
Nutrition
Dr. Mohamed
“ Breast Feeding ”
Total Lec: 32
cont.
DR. MOHAMMAD F. IBRAHEEM
DEPARTMENT OF PEDIATRICS
INFANT FEEDING (2)
Objectives
• Formula feeding and types
• Weaning
• First year feeding problems
• Over feeding
• Regurgitation
• Colic
• Constipation
Formula Feeding
Most women make their feeding choices for their infant early in pregnancy.
The usual intake to allow a weight gain of 25-30 g/day will be 140-200
ml/kg/day in the first 3 mo of life.
But after that, the rate of weight gain declines.
Vomiting and spitting up are common, and when weight gain and general well-
being are noted, no change in formula is necessary.
In addition to complementary foods introduced between 4 and 6 mo. of age,
continued breast-feeding or the use of infant formula for the entire 1st year of
life should be encouraged.
1-COW’S MILK PROTEIN–BASED FORMULAS
The protein concentration varying from 1.45 to 1.6 g/dl, considerably higher than
in mature breast milk (~1 g/dl). The predominant whey protein is β-globulin in
bovine milk and α-lactalbumin in human milk. Plant or a mixture of plant and
animal oils are the source of fat in infant formulas. Lactose is the major
carbohydrate in mother’s milk and in standard cow’s milk–based infant formulas
for term infants.
2-SOY FORMULAS
Free of cow’s milk protein and lactose and provide 67 kcal/dl. The protein is a
soy isolate supplemented with l-methionine, l-carnitine, and taurine to provide a
protein content of 2.45-2.8 g per 100 kcal or 1.65-1.9 g/dL.
Indications:-
a) Galactosemia.
b) Hereditary lactase deficiency.
c) Situations in which a vegetarian diet is preferred.
3-PROTEIN HYDROLYSATE FORMULA
May be partially hydrolyzed, containing oligopeptides with a molecular weight of
<5000 d, or extensively hydrolyzed, containing peptides with a molecular weight
<3000 d.
Indications:-
a) Infants intolerant to cow’s milk or soy proteins.
b) Gastrointestinal malabsorption due to cystic fibrosis, short gut syndrome,
and prolonged diarrhea.
c) e.g. Nutramigen. Pregestemil. Aptamil pepti.
4-AMINO ACID FORMULAS
Are peptide-free formulas that contain mixtures of essential and nonessential
amino acids. They are specifically designed for infants with dairy protein allergy
who failed to thrive on extensively hydrolyzed protein formulas.
Whole cow’s milk is not recommended under one year of age because:
1-Intolerance occurs.
2-Increase incidence of iron def. anemia.
3-Contains more solutes that the kidneys of small babies cannot cope with.
Weaning
Weaning is the process of gradually introducing a mammal infant to what will be
its adult diet and withdrawing the supply of its mother's milk.
When's the best time to start weaning?
The AAP recommends exclusive breast-feeding for the first six months after birth
— and breast-feeding in combination with solids foods until at least age 1.
Extended breast-feeding is recommended as the mother and her baby wish to
continue.
Still, when to start weaning your child is a personal decision.
Whenever the mother chooses to start weaning her baby from the breast, stay
focused on her child's needs as well as her own.
Resist comparing your situation with that of other families
Are there certain times when it wouldn't be smart to start weaning?
Consider delaying weaning if:
• Concerned about allergens.
Might prevent or delay eczema, cow's milk allergy, and wheezing in
early childhood.
• The child isn't feeling well.
If the child is ill or teething, postpone weaning until he or she is feeling
better.
• A major change has occurred at home. Avoid initiating weaning during a
time of major change at home. If the family has recently moved or the
child care situation has changed, for example, postpone weaning until a
less stressful time.
What's the best way to begin weaning?
When you start the weaning process, take it slow—over the course of weeks or
months —
Will cause milk supply to gradually diminish and prevent discomfort caused by
engorgement.
(Treated by applying cold compresses to the breasts to help decrease swelling
and discomfort).
Keep in mind that children tend to be more attached to the first and last
feedings of the day, when the need for comfort is greater.
These feedings might be the last ones your child drops. As a result, it might be
easier to drop a midday breast-feeding session first.
After a lunch of solid food, your child might become interested in an activity and
naturally give up this session.
Once you've successfully dropped one feeding, you can start working on
dropping another.
You might also choose to wean the baby from breast milk during the day but
continue breast-feeding at night.
Remember, it's up to the mom and her child.
First year feeding problems:
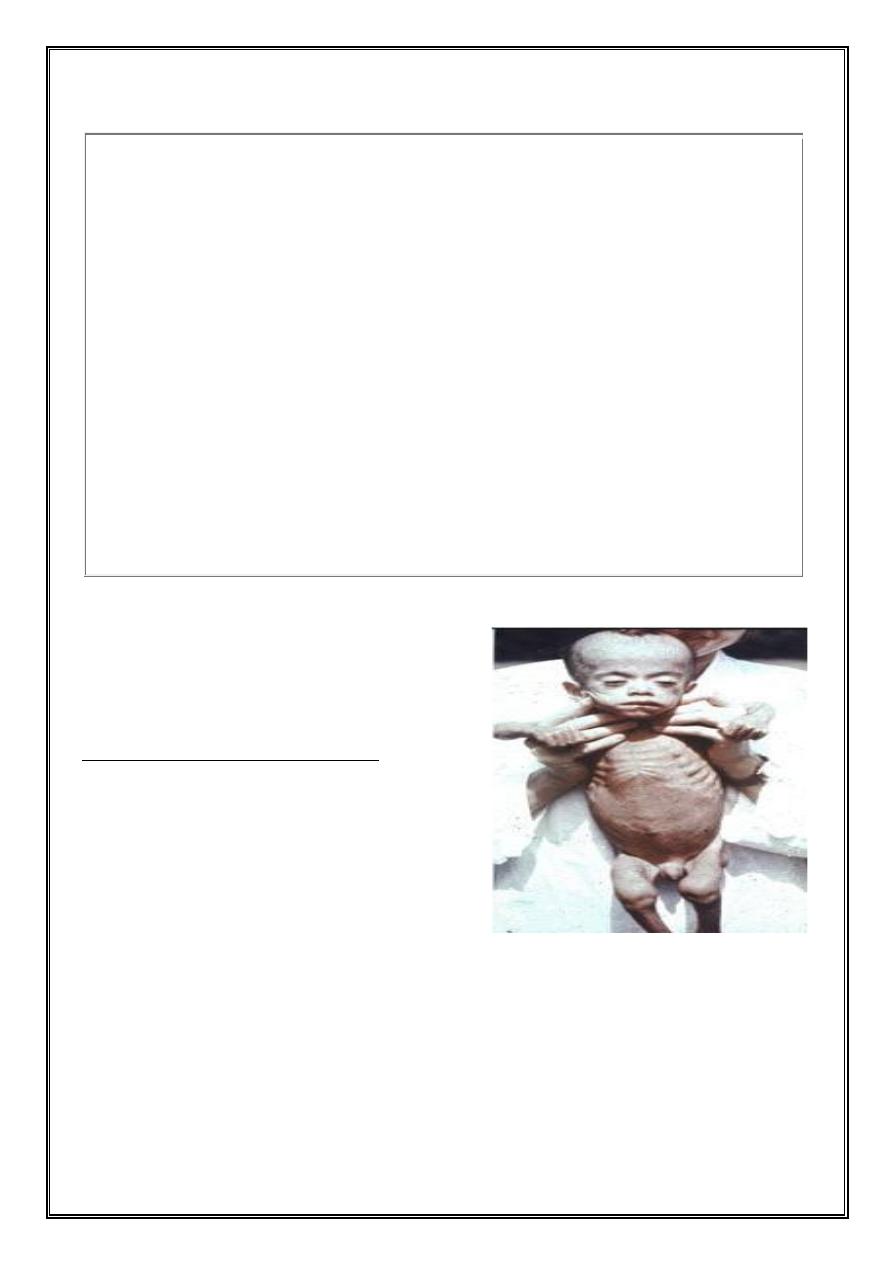
Under feeding:
It is suggestive by crying, restlessness &
failure to gain wt. adequately despite
complete emptying of the breast or the
bottle. It is also result from the failure to
take sufficient quantities of food even when
offered.
The child will not gain wt. and actually he will lose wt. and become Marasmic
(looks as an old man and loose the muscle bulk. Constipation, failure to sleep,
irritability, and excessive crying are to be expected).
The child will be def. in vit. A, B, C, D; Fe. Def. anemia & protein def. also.
Important Principles for Weaning
Begin at ≈ 6 mo of age
Avoid foods with high allergenic potential (cow's milk, eggs, fish, nuts,
soybeans).
At the proper age, encourage a cup rather than a bottle.
Introduce 1 food at a time.
Energy density should exceed that of breast milk.
Iron-containing foods (meat, iron-supplemented cereals) are required.
Zinc intake should be encouraged with foods such as meat, dairy products,
wheat, and rice.
Phytate intake should be low to enhance mineral absorption.
Breast milk should continue to 12 mo; formula or cow's milk is then
substituted.Give no more than 24 oz/day of cow's milk.
Fluids other than breast milk, formula, and water should be discouraged. Give
no more than 4–6 oz/day of fruit juices. No soda.
Treatment:
Treatment of underfeeding includes:-
1. Increasing nutrient intake.
2. Correcting any deficiencies of vitamins
and/or minerals.
3. And instructing the caregiver in the art
and practice of infant feeding.
4. If an underlying systemic disease, child
abuse or neglect, or a psychologic
problem is responsible, specific management of that disorder is necessary
Over feeding:
Which is either quantitative or qualitative.
Regurgitation & vomiting are the major symptoms.
• Diet high in fat --delay gastric emptying—distention & discomfort- inc. wt.
• Diet high in CHO—fermentation in int.—distention &flatulence— inc. wt.
In both cases there will be deficiency of protein, ess.A.A. Vits. & minerals.
*Too high calories esp. in the first two weeks of life
will cause loose stool (osmotic diarrhea).
Regurgitation:
Definition: Return of small amounts of swallowed food
during or shortly after feeding; within limit it is normal
and called (Posseting) which occurs during the first 6
mon. of life.
Colic:
Definition: It is a complex of paroxysmal abdominal
pain presumably of intestinal origin. It is of
unknown cause. But recent studies suggest that it
has some relation to irritable bowel syndrome in
adults of the same family.
It is common in babies and called (3 months colic), there will be an unexplained
irritability & severe crying, it occurs usually in the afternoon. Careful physical
exam. to exclude other causes of colic as:
Intussusception,
Strangulated hernia,
Otitis media,
Pyelonephritis,….etc.
Factors that play part in colic:-
§
Hunger---crying---swallowing air--- vicious
cycle.
§
Increase CHO in the diet -----fermentation ----
distention----colic.
§
Allergy to cow milk.
Treatment:
1-Holding the infant upright or prone across the lap
or on a hot water bottle or heating pad occasionally
helps.
2- Passage of flatus or fecal material spontaneously
or with expulsion of a suppository or enema sometimes
affords relief.
3-Carminatives before feedings are ineffective in
preventing the attacks.
4-Sedation is occasionally indicated for a prolonged
attack.
5-If other measures fail; both the child and the parent
may be sedated for a period.
6- In extreme cases, temporary hospitalization of the
infant, often with no more than a change in the feeding routine and a period of
rest for the parent may help.
7- Prevention of attacks should be sought by improving feeding techniques,
including:-
a-“Burping.”
b- Providing a stable emotional environment.
c- Identifying possibly allergenic foods in the infant's or nursing mother's
diet.
d- And avoiding underfeeding or overfeeding.
Although it is not serious, colic can be particularly
disturbing for the parents as well as the infant.
Thus, a supportive and sympathetic physician can be
particularly helpful, even if attacks do not resolve
immediately.
The fact that the condition rarely persists beyond 3 mo. of age should be
reassuring.
CONSTIPATION
Constipation is infrequent bowel movements or
difficult passage of stools.
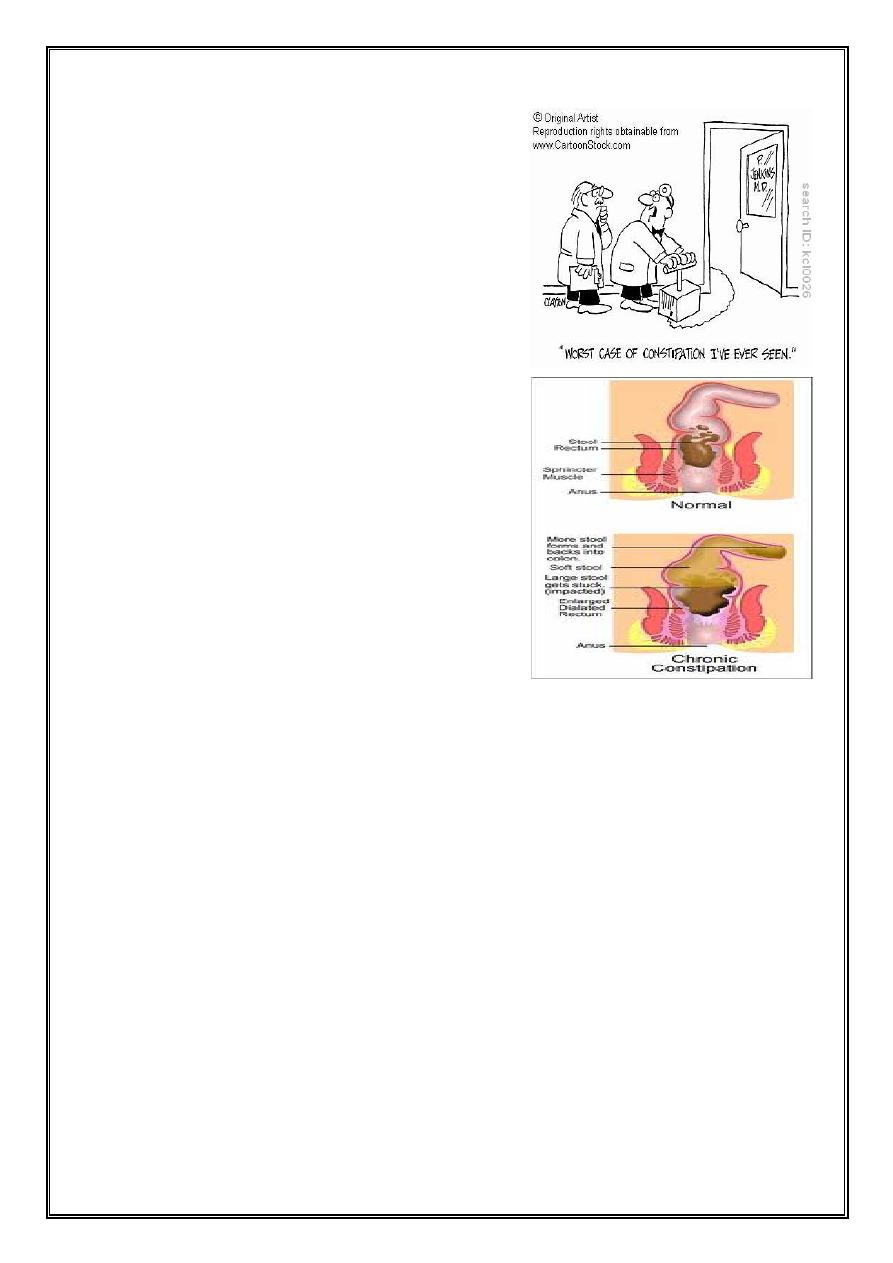
Obstipation
Is intractable constipation.
Constipation is practically unknown in breast-
fed infants receiving an adequate amount of
milk and is rare in formula-fed infants receiving
an adequate intake.
The consistency of the stool, not its frequency,
is the basis for diagnosis. Most infants have 1 or
more stools daily, but some occasionally have a
stool of normal consistency at intervals of up to
36–48 hr.
Whenever constipation or obstipation is present
from birth or shortly after birth, a rectal
examination should be performed. Tight or
spastic anal sphincters may occasionally be
responsible for obstipation, and finger dilation
is frequently corrective. Spastic anal sphincters
may occasionally be responsible
If irritation is alleviated, healing usually occurs quickly.
Aganglionic megacolon may be manifested by constipation in early infancy; the
absence of stool in the rectum on digital examination suggests this possibility,
but further diagnostic work-up is indicated.
Constipation may be caused by :-
§
An insufficient amount of food or fluid.
§
Diets those are too high in protein or deficient in
bulk. Simply increasing the amount of fluid or
sugar in the formula may be corrective during the
1st few months of life. After this age, better
results are obtained by adding or increasing the intakes of cereal,
vegetables, and fruits.
Prune juice (½–1 oz) may be helpful, but adding
foods with some bulk is usually more effective. Milk
of magnesia may be given in doses of 1–2 tsp, but
should be reserved for unresponsive or severe
constipation. Enemas and suppositories should
never be more than temporary measures.
Summary
• There are different types of formula feeding
which includes: -
1-ordinary formulas. 2- Formulas prepared for
special purpose.
• Weaning (u) begin between 4-6 mo.
• Under feeding & overfeeding should be avoided
• Differentiation between pathol. From non-
pathol. throw up.
• Colics in the first 3mo. Of life is very common non pathol. Problems.
• Constipation should be managed properly.
THANK YOU
