Congenital Anomalies of CNS
د .اثل اطفال مرحله خامسهCongenital Anomalies of CNS
NTD
Microcephaly
Macrocephaly
Neural Tube Defects ( Dysraphism )
Neural tube defects (NTDs) account for most congenital anomalies of the central nervous system (CNS) and result from failure of the neural tube to close spontaneously between the 3rd and 4th wk of in utero development.Although the precise cause of neural tube defects remains unknown, evidence suggests that many factors may adversely affect normal development of the CNS from the time of conception, these include:
Hyperthermia
Drugs
Chemicals
Malnutrition
Maternal obesity or diabetes
Genetic determinants (mutations in folate-responsive or folate-dependent pathways)
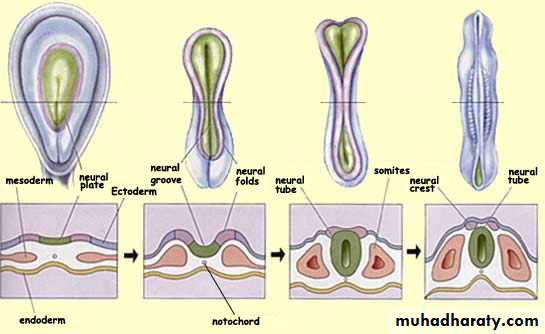
Neural tube development
Neural tube defects
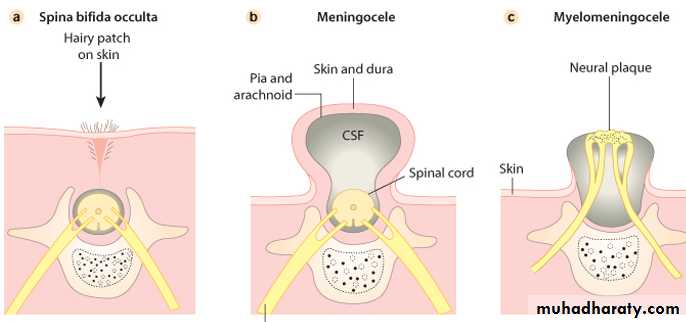
Spina Bifida Occulta :
This common anomaly consists of a midline defect of the vertebral bodies without protrusion of the spinal cord or meninges.Most individuals are asymptomatic and lack neurologic signs, and the condition is usually of no consequence.
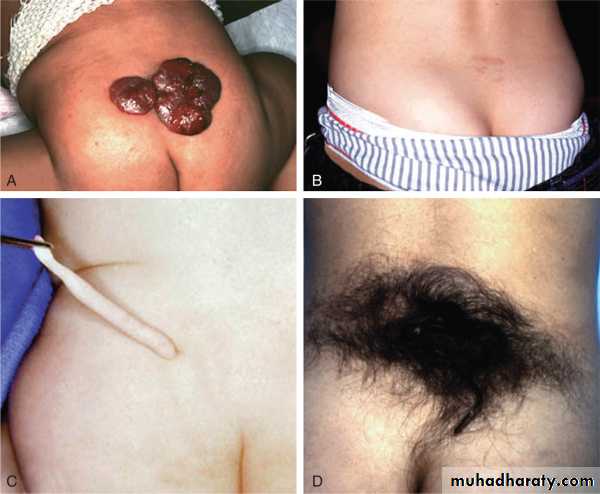
In some cases, patches of hair, a lipoma, discoloration of the skin, or a dermal sinus in the midline of the lower back suggests a more significant malformation of the spinal cord.
Meningocele
A meningocele is formed when the meninges herniate through a defect in the posterior vertebral arches. The spinal cord is usually normal and assumes a normal position in the spinal canal.A fluctuant midline mass that may transilluminate occurs along the vertebral column, usually in the lower back.
An anterior meningocele projects into the pelvis through a defect in the sacrum. Symptoms of constipation and bladder dysfunction develop due to the increasing size of the lesion. Female patients may have associated anomalies of the genital tract.
A CT scan of the head is recommended for children with a meningocele because of the association with hydrocephalus in some cases.
Plain roentgenograms demonstrate a defect in the vertebra, and CT scanning or MRI outlines the extent of the meningocele.
Most meningoceles are well covered with skin and pose no threat to the patient.
Careful neurologic examination is mandatory. Asymptomatic children with normal neurologic findings and full-thickness skin covering the meningocele may have surgery delayed. Those patients with leaking cerebrospinal fluid (CSF) or a thin skin covering should undergo immediate surgical treatment to prevent meningitis.
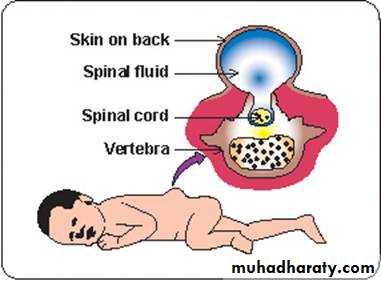
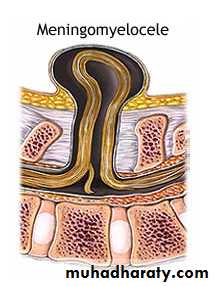
Myelomeningocele
It is a spinal meningocele that contains nerve roots & some times spinal cord tissue & is always associated with mid line defects of the vertebral neural arches, muscle, subcutaneous connective tissues & skin.This condition produces dysfunction of many organs and structures, including the skeleton, skin, GIT & GUT, in addition to the peripheral nervous system and the CNS.
Prevention: folic acid daily
Figure : A lumbar myelomeningocele is covered by a thin layer of skin.
Myelomeningocele showing the exposed neural tissue and the patulous anus from neuropathic bowel.
Encephalocele
cranial encephalocele contains the meningeal sac plus cerebral cortex, cerebellum, or portions of the brainstem. The cranial defect occurs most commonly in the occipital region, frontal or nasofrontal encephaloceles may occur.Infants with a cranial encephalocele are at increased risk for developing hydrocephalus
Anencephaly
This is failure of development of most of the cranium and brain.Affected infants are stillborn or die shortly after birth.
It is detected on antenatal ultrasound screening and termination of
pregnancy is usually performed.
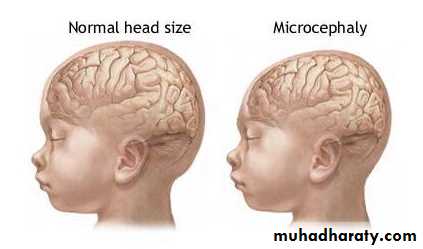
Microcephaly ( small head )
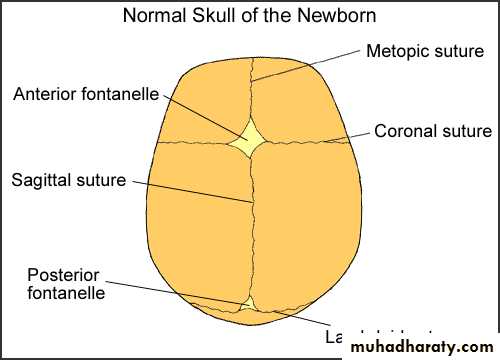
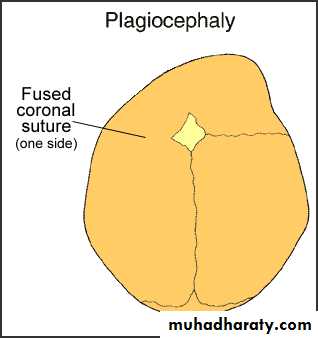
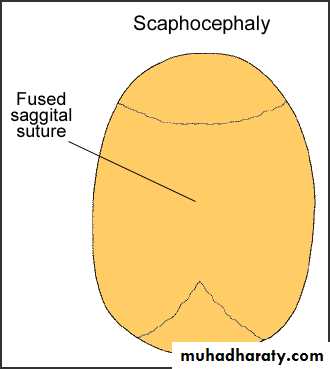
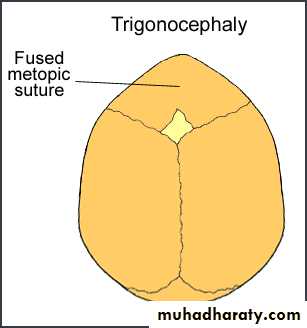
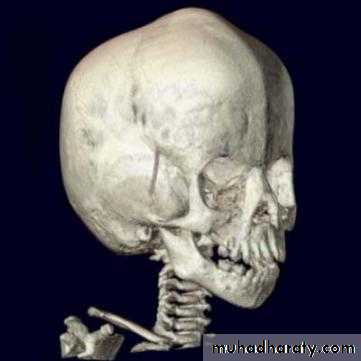
Crainocynostenosis: is defined as premature closure of the cranial sutures and is classified as primary or secondary.Primary craniosynostosis refers to closure of one or more sutures due to abnormalities of skull development. The cause is unknown in the majority of children ,however, genetic syndromes account for 10–20% of cases.
secondary craniosynostosis results from failure of brain growth and expansion.
Small brain
Etiology of small brain:
PRIMARY (GENETIC) :Autosomal recessive
Autosomal dominant
Syndromes : Down (21-trisomy), Edward (18-trisomy), (13-trisomy).
2. SECONDARY (NONGENETIC) :
RadiationCongenital infections (TORCHS)
Drugs :Fetal alcohol
Meningitis/encephalitis
Malnutrition
Metabolic
Hyperthermia
Hypoxic-ischemic encephalopathy
Macrocephaly ( large head )
1- Macrocrania (increased skull thickness) :Ricket
Osteogenesis imperfecta
Hypertrophy of BM resulting from hemolytic anaemia.
2- Megalencephaly ( enlargment of the brain) :
Abnormal proliferation of the brain tissue such as NF & TS.
Accumulation of abnormal metabolic substances as seen in Tay-Sachs & mucopolysaccharidoses.
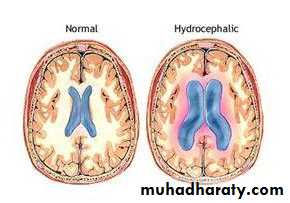
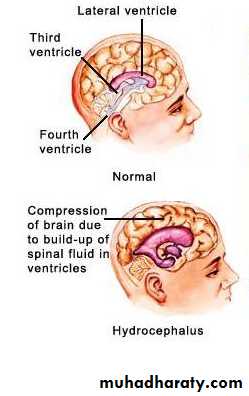
3- Hydrocephalus( enlargement of the ventricles)
Hydrocephalus
Produces slowly evolving syndrome of ↑ICP extending over wks or ms.
Pressure is exerted by both enlarging ventricle & interstitial edema in the periventricular white matter created by transudation of CSF through the ependymal barrier.
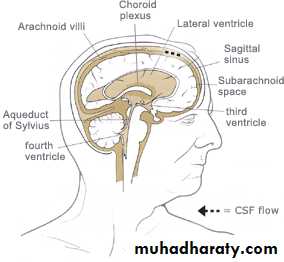
CSF:
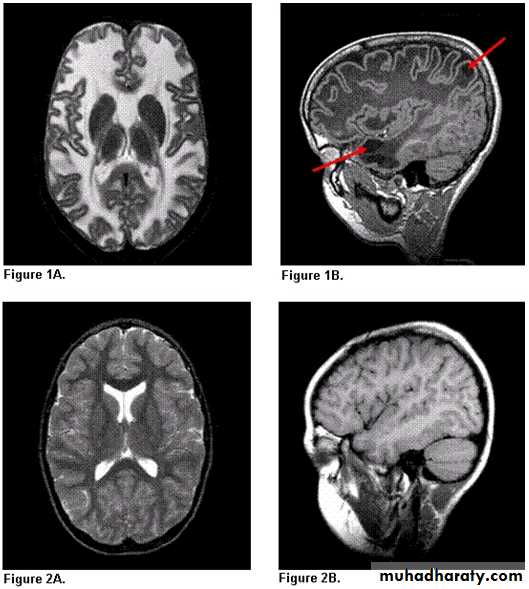
Ultra filtration of plasma produced by choroids' plexus. Volume 50 ml in neonate ,150 ml in adultFlow from lateral v →3rd V through foramen of Monro then through cerebral aqueduct →4th V then through foramen of Magendie and Luschka to the subarachnoid space.
Absorption: by arachnoid villi.
Types of hydrocephalus
Obstructive non obstructive over production of csfObstructive
EtiologyCongenital, IV tumors, mass
NF, IU toxo, postmumps meningoencephalitis, mass, tumors, malformation, congenital dysplasia
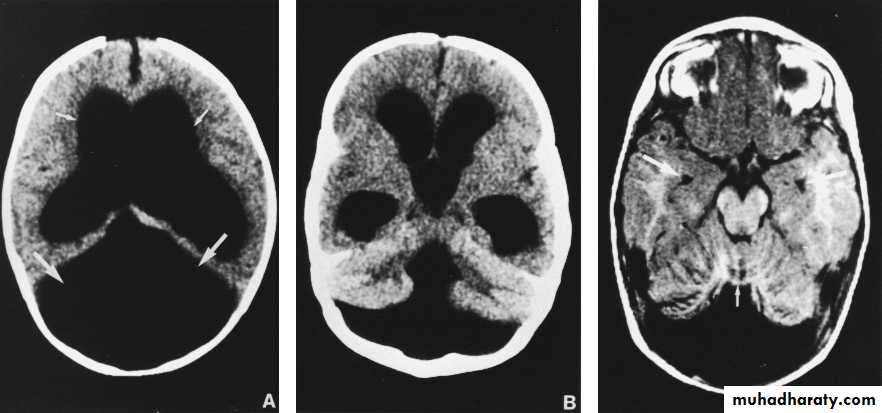
Agenesis of cerebellar vermis & cystic dilation of 4th ventricle.
Congenital small post fossa with caudal displacement of 4th ventricle & cerebellum & distortion of the brainstemRickets, achondroplasia
Non obstructive (extraventricular obstruction, communicating) :1- congenital hypoplasia of arachnoid villi.
2- infection: IU inf, pneumococcal & TB meningitis.
3- leukaemic infilteration
4- hemorrhage
Overproduction of CSF:
Colloid plexus papillomas, which manifist early in infancy.Diagnosis:
Hx:F.Hx. Suggest x- linked aqueduct stenosis.
Past hx of prematurity suggest ICH.
Meningitis, mumps encephalitis.
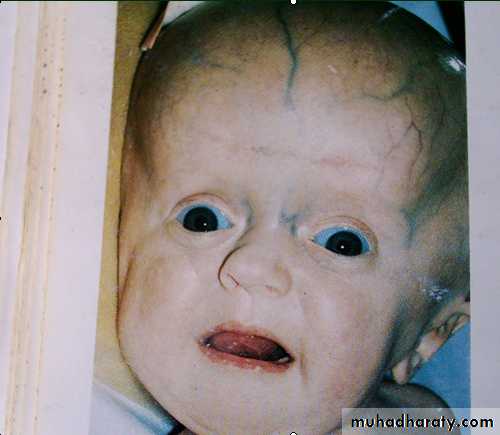
Clinical feature:
Symptoms & signs of ↑ICP ( may evolve slowly or rapidly)
Rapid ↑in OFC by serial measures.
widely opening fontanel.
Broad forehead.
Ataxia & spasticity
Endocrine dysfunction
Visual dysfunction
Sun set eyes
Dilated scalp veins.
Gradual change in personality & deterioration in academic productivity suggest slowly progressive hydrocephalus
Examination:
inspection, palpation & auskultation of the skull & spine.
OFC measurement
Ant fontanel size & shape
Inspection of the back for midline lesion; hair, lipoma…
Prominent forehead or abnormal occiput shape.
Cranial bruit; AVM
Transullimation of the skull +ve; Dandy walker.
Inspection of eye ground; chorioretinitis suggest IU infection as toxoplasmosis.
INV:
Skull X-ray:Seperation of sutures
Errosion of posterior clinoid
CT/MRI/US: Dx specific Cause.
Dandy-walker
Treatment:
Medical :(Meningitis, SAH)
Acetazolamide; decrease CSF production
Surgery :
Removal of cyst ,tumor & AVMshunt placing.