multiple sclerosis
Case (1)
A 26-year-old white female presents with worsening weakness of her right upper extremity,
Left lower extremity and ataxia. She also complains of unilateral eye pain and visual loss.
The eye pain is worsened by ocular movements. On eye examination there is a central visual
field defect in her right eye. Fundoscopy is normal. Neurological examination shows spastic
paraparesis in the right upper extremity and the left lower extremity. What is the most
appropriate next step in this patient's management?
A. CT scan with contrast
B. MRI of the brain
C. Lumbar puncture
D. Brain biopsy
E. PET scan
Explanation:
The above patient is most likely suffering from multiple sclerosis (MS). Her history is consistent
with patchy neurological problems (e.g. right upper extremity, left lower extremity and optic
neuritis). Which is characteristic for MS. Optic neuritis presents as a painful loss of vision and is
an important presentation. Patients usually have a central visual field defect and fundoscopy is
normal. Sensory abnormalities may also occur.
MRI is the test of choice to support the clinical diagnosis of MS. It is also a better predictor of
evolution to clinically definite MS than other studies such as CT scan CSF examination or
evoked potentials. The characteristic MRI lesions are cerebral or cerebellar plaques. The typical
locations of the plaques are the periventricular regions, corpus callosum, deep white matter and
basal ganglia.
Case (2)
A 29-year-old female is brought to the emergency department due to paraplegia, urinary
incontinence and urgency. She denies any trauma. She has a history of trigeminal neuralgia. The
neurological examination shows spasticity and hyperreflexia in the lower extremities and
impaired vibration and proprioception in her left forearm. Which of the following is the most
likely finding in this patient's cerebrospinal fluid (CSF) examination?
A. Oligoclonal bands
B. Albumino-cytologic dissociation
C. Increased pressure
D. Increased cell count
E. Increased total protein concentration
Explanation:
This patient most likely has multiple sclerosis (MS). The total protein concentration in such
patients is usually normal; however, immunoglobulin levels are high relative to other protein
components. The predominant immunoglobulin type is lgG although lgM and lgA are also
increased. The lgG index is used to measure the increase in lgG levels relative to other proteins.
lgG index is elevated in 90% of patients with MS; however the false positive rate is high (8%).
Furthermore elevated immunoglobulin levels may be found in other diseases such as
neuropathies chronic central nervous system infections or viral syndromes. For these reasons the
presence of oligoclonal bands is not considered diagnostic for MS.
Case (3)
A 27-year-old Caucasian female with multiple sclerosis (MS) comes to the office for a follow-up
visit. Six months ago she experienced monocular vision impairment and clumsiness of the
right hand and both symptoms resolved completely. Three weeks ago she experienced
incoordination, weakness and spasticity in the right extremities. She was admitted in the
hospital for treatment of an acute MS flare and rapidly improved thereafter. Physical
examination currently demonstrates slight weakness of the right leg with a hyperactive knee jerk.
Which of the following medications may slow the long-term progression of this patient's
disease?
A. High-dose corticosteroids
B. lnterieron-beta
C. Cyclosporine
D. Methotrexate
E. Mitoxantrone
Explanation:
This patient has the relapsing-remitting form of multiple sclerosis (MS). which is characterized
by well-defined acute episodes with no significant disease progression between the episodes.
Several well-designed clinical trials have proven that interieron-beta decreases the frequency of
relapse and reduces disability in patients with the relapsing-remitting form of MS.
Case (4)
A 25-year-old woman comes to the office and complains of intermittent dizziness and an
unsteady gait for the last few days. Her symptoms worsen with exercise. Her past medical
history is significant for tingling and numbness of her right foot that lasted 3-4 days (1 year
ago), and visual loss in her right eye which spontaneously resolved (3 years ago). She is
currently nursing her 2-month-old baby. Her obstetrical history was uncomplicated. Her
neurological examination shows right hyperactive deep tendon reflexes.
On attempted left
gaze, her left eye abducts and exhibits horizontal jerk nystagmus, but her right eye remains
stationary. When she attempts to look to the right, her right eye abducts and exhibits
horizontal jerk nystagmus, but her left eye remains stationary
. The patient is able to
converge both eyes together, without any associated nystagmus. The facial muscles show no
signs of weakness. Where is the most likely site of this patient's lesion?
A. Optic nerve
B. Oculomotor nerve
C. Trochlear nerve
D. Abducent nerve
E. Medial longitudinal fasciculus
F. Medial lemniscus
Explanation:
Suspect multiple sclerosis in a patient with neurological deficits that cannot be explained by a
single lesion. Exacerbation of these neurological deficits by hot weather or exercise is a useful
clue. Complete internuclear ophthalmoplegia (excellently described in this patient's current eye
movement dysfunctions) is a characteristic finding, and is caused by demyelination of the medial
longitudinal fasciculus in the dorsal pontine tegument.
Case (5)
A 32-year-old female is brought to the clinic by her husband because he believes she is a
malingerer and is "just being difficult." Sometimes, she appears confused and disoriented. Over
the past year, she has complained of visual loss, eye pain and inability to do any household
chores. Two months ago, she claimed to have lost control of her bladder. Interestingly, she is
"her normal self" when it is time to go for summer trips. The wife insists that she does not
understand what is happening to her, and adds that she occasionally loses the ability to move her
right hand. The physical examination is basically normal. The patient appears, alert, oriented,
and is in no distress. Which of the following is the most appropriate next step in management?
A. MRI of the brain
B. Lumbar puncture
C. Tonometry
D. Serum immunoglobulins
E. Nerve conduction studies
F. Refer to psychiatry
Explanation:
Suspect multiple sclerosis (MS) in a female who has recurrent attacks of focal neurologic
dysfunction that occur at non-predictable time intervals. The age of onset is usually between the
third and the fourth decade. The pathology involves demyelination of focal regions in the white
matter of the brain, with a propensity to involve the periventricular and subpial white matter of
the cerebrum, the optic nerves, brain stem and spinal cord. The MRI is the diagnostic test of
choice for identifying demyelinating lesions. Visual, auditory and somatosensory evoked
response tests are of value in identifying silent lesions.
Case (6)
A 33-year-old white female presents to the office with severe. bilateral, lightning-like pain on
her face. The pain is burning and sharp in nature, occurs 20-30 times a day, and each
episode lasts a few seconds. She is completely incapacitated by this pain. Prior to this event, she
had weakness in her left arm which gradually improved. She denies any history of trauma or
drug use. She has no other medical problems. She does not use tobacco, alcohol or drugs. Her
blood pressure is 118/81 mmHg, pulse is 72/min, temperature is 36’7C (98F) and respirations are
14/min. Complete neurologic examination shows no focal deficits. This type of disorder is most
commonly seen in which of the following?
A. Parkinson disease
B. Huntington chorea
C. Multiple sclerosis
D. Aseptic meningitis
E. Transient ischemic attack
Explanation:
The history and presentation of this patient is characteristic for multiple sclerosis (MS). MS
usually presents during the third or the fourth decade with recurrent focal neurologic
dysfunction. The attacks are non-predictable and erratic in presentation. The symptoms may last
a few weeks with variable recovery. MS is one of the few conditions that may present with
bilateral trigeminal neuralgia. Another clue is the presentation of transient left arm weakness.
Case (7)
A 36-year-old white female is brought to the emergency department due to paraplegia and
bladder incontinence. She immediately tells you that she has, "multiple sclerosis in
remission." She has a history of optic neuritis and internuclear ophthalmoplegia and both
resolved with treatment at that time MRI showed plaques in the periventricular region. She is
currently not taking any medications. Which of the following is the most appropriate next step in
the management of this patient?
A. Corticosteroids
B. Plasmapheresis
C. Interferon
D. Cyclophosphamide
E. Intravenous Immunoglobulins
F. Glatiramer acetate
Explanation:
Acute exacerbations of multiple sclerosis are generally treated with IV steroids. Steroids are the
most widely used drugs in the treatment of acute exacerbations because these can hasten the
recovery of such patients. A high-dose intravenous steroid (i.e. methylprednisone) is used when
patients present with disabling symptoms. Mild sensory symptoms generally do not require
steroids. Long-term steroid therapy provides no benefit, and does not prevent future relapses. To
reduce the frequency of acute exacerbations interferon, plasmapheresis, cyclophosphamide,
intravenous immunoglobulins and glatiramer acetate may be used.
Long case
A 31-year-old woman is referred to a neurologist for evaluation of multiple neurologic complaints. She
recalls a specific episode 3 years ago of mild weakness in her right leg, which seemed to resolve over
time. Last month, she developed incoordination of her left leg and left hand, although these too seem to
be improving. She feels that she has also become less steady on her feet over time. Though she always
considered herself to be an energetic person, over the past year or two she has been constantly
fatigued. She has also been having problems focusing her attention and feels that her thinking has
slowed down in general. She has noticed that many of her symptoms sometimes get worse after a hot
bath or after she has been to the gym. The patient recently was sick with the fl u and is now suffering
from a particularly bad flare of her symptoms. Although her fl u symptoms have subsided, she is
concerned by the fact that 2 days following the onset of her fl u she developed blurry vision in the right
eye and pain in the eye associated with eye movements. On examination the patient is found to be
afebrile and has normal vital signs. Her visual acuity in the right eye is 20/80 compared to 20/20 in the
left eye. WBC count, erythrocyte sedimentation rate, and C-reactive protein are all normal.
Cerebrospinal fluid analysis reveals slightly elevated protein, with elevated immunoglobulin G and
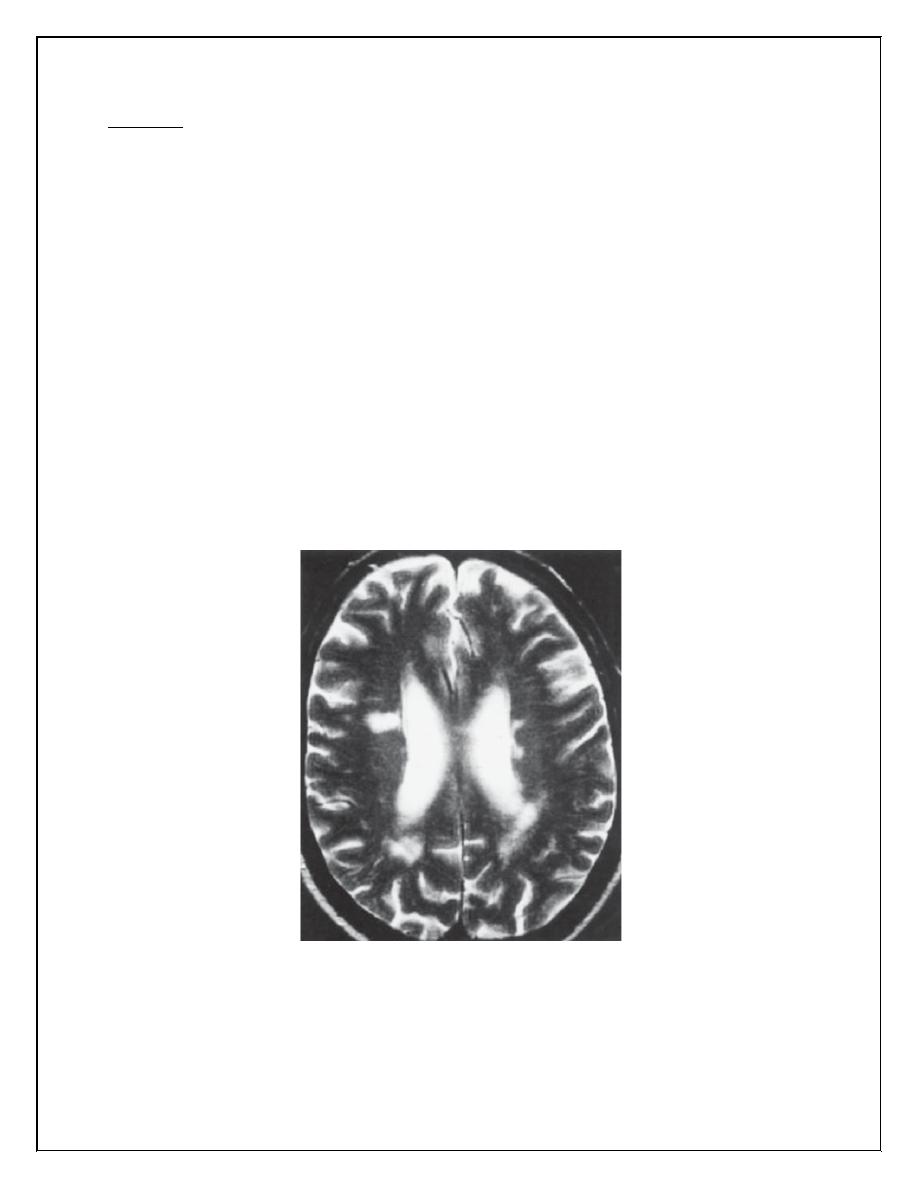
oligoclonal bands on further analysis. MRI of the brain is shown in Figure below.
� What is the most likely diagnosis?
Multiple sclerosis (MS), MS is an idiopathic inflammatory demyelinating disease of the central nervous
system. This disease more frequently affects women of northern European descent who are of
childbearing age. As seen in Figure 10-2, MS is characterized pathologically by multifocal areas of
demyelination (often periventricular) with relative preservation of axons, loss of oligodendrocytes, and
astroglial scarring. MS has a highly variable presentation and remains a clinical diagnosis made by the
combination of history and physical and laboratory and radiological examinations. MS is an autoimmune
disease of unclear etiology (it is thought that stimulation of the immune system by a viral infection may
trigger the disease). Typical presenting features include optic neuritis, internuclear ophthalmoplegia,
Lhermitte's phenomenon (electric shock–like sensations radiating down the spine or into the limbs with
fl exion of the neck), nystagmus, and pain. Psychiatric symptoms are not uncommon.
� What conditions should be included in the differential diagnosis?
The differential diagnosis is limited in a young patient who presents with a history of two or more
clinically distinct episodes of CNS dysfunction with at least partial resolution. This diagnosis becomes
diffi cult when a patient presents with atypical symptoms. In general, the differential includes infl
ammatory diseases (acute disseminated encephalomyelitis, polyarteritis nodosa, lupus), infectious
diseases (HIV, neurosyphilis, Lyme disease), granulomatous disease (sarcoidosis, Wegener's
granulomatosis), other primary myelin diseases (e.g., adrenoleukodystrophy), and others such as
Arnold-Chiari malformation, vitamin B12 defi ciency, and arteriovenous malformation.
� What criteria are used to diagnose this condition?
The McDonald criteria are now the most commonly used for diagnosing MS (see Table 10-1) and are
based on both clinical and MRI fi ndings.
� What is the most appropriate treatment for this condition?
IV steroids have been shown to reduce the duration and severity of an acute fl are, but probably do not
change overall disease progression. Specifi c immunomodulatory agents used to treat MS include:
interferon β1a (Avonex and Rebif), interferon β1b (Betaseron), glatiramer acetate (Copaxone), and
mitoxantrone (Novantrone). Since the course is typically progressive, symptomatic therapy for
depression, spasticity, urinary incontinence/retention is imperative.
