AFTER MID
LEC: 15
DR. NAJAH
Ophthalmology
The Lens
TOTAL LEC: 10
Dr. Najah
1
2015 -2016 Baghdad medical college
Lens
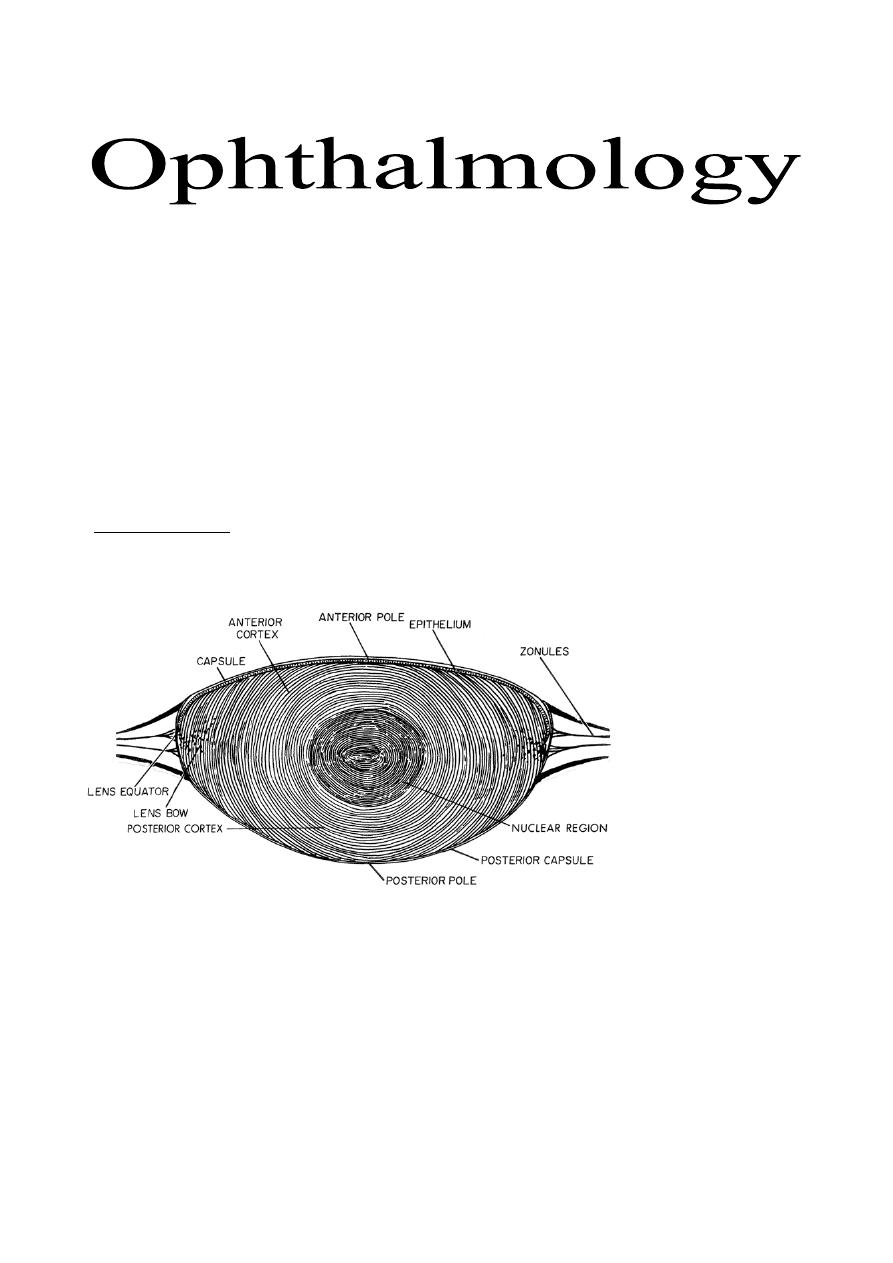
Anatomy of the lens
The crystalline lens is a biconvex, avascular transparent structure enclosed
by a capsule.
The lens consists of:
1- Nucleus: the central compacted core, which represents the older lens fibers
which are formed during intrauterine life and early years of life.
2- Cortex: represents the newly formed epithelial cells, which elongate to
form new lens fibers (softer than nucleus) situated around the old fibers
(nucleus). These new lens fibers are continuously laid down subcapsularly
throughout life, resulting in that the older layers acquire progressively deeper
localizations within the lens.
3- The capsule: which is the thickest basement membrane in the body and
responsible for molding the lens substance during accommodation.
- A ring of zonular fibers, which insert in the equatorial region, suspends the
lens from the ciliary body. As the zonule keeps the lens attached to the ciliary
body, it can mould and change the shape of the lens during accommodation.
Contraction of the ciliary muscles causing decrease in the tension of zonule on
the lens capsule which is change the lens shape to more sphere by its elasticity
and increasing the power of lens. "Accommodation"
- The lens grows in both anteroposterior and equatorial dimensions throughout
life. It is the only organ in the body which is continuously grows to the end of
life.
Dr. Najah
Lectures: 15 & 16
B
Cross
section
through
the lens

2
Symptoms and signs of diseases of lens:
1- Cataract: lead to painless gradual impairment visual acuity.
2- Presbyopia: decrease in amplitude of accommodation (due to decreased
elasticity) leading impairment of near vision.
3- Nuclear sclerosis: lead to increase the difference between the refractive
indices of the nucleus and cortex causes "index (lenticular) myopia".
4- Monocular diplopia: due to opacification or tilting of lens producing two
images in the same eye due to diffraction of light.
Cataract
- The normal lens is transparent, any congenital or acquired opacity in the lens
or its capsule, irrespective to the effect on vision, is a cataract.
Types of cataract:
1- According to its site within the lens:
a- Posterior subcapsular: just anterior to the posterior capsule.
b- Anterior subcapsular: just posterior to the anterior capsule.
c- Cortical: cataract involving the cortex.
d- Nuclear: cataract involving the nucleus.
Cataract can be detected by slit-lamp, direct ophthalmoscope (as black dots
in the red reflex or total loss of red reflex if it is mature), B-scan and even by
naked eye as leukocoria (white pupil) when it is mature.
2- According to maturation:
a- Immature: if there is involvement of part of lens (any part), and other
parts are still transparent.
b- Mature: complete opacification of the entire lens.
c- Hypermature Cataract: is a mature cataract in which there is partial
liquefaction of the cortex, leakage of resultant fluids from the lens towards
aqueous humor, shrinkage of lens and folding of capsule. So, the size of the
lens becomes smaller than when it is mature.
d- A morgagnian cataract is a hypermature cataract in which the total
liquefaction of the cortex has allowed the nucleus to sink inferiorly.
e- Intumescent Cataract (phacomorphic cataract): In case of immature or
mature cataract, if there is influx of fluids from aqueous humor towards lens
lead to swelling of the lens. Some time, this swelling will progress to a level
sufficient to occlude the angle of AC results in "Intumescent Glaucoma".
3- According to its onset: into either acquired or congenital.

3
Acquired cataract
Causes:
1- Age-related cataract: due to biochemical changes that occur with
advancing age in the proteinaceous matter of the lens converting soluble into
insoluble protein causing opacification, usually develops after the age of 60.
2- Pre-senile cataract: develops before the age of 60 in the following
conditions:
a- Diabetes Mellitus: high level of glucose in the lens is metabolized into
sorbitol by aldose reductase, and then accumulation of sorbitol causes
secondary osmotic over hydration, refractive changes (Myopia), and then
cataract. (hypoglycemia is another example of metabolic causes in addition to
DM)
b- Myotonic dystrophy: 90% of patients develop cataract in the third decade.
c- Atopic dermatitis: 10% of patients with severe atopic dermatitis develop
cataract in the second to fourth decades of life.
d- Neurofibromatosis type 2.
3- Traumatic cataract: trauma is the most common cause of unilateral
cataract in young individuals:
a- Direct penetrating injury to the lens.
b- Concussion by blunt.
c- Electrical shock is a rare cause.
d- Ionizing radiation.
e- Infrared radiation; as in glassblowers.
4- Drug-induced cataract:
a- Steroids: both systemic and topical steroids are cataractogenic.
b- Chlorpromazine: both corneal and lenticular deposits are dose related and
usually irreversible, high dose (>2400 mg daily) may cause retinotoxicity.
c- Amiodarone (anti-arrhythmic): lens deposits occur in 50% of patients.
d- Gold: lens deposits occur in 50% of patients on treatment for longer than 3
years.
e- Allopurinol: used in hyperuricaemia and chronic gout.
5- Secondary cataract: is a complicated (secondary) cataract develops as a
result of some other primary ocular disease:
a- Chronic anterior uveitis: it is the most common cause of secondary
cataract.
b- Acute congestive angle-closure glaucoma.
c- High (pathological) myopia.
d- Hereditary fundus dystrophies, such as retinitis pigmentosa.

4
Treatment of catract:
SURGERY
.
There is NO effective medical treatment
Indications of surgery:
1- Visual improvement: is the most common indication, whether it is mature
or immature. If the patient feels that his vision is not enough to perform daily
requirements, surgery is indicated.
2- Medical indications: e.g., Intumescent Cataract (phacomorphic cataract)
which might lead to intumescent glaucoma. Other example is dense cataract
impaired visualization of retina or its laser treatment in diabetic patients.
3- Cosmetic indication: is rare, as mature cataract causing white pupil
(Leukocoria). The cataract is associated with untreatable other condition like
advance optic nerve atrophy or long standing retinal detachment.
Anesthesia used is general, local, and topical. Choices one of them is according
to method of surgery, general health of the patient and surgeon preference.
Types of cataract surgery:
1- Extracapsular cataract extraction (ECCE) + PC IOL (posterior
chamber intraocular lens):
→
Here a smaller incision 8-10 mm, about 120°-140° of the circumference of
cornea or limbus. The anterior capsule only is cut near to its periphery and
removes it (Capsulotomy). Then, the nucleus is extracted out, and the retained
lens material (cortex) is taken out by fluid irrigation and aspiration. Therefore,
the posterior capsule and the peripheral part of anterior capsule are still
attached in its position to the Zonules. Finally, PC IOL is implanted in the bag
between the posterior capsule and the peripheral part of anterior capsule (in the
position of previous cataractous lens). This operation is characterized by
having less length incision, rapider rehabilitation, less astigmatism and less
incidence of vitreous loss because the posterior capsule is still there.
2- Phacoemulsification + PC IOL: most recent method, 2.8 to 3.2 mm
incision + foldable or injectable IOL, suture less because the incision is so
small.
Like ECCE, anterior capsule is removed but the nucleus is not delivered as a
one piece but it emulsified and fragmented into small pieces by high frequency
mechanical partitioned machine (its frequency is nearly equal to the frequency
of ultrasound) or by laser. So, there is no need to do a large incision like in
5
ECCE. The remnant of cortex is also removed by irrigating and aspirating
fluid. Finally, implantation of a foldable or injectable lens manufactured of
soft material can be inserted into the PC through this small wound. This
operation does not need suture and patient can leave hospital at the day of
surgery and resume his life after few days. Astigmatism is either minor degree
or nil because the incision is so small.
Aphakia
Congenital or acquired absence of the lens from the eye, or its absence from
the pupillary area (luxated). An aphakic eye is usually strongly hypermetropic
where parallel rays of light are brought to a focus behind the retina.
All accommodation is abolished (why?)
Treatment:
1- High powered convex lenses in spectacles: High power spectacles lens
causing magnification of the images on the retina (about 30% magnification),
which will produce anisoconia (different sizes of image on the retina coming
from the 2 eyes). Normal eye sending normal size image while aphakic eye
with high power spectacle producing large image (30%). The cerebral cortex
cannot fuse those 2 images with such high difference in their sizes result in
diplopia. Other disadvantages of high power spectacles are including,
limitation of visual field and heavy weight.
* Cerebral cortex cannot fuse images difference in more than 5%. Therefore
any difference which is more than 5% causing diplopia.
2- Contact lens (1% magnification). This is can be used without diplopia in
aphakic eye if the other eye is phakic or pseudophakic.
3- IOL (intraocular lens): is the best way of correction as there is no
magnification at all.
Congenital cataract
Occurs in about 3:10.000 live birth, 2/3
rd
of cases are bilateral.
Causes:
1- Isolated hereditary cataracts:
Account for about 25% of cases, mode of inheritance is most frequently AD
(Autosomal dominant), yet AR (Autosomal Recessive) and X-linked
inheritance can occur.
2- Metabolic cataract:
a- galactosaemia (Galactose -1-phosphate uridyl transferase "GPUT").
b- Lowe's (oculocerebral) syndrome: rare inborn error of amino acid
metabolism which predominantly affects boys (X-linked).
3- Prenatal infections:

6
a- Congenital Rubella: cataract presents in 15% of cases.
b- Others: Cytomegalovirus, Herpes simplex and Varicella.
4- Chromosomal abnormalities:
a- Down syndrome (Triosomy 21).
b- Other: Patau syndrome (Triosomy 13), Edward syndrome
Treatment:
SURGERY
.
Assessment of the density of cataract is usually done through visualization of
retina by direct and indirect ophthalmoscope. If the cataract is so dense,
visualization of retina is difficult or impossible then surgery is indicated.
Surgery is by lensectomy (removal of the entire cataractous lens) + anterior
vitrectomy (removal of anterior surface of the vitreous just posterior to the lens)
should be done with it as opacification of anterior vitreous face occur in 100%
of Childs after surgery. Lensectomy and anterior vitrectomy done by special
machine called vitrectomy machine.
Correction of aphakia in congenital cataract:
1- Unilateral aphakia: either IOL or contact lens (NO role for glasses).why?
2- Bilateral aphakia: in addition to IOL and contact lens, it can be corrected
by spectacles.
Ectopia lentis
Is refers to a displacement of the lens from its normal position. The lens may
be completely dislocated "Luxated" (complete destruction or cut of zonules) or
partially dislocated "Subluxated".
Causes:
1- Acquired:
- Trauma.
- Large eye {high myopia, buphthalmus (congenital glaucoma)}, due to
stretching of zonules that causes their destruction.
- Anterior uveal tumour, as it pushes the lens away from the ciliary body
leading to destruction of zonules.
- Hypermature cataract because of redundant capsule.
2- Congenital:
a- Without systemic association: AD, AR or associated with aniridia
(congenital absence of iris).
b-With systemic association: e.g., Marfan's syndrome, Weill-Marchesani
syndrome, homocystinuria, Ehlers-Danlos syndrome.

7
Complications of ectopia lentis:
1- Refractive errors: myopia (as the lens moves forward) and astigmatism (as
the lens is tilted).
2- Glaucoma: due to pupillary block that raises the pressure inside the
posterior chamber that pushes and bows the iris anteriorly "Iris bombé" and
causes obstruction of the angle of the anterior chamber ending with glaucoma.
3- Endothelial touch: damage to the endothelium of cornea.
4- Lens induced uveitis: rare, occurs due leakage of lens matter to the
intraocular cavities where it is regarded as foreign body, so there will be
inflammatory reaction causing uveitis.
Treatment of ectopia lentis:
Indications for treatment:
1- Refractive error: treated by spectacles and surgery if not corrected by
spectacles.
2- Glaucoma: - If the lens is clear, do YAG PI (Yttrium-Aluminum-Garnet
Peripheral Iridotomy, where there is creation of a fistula
between anterior and posterior chamber through a hole at the
periphery of iris).
- If there is cataract, the treatment is lens extraction.
3- Endothelial touch → removal of lens.
4- Lens induced uveitis (which is chronic) → removal of lens.
The end



