
Medicine
Dr. Akram
Neurology
“MULTIPLE SCLEROSIS”
Prof. Akram AI-Mahdawi
LECTURE 11
Multiple Sclerosis Prof. Akram Al.Mahdawi
2
Multiple Sclerosis
Objectives
What is demyelination disease?
How would you diagnose MS?
What are the different treatment options?
History of disease
Multiple Sclerosis, also known as MS, was given its name, multiple
because of the numerous sites of demyelination and ‘sclerosis’ which
means scarring.
“There are accounts of probable MS dating back to the 14th century but
the history of the disease really begins in the 19th century with the first
illustrations and clear clinical description of the disease beginning to
appear in 1838”.
The first actual case was first diagnosed in 1849. It was Jean-Martin
Charcot who is credited with giving us the first signs and symptoms of
Multiple Sclerosis.
Pierre Marie Charcot
The Disease (MS) without his name is
meaningless! His students are: Babinski & Sigmund Feroid
Facts
It is an Immune mediated disease.
It is a life-long disease with no cure.
MS, the body attacks and destroys myelin that insulates an axon/nerve
(demyelination )
If damage is severe it can also destroy the nerve/axon itself.
MS affects the central nervous system and inflames the white matter in
the brain which creates plaques
This box added by students (it is not included in the lecture):
White matter
is composed of bundles of myelinated nerve cell projections (or axons), which
connect various
grey matter
areas (the locations of nerve cell bodies) of the brain to each
other, and carry nerve impulses between neurons.
Myelin acts
as an insulator, increasing
the speed of transmission of all nerve signals
Multiple Sclerosis Prof. Akram Al.Mahdawi
3
Multiple sclerosis
Most common disabling condition in young adults
Most common demyelinating disorder
Chronic disease of the CNS
Progresses to disability in majority of cases
Unpredictable course / variety of signs and symptoms.
Current theory favors immunologic pathogenesis
Women 2 to 3 times as men
It is rare in the pediatric
MS is rare after age of 60
MS is uncommon in equatorial climates but increase with northern
distance from equator (More in cold northern countries)
Pathophysiology
Both genetic and environment
Low near the equator and increase in temperate
Sunlight, Vitamin D and
Epstein–Barr virus
Familial 15%, monozygotic twins 30%
Polygenic
Immunological-T lymphocyte in CSF and increase immunoglobulin
synthesis in CNS
Entry of activated T lymphocyte
Recognized antigen-presenting cell (microglia).
Inflammatory cascade lead to release cytokines and initiate destruction
of oligodendrocyte-myelin unit by macrophage
Damage myelin associated with inflammatory infiltrate of lymphocyte,
macrophage, antibody, complement deposition, activated microglia and
oligodendroglia cell.
Inflammation + demylination= plaque= gliosis
Mainly select periventricular, optic nerve & subpial region of spinal cord
Absence of myelin will lead to:
1. Conduction abnormalities (delay, blocked, Impairment) lead to negative
symptoms & signs (visual loss, weakness, ataxia and numbness)
2. Emphatic conduction-positive signs and symptoms (pain, paroxysmal
syndrome)

Multiple Sclerosis Prof. Akram Al.Mahdawi
4
Common initial Symptoms:
(Important!)
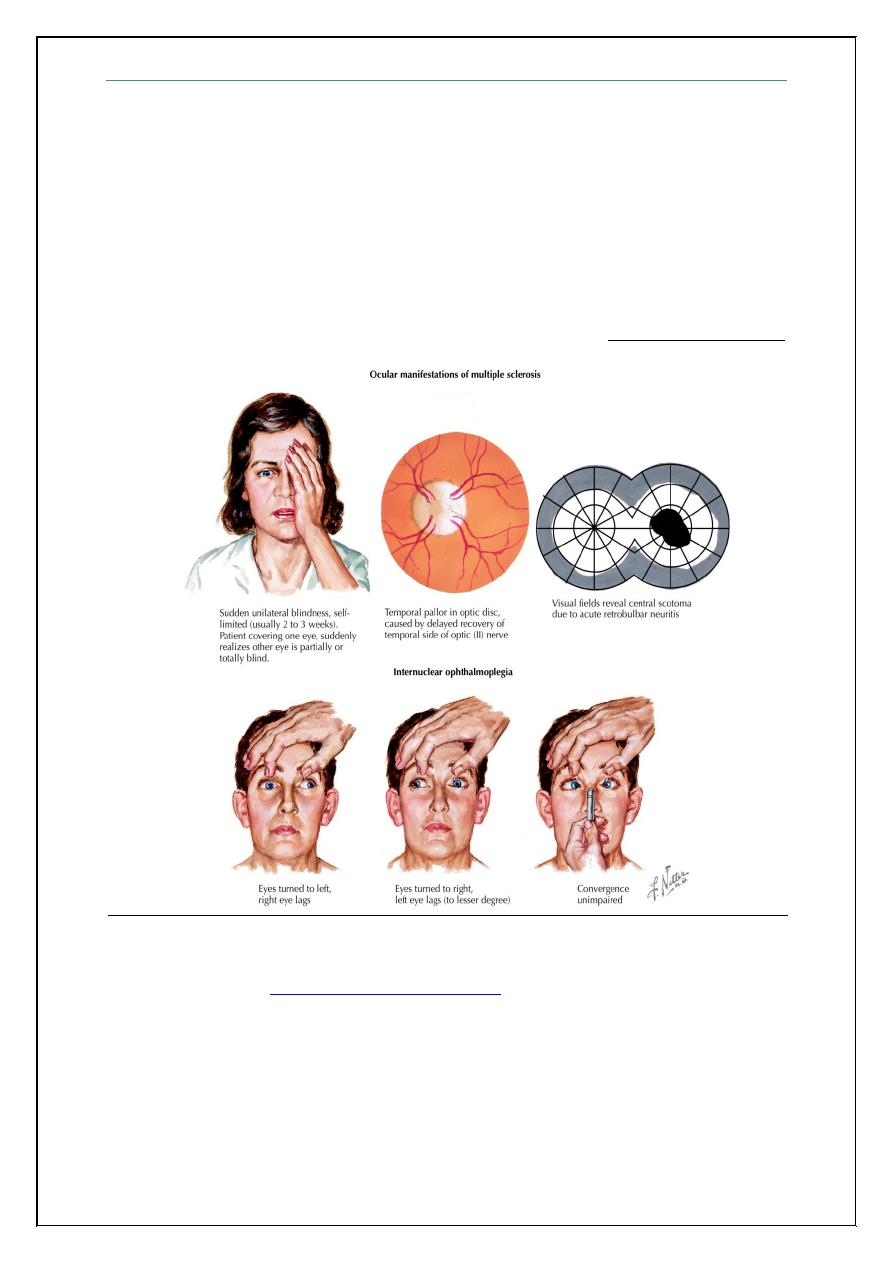
Optic neuritis*
Relapsing and remitting (RR) sensory symptoms
Subacute painless spinal cord lesion (transverse mylitis)
Acute brain-stem syndrome
Subacute dorsal column deficit
Case Presentation:
A 20-year – old female. She had three episodes (Relapsing and remitting) of
neurological symptoms including
1- An episode of hemiparesis lasting 3 weeks
2- One episode of optic neuritis in left eye lasting 2 weeks
3- Episode of paresthesias of both legs and lower abdomen with reduce
bladder sensation with residual symptoms
Condition suggestive of MS ?
(Important!)
Afferent pupillary defect and optic atrophy (Marcus Gunn pupil)
Lhermitts symptom
(
is an electrical sensation that runs down the back and into the limbs. In
many patients, it is elicited by bending the head forward. It can also be evoked when a practitioner
pounds on the posterior cervical spine while the neck is flexed; this is caused by involvement of the
posterior columns and has many causes not only MS)
Internuclear opthalmoplagia (INO)
Rubral, holmes tremor
Trigeminal neuralgia under the age of 50
Recurrent facial nerve palsy
Urinary sphincter disturbance
Mentioned by Dr. Akram
Optic neuritis: Sudden, painful (especially on eye movement) visual loss with impaired color
vision.
We have to differentiate it from Anterior Ischemic optic neuropathy which is painless
visual loss and has 2 types: Artertic and non artertic (giant cell arteritis.)
Mentioned by Dr. Akram
Marcus Gunn pupil: is a
medical sign observed during the
swinging-flashlight test where
upon the patient's pupils constrict
less (therefore appearing to
dilate) when a bright light is
swung from the unaffected eye to
the affected eye.
Multiple Sclerosis Prof. Akram Al.Mahdawi
5
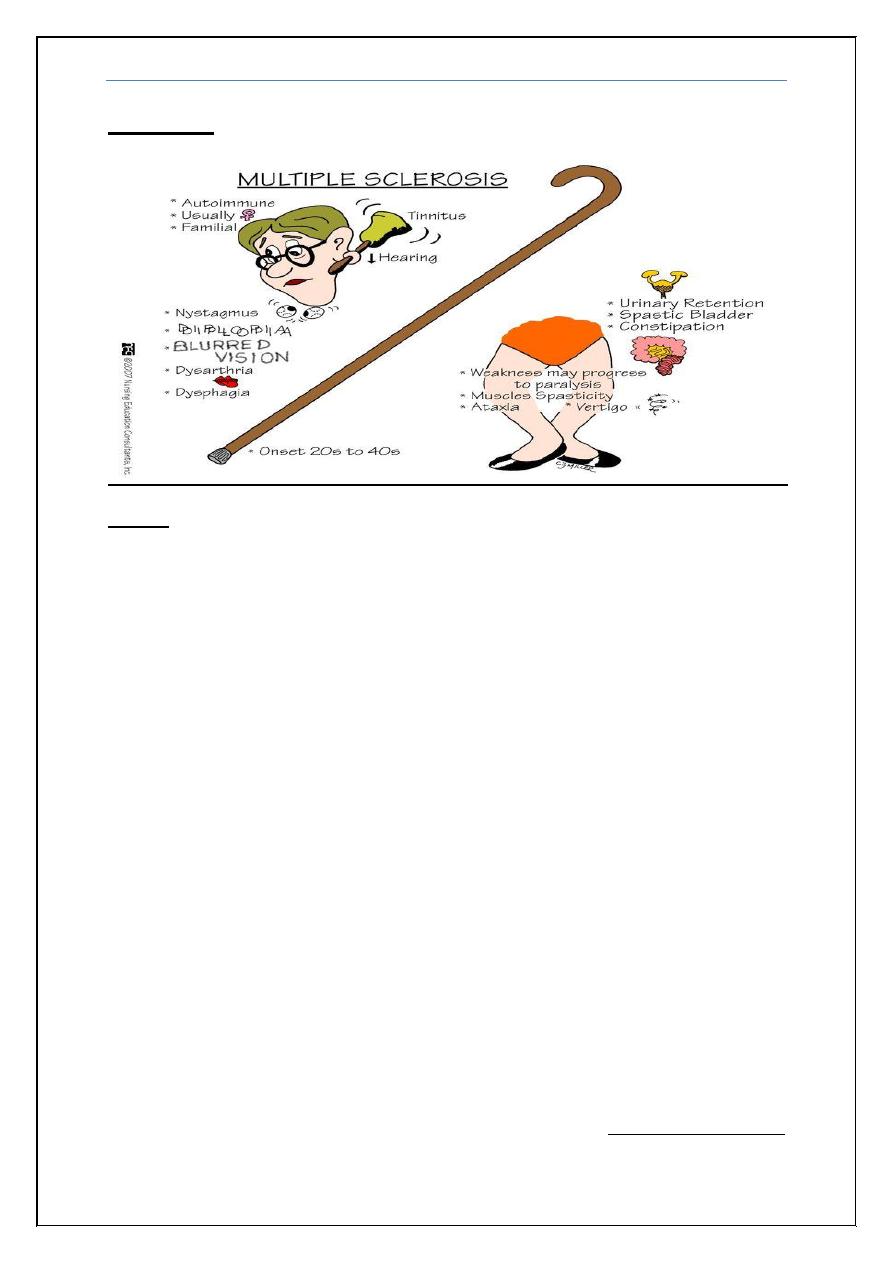
Signs and Symptoms:
Weakness 90%
Sensory disturbance
Ataxia
Bladder
Fatigue
Cramps
Diplopia
Visual loss 50%
Dysarthria 30%
Vertigo
Psychatric symptoms
Dysphagia
Loss of consciousness
Loss of taste 6%
Sensory disturbances
Ascending numbness starting in feet
Bilateral hand numbness
Hemiparesthesia / dysesthesia
Generalized heat intolerance
Dorsal column signs:
i.
Loss of vibration/proprioception
ii.
Lhermitte’s sign
Visual disturbances
Unilateral or bilateral partial/complete intranuclear ophthalmoplegia
CN VI paresis
Optic neuritis
- Central scotoma, headache, change in color perception, retroorbital
pain with eye movement)
Mentioned by Dr. Akram
Internuclear ophthalmoplegia: a
disorder caused by injury or dysfunction in the medial
longitudinal fasciculus (MLF) which connects the 6
th
cranial nerve with 3
rd
cranial nerve. It is a
disorde
r of conjugate lateral gaze in which the affected eye shows impairment of
adduction. When an attempt is made to gaze contralaterally (relative to the affected
eye), the affected eye adducts minimally, if at all. The contralateral eye abducts,
however with nystagmus. Additionally, the divergence of the eyes leads to horizontal
diplopia. If bilateral it is highly suggestive of MS if unilateral may be due to other
causes
Multiple Sclerosis Prof. Akram Al.Mahdawi
6
Motor disturbances
Weakness
Increased spasticity
Pathologic signs (Babinski, Hoffman)
Crebellar signs
Nystagmus
Dysarthria
Tremor
Dysmetria
Titubation
Stance and gait
Other clinical signs
Urinary incontinence, incomplete emptying
Cognitive and emotional abnormalities (depression, anxiety, emotional
labiality)
Fatigue
Sexual dysfunction
Differential diagnosis
Connective tissue diseases (SLE, Behcet and anti-phosphplipid
syndrome)
Primary CNS vasculitis
Postinfectious encephalomyelitis
Lyme disease
Behcet’s syndrome
Sarcoidosis / Sjogren’s disease
B12 deficiency / tertiary syphylis
Leukodystrophies
Multiple Sclerosis Prof. Akram Al.Mahdawi
7
Macdonald criteria
(No need to memorize it!)
Two or more relapses, objective clinical evidence of two or more lesions.
Two or more relapses, objective clinical evidence of one lesion (Need
dissemination in space)
One relapse, objective clinical evidence of two or more lesions
(dissemination in time).
Clinically Isolated Syndrome (CIS)
Exclude other structural disease and identify plaques of demylination
Demonstrate other site of involvement (MRI, VER).
Demonstrate inflammatory nature of lesions (CSF, cellcount, oligoclonal
bands)
Exclude other conditions (B12, CTS, CXR, ACE)
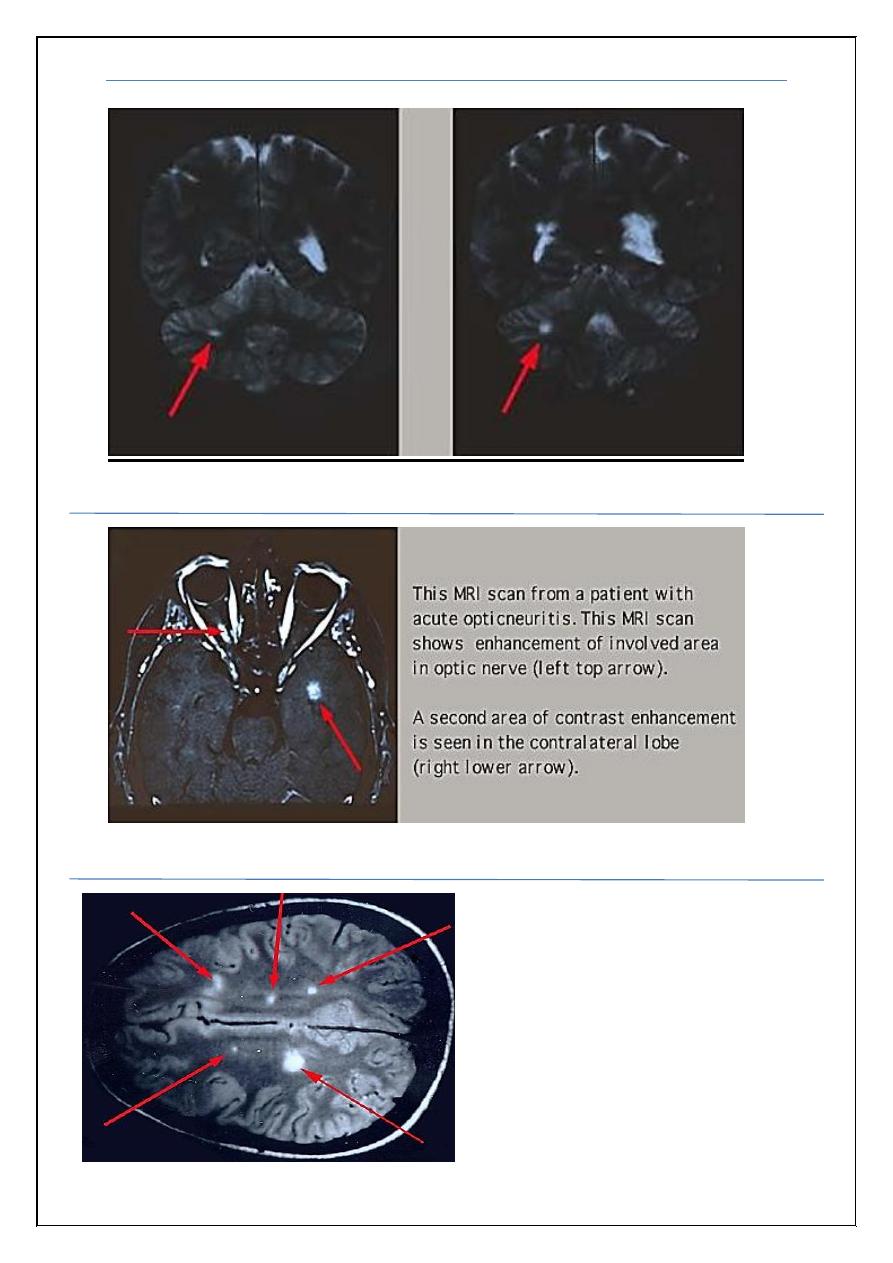
MRI findings:
Patchy areas of white matter in paraventricular cerebral areas
Lesions in cerebellum/brainstem/ cervical and thoracic spinal cord
Gadolinium enhancement identifies active lesions
**Caveat: **
Abnormal MRI without clinical evidence is not sufficient to confirm
the diagnosis of MRI.
Absence of abnormal MRI in clinically definite MS doesn’t disprove
diagnosis
Multiple Sclerosis Prof. Akram Al.Mahdawi
8
Fig (1): Abnormal MRI of the cerebellum
Fig (2):
Abnormal MRI of the optic nerve
Fig (3): Abnormal MRI of the
cerebral hemishperes
Multiple Sclerosis Prof. Akram Al.Mahdawi
9
Cerebro Spinal Fluid (CSF) findings
(Important!)
Increased immunoglobulin concentration in >90% of patients
IgG index (CSF/serum) elevated
Oligoclonal bands—85%
Elevated protein—50%
Modest increase in mononuclear cells
Evoked potentials
VER (visual evoked response)—75% abnormal regardless of optic
neuritis history
BAER (brainstem auditory evoked response)—30% abnormal
SSER (somatosensory evoked response) – 80% abnormal
- Helps distinguish peripheral from central lesions
Types of MS:
Relapse-remitting MS
(RRMS): Here you have an
attack, go into complete or
partial remission, and then
have the symptoms return.
Primary-progressive MS
(PPMS): Here you
continually decline and have
no remissions.
A few patients have malignant
MS which is where they have
a quick decline which leaves
them severely disabled or
even lead to death.
Secondary-progressive MS
(SPMS): This stage of MS
starts with RRMS symptoms
and continues on to show
signs of PPMS.
Progressive-relapsing MS
(PRMS): This is a rare form
but here it takes a progressive
route made worse by acute
attacks.
20% of the people with MS
have a benign form. Here
they show little progression
after the first attack.
Most
common
85%
Multiple Sclerosis Prof. Akram Al.Mahdawi
10
Favorable prognostic factors
(Important!)
Female gender
Low rate of relapses per year
Complete recovery from 1st attack
Long interval between 1st and 2nd attack
Younger age of onset
Later cerebellar involvement
Low disability 2-5 years from onset
Treatment of relapse attack
Methylprednisolone -500 to 1000 mg (1gm) /daily for 5 days.
PE, IV immune globulin for fulminate disease.
Interferon-beta -- Immune modulation -- widespread use for reducing
relapse rate (RCT evidence).
Glatiramer acetate --Immune modulation --Similar efficacy to interferon-
beta (RCT evidence).
Fingolimod --Immune modulation -- Superior efficacy to interferon-beta
in RCTs.
Monoclonal antibody to alpha4-integrin (natalizumab) --Immune
modulation. Possibly more effective than other drugs.
Teriflunomide (AUBAGO).
Dimethyl fumarate (Tecfidera ).
When Interferon beta therapy is initiated
Liver function tests and CBC at baseline.
Lab tests should then be repeated in 1, 3, 6 months during initiation of
therapy.
Monitoring can then be performed every 3 to 6 months thereafter.
Thyroid function tests are recommended in patients with history of
thyroid dysfunction every 6 months
Multiple Sclerosis Prof. Akram Al.Mahdawi
11
Adverse events
Inflammation at site of injection.
Headache, flu like symptoms (myalgia,fever, rigor, rhinitis and fatigue).
Rare side effects: Depression, suicide, epileptic events, Thyroid
abnormalities, lymphopenia, thrombocytopenia, asymptomatic elevated
liver transaminase levels and rarely symptomatic hepatitis
Symptomatic therapy
Spasticity: physiotherapy, baclofen, tizanidine, benzodiazepine, dantrolen
Botulinm toxin type A
Fatigue: amantadine,Modafinil,SSRIs
Depression: SSRIs, TAD (tricyclic anti-depressent)
Anxaiety: alprazolam
Ataxia: isoniazid,clonazepam
Dysthesia: carbamazepine,gabapentin
Paroxysmal disordersl: evetiracetam, carbamazepine
Trigeminal neuralgia: carbamazepine, levetiracetam
Tonic spasms: anticonvulsant,baclofen
Cerebellar dysfunction: levetiracetam, INH, carbamazepine
Breakthrough Relapsing
An increase in NO of relapses coupled with increase No of T2 hypertense
and or T1 enhancing lesion on MRI
Approach –Switch to another agent
Restoring conduction in area of demyelination
Dalfampridine (ampyria) is a broad- spectrum K channel blocker that increases
conduction of action potential in area of demyelination.
Counseling: provision of pre-conception counseling is best practice.
Relapse risk: endocrine effects on the immune system ensure that relapse
risk drops during pregnancy.
Multiple Sclerosis Prof. Akram Al.Mahdawi
12
Disease-modifying drugs: risk of teratogenicity means that all disease-
modifying drugs should ideally be stopped 6–8 wks before conception
and recommenced after.
Breastfeeding has stopped.
Post-partum relapse rate: rebound of immune system activity means that
the highest risk of relapse is in the first year after delivery.
Clinically isolated Syndrome (CIS)
An episode of symptoms of demylinating affecting the optic nerve, spinal
cord, brain stem in isolation.
85% of MS patients, onset is heralded by single episode.
Early treatment with interferon can delay progression to CDMS after CIS
presentation
Guidelines give beta interferon a level A recommendation for use in CIS.
Early initiation of treatment can delay progression to CDMS
MS & neuromyelitis optica (NMO)
The two conditions were long thought to represent variations of same disease.
Neuropathologic differences as well as the recent identification of an
autoantibody to the aquaporin-4 water channel (NMO-IgG) in patients
with NMO suggest is pathologically distinct from MS.
Acute bilateral optic neuritis should suggest the diagnosis of NMO.
The vision loss in NMO also tends to be more severe and recovery is less
complete than in MS.
Spinal cord lesion extending over at least three segment.
Absence of oligoclonal band in the CSF.
Strong association with other autoimmune disease.
Paucity or absence of brain lesions on MRI
Presence of NMO-IgG antibody
Multiple Sclerosis Prof. Akram Al.Mahdawi
13
Treatment of NMO
IV MP was associated at 6 months with a significantly faster recovery.
Short-term improvements with corticosteroid use have been demonstrated
in several studies.
IV MP is often given at a dose of 500mg to 1000 mg for 3 to 5 days,
sometimes followed by an oral prednisone taper for 10 to 14 days.
Other therapy includes plasma exchange and IVIG, Rituximab, anti-CD-
20 monoclonal antibody, azathioprin.
Acute disseminated encephalomyelopathy (ADEM):
Occurs in children and young adult
Typically follows febrile illness or vaccination
Low grade fever, headache and meningism followed by encephalopathy
Muti-focal deficit and seizure
Diagnosis depend on history, clinical findings, CSF, MRI (extensive,
large , multifocal lesion)
Usually monophasic illness, recovery occurs in 50-70%
Recurrent or multiphase occur in 20%
Neurological squeal in 1/3
Treatment, supportive, antiviral medication (because it looks like herpes
encephalitis), high dose IV MP followed by tapering oral steroid.
End
Multiple Sclerosis Prof. Akram Al.Mahdawi
14
Appendix (added by student not included in the lecture)
Case (1)
A 26-year-old white female presents with worsening weakness of her right upper
extremity, Left lower extremity and ataxia. She also complains of unilateral eye pain and
visual loss. The eye pain is worsened by ocular movements. On eye examination there is a
central visual field defect in her right eye. Fundoscopy is normal. Neurological
examination shows spastic paraparesis in the right upper extremity and the left lower
extremity. What is the most appropriate next step in this patient's management?
A. CT scan with contrast
B. MRI of the brain
C. Lumbar puncture
D. Brain biopsy
E. PET scan
Explanation:
The above patient is most likely suffering from multiple sclerosis (MS). Her history is
consistent with patchy neurological problems (e.g. right upper extremity, left lower extremity
and optic neuritis). Which is characteristic for MS. Optic neuritis presents as a painful loss of
vision and is an important presentation. Patients usually have a central visual field defect and
fundoscopy is normal. Sensory abnormalities may also occur.
MRI is the test of choice to support the clinical diagnosis of MS. It is also a better
predictor of evolution to clinically definite MS than other studies such as CT scan CSF
examination or evoked potentials. The characteristic MRI lesions are cerebral or cerebellar
plaques. The typical locations of the plaques are the periventricular regions, corpus callosum,
deep white matter and basal ganglia.
So the answer is B
Multiple Sclerosis Prof. Akram Al.Mahdawi
15
Case (2)
A 25-year-old woman comes to the office and complains of intermittent dizziness and an
unsteady gait for the last few days. Her symptoms worsen with exercise. Her past medical
history is significant for tingling and numbness of her right foot that lasted 3-4 days (1
year ago), and visual loss in her right eye which spontaneously resolved (3 years ago).
She is currently nursing her 2-month-old baby. Her obstetrical history was
uncomplicated. Her neurological examination shows right hyperactive deep tendon
reflexes.
On attempted left gaze, her left eye abducts and exhibits horizontal jerk
nystagmus, but her right eye remains stationary. When she attempts to look to the right,
her right eye abducts and exhibits horizontal jerk nystagmus, but her left eye remains
stationary
. The patient is able to converge both eyes together, without any associated
nystagmus. The facial muscles show no signs of weakness. Where is the most likely site of
this patient's lesion?
A. Optic nerve
B. Oculomotor nerve
C. Trochlear nerve
D. Abducent nerve
E. Medial longitudinal fasciculus
F. Medial lemniscus
Explanation:
Suspect multiple sclerosis in a patient with neurological deficits that cannot be explained by a
single lesion. Exacerbation of these neurological deficits by hot weather or exercise is a
useful clue. Complete internuclear ophthalmoplegia (excellently described in this patient's
current eye movement dysfunctions) is a characteristic finding, and is caused by
demyelination of the medial longitudinal fasciculus in the dorsal pontine tegument.
So the answer is E
Case (7)
A 36-year-old white female is brought to the emergency department due to paraplegia and
bladder incontinence. She immediately tells you that she has, "multiple sclerosis in
remission." She has a history of optic neuritis and internuclear ophthalmoplegia and both
resolved with treatment at that time MRI showed plaques in the periventricular region. She is
currently not taking any medications. Which of the following is the most appropriate next
step in the management of this patient?
A. Corticosteroids
B. Plasmapheresis
C. Interferon
D. Cyclophosphamide
E. Intravenous Immunoglobulins
F. Glatiramer acetate
Multiple Sclerosis Prof. Akram Al.Mahdawi
16
Explanation:
Acute exacerbations of multiple sclerosis are generally treated with IV steroids. Steroids are
the most widely used drugs in the treatment of acute exacerbations because these can hasten
the recovery of such patients. A high-dose intravenous steroid (i.e. methylprednisone) is used
when patients present with disabling symptoms. Mild sensory symptoms generally do not
require steroids. Long-term steroid therapy provides no benefit, and does not prevent future
relapses. To reduce the frequency of acute exacerbations interferon, plasmapheresis,
cyclophosphamide, intravenous immunoglobulins and glatiramer acetate may be used.
So the answer is A
For those who are interested to read more clinical cases please see the
uploaded file on
