal keratinocyte damage and lichenoid interface lymphocytic
reaction.
Description :
• Lesions: Symmetric, grouped, erythematous to violaceous, flat-topped, polygonal
papules. (4Ps).
• Wickham’s striae (white network). (MCQ)
• Distribution: Widespread, predilection for flexural aspects of arms and legs.
LEC : 2
!2
Wickham’s Striae
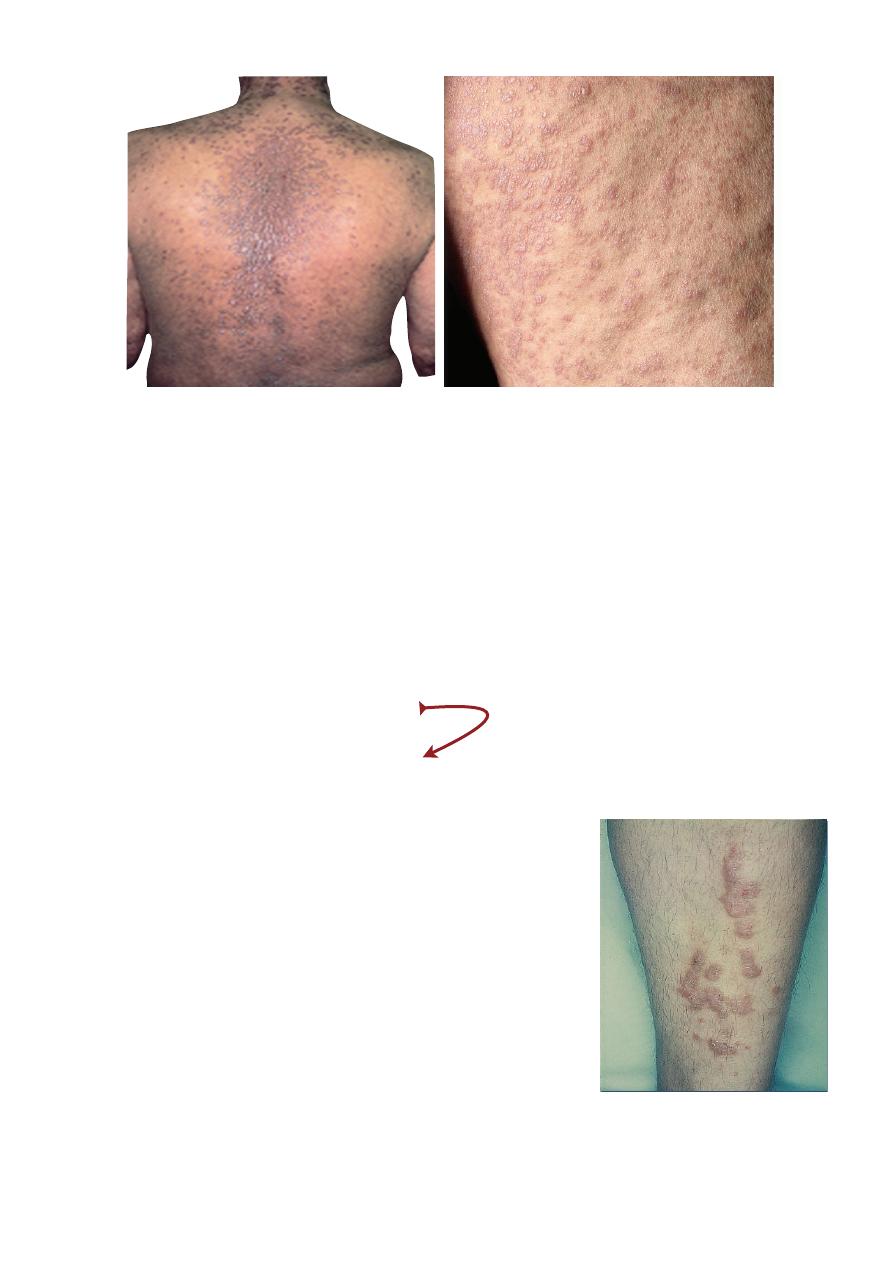
CONFIGURATION OF LESIONS
A. Annular Lichen Planus:
• They occur in blacks and are more common on the penis and scrotum
• Actinic lichen planus, seen in subtropical zones on sun-exposed, dark-skinned
young adults and children.
B. Linear Lichen Planus:
• Papules of lichen planus may develop a linear pattern secondary to trauma
(koebnerization).
Clinical variants according to
MORPHOLOGY OF LESIONS
A. Hypertrophic
Occurs on the extremities and tends to be the
most pruritic variant lesions are thickened and
elevated, purplish or reddish-brown in color, and
hyperkeratotic.
B. Vesiculo bullous Lichen
The development of vesicles and bullae within
the lesions, Bulla arising in oral can lead to painful
erosions.
C. Erosive and Ulcerative
D. Follicular
Sites of predilection include the trunk and the
scalp.
LEC : 2
!3
The thickened lesions characteristic of
hypertrophic lichen planus on the shins.

SITE of INVOLVEMENT
A. Mouth examination > Mucosal lichen planus.
B. Nail examination > Lichen planus of nail.
C. Scalp examination > Lichen planopilaris.
Complications:
A. Permanent nail loss.
B. Scarring alopecia.
Course:
A. last for one year
B. Hypertrophic many years
C. Leave brown macules
Treatment:
• The mainstay of treatment for lichen planus is
strong topical corticosteroids
.
•
Resistant localized lesions, such as on the shins, may be treated with
intralesional
steroids
or with steroids
under occlusive dressings
.
•
Systemic treatment
of lichen planus has traditionally been with
corticosteroids
,
usually at doses equivalent to 20–40mg prednisolone initially, reduced over a period
of a few weeks.
•
Cyclosporine
appears to be the most consistently useful.
PUVA photo
chemotherapy
.
Question?
Wickham's striae is characteristically seen in :
A. Pityriasis rosea.
B. Lichen planus.
C. Psoriasis.
D. Pityriasis versicolor.
E. Tinea corporis.
LEC : 2
!4
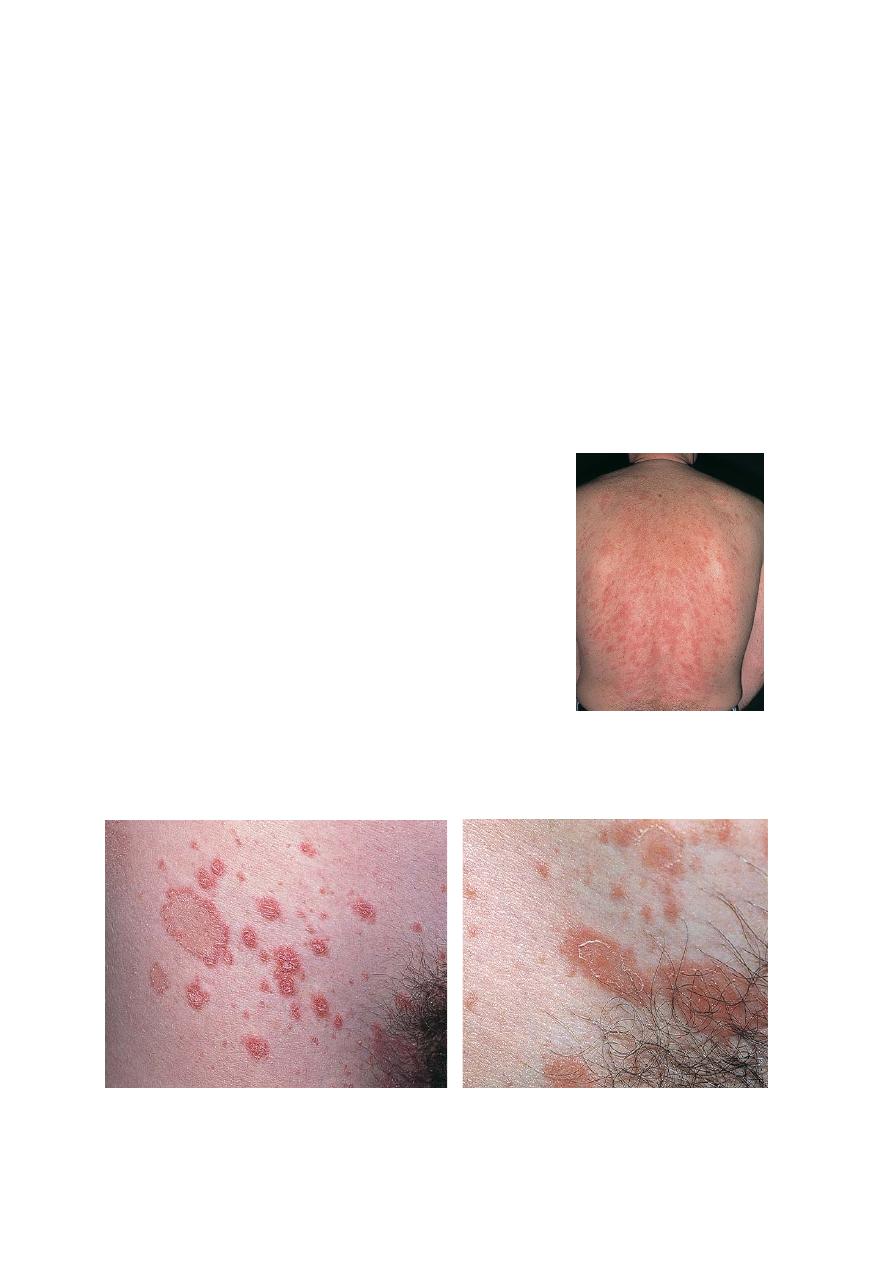
Pityriasis rosea
A. Pityriasis rosea is self-limiting acute exanthematous eruption with a distinctive
morphology.
B. First, a single (primary, or "herald") plaque lesion develops, usually on the trunk,
and 1 or 2 weeks later a generalised secondary eruption develops in a typical
distribution pattern.
C. Remits spontaneously in 6 weeks.
D. 50% itching.
E. There is some evidence that it is viral in origin
F. Age of Onset:
10 to 40 years, but can occur rarely in infants and old persons.
G. Season:
Spring and fall.
H. Etiology
Herpes virus type 7 is suspected.
Differential Diagnosis:
Tinea corporis
—>
Herald patch.
More than 3 months —>
Guttate psoriasis.
Secondary syphilis.
LEC : 2
!5
Collarette scale

Scarring alopacia
occurs in:
A. Psoriasis
B. Pityriasis alba
C. Pityriasis rosea
D. Seborrheic dermatitis
E. Lichen planopilaris
Treatment
A. It usually causes few symptoms, but a topical corticosteroid speeds up the
resolution.
B. Oral erythromycin daily (1 gm in four equally divided doses for 2 weeks in adults).
C. Ultraviolet light B (UVB), administered in five consecutive daily erythemogenic
exposures, results in decreased pruritus and hastens the involution of lesions.
Summery
• Scaly erythematous rashs patchy or papular may resemble psroriais
• History, location and clinical features may facilitate diagnosis and some time
even lab test and biopsy are
• Needed
• Lichen with its four P (4P
s
) may end in serious complications.
• While pity rosea is self limmiting which may similate tinea corporis for its herald
patch and secondary of syphlis in the wide spread stage
ز
LEC : 2
!6
LEC : 2
!7
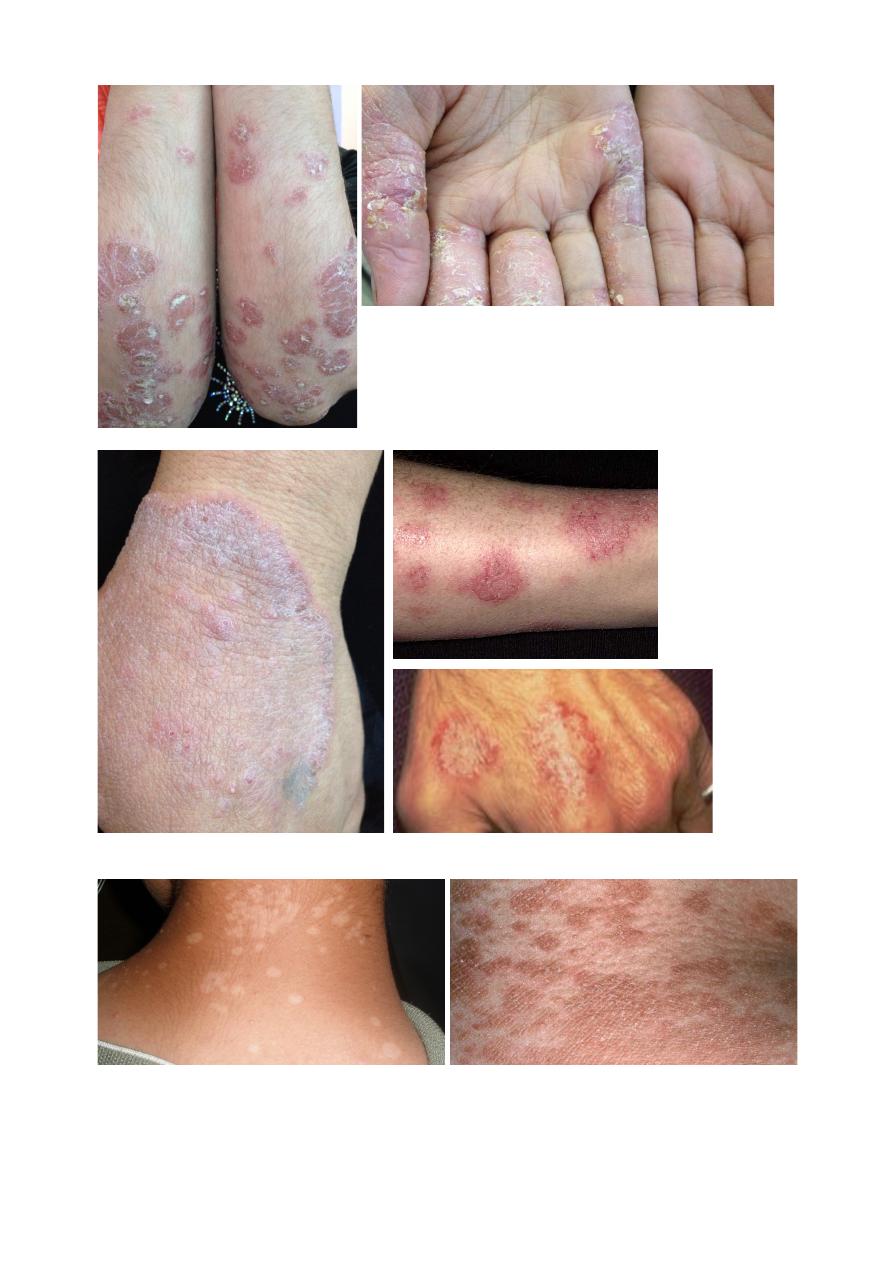
1.
2.
Psoriasis
T
inea
Co
rp
orus
2.
1.
a. b. c.
a.
b.
c.
I.
II.
Pityriasis versicolor
I. II.

