ISHIK UNIVERSITYFACULTY OF DENTISTRY
Pharmacology2015-2016
1
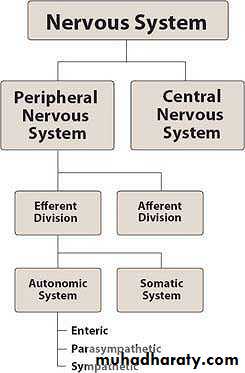
The nervous system is divided into two anatomical divisions: the central nervous system (CNS), which is composed of
the brain and spinal cord, and the peripheral nervous system, which includes neurons located outside the brain and spinal cord that is, any nerves that enter or leave the CNS.
The peripheral nervous system is subdivided into the efferent division, the neurons of which carry signals away from the brain and spinal cord to the peripheral tissues, and the afferent division, the neurons of which bring information from the periphery to the CNS.
Afferent neurons provide sensory input to modulate the function of the efferent division through reflex arcs, that is, neural pathways that mediate a reflex action.
Brain & Spinal cord
Carry impulses from CNS to PNS
Carry impulses from PT to CNS
Drugs Affecting Autoimmune System
EfferentAutonomic N.S. : Function involuntarly to control the body needs and requirements without the concious participationsof the mind ? HR, cardiac contraction, exocrene gland.
Somatic N.S. : Under voluntary control, and it controls skeletal muscle contraction.
The efferent somatic nervous system differs from the autonomic system in that a single myelinated motor neuron,originating in the CNS, travels directly to skeletal muscle without the mediation of ganglia.
Drugs Affecting Autoimmune System
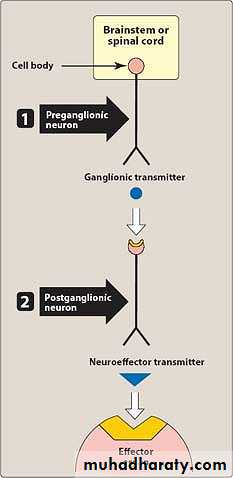
In A.N.S. the nerve impulses are carried by the way of two neurons
1. It is cell body located CNS and makes connection with a second neuron in an area called as ganglion.
2. A.N.S. innervates cardiac muscle; exocrine gland and vascular and non-vascular smooth muscle. The nerve impulse is carried along pre-ganglion an post-ganglion by a process called conduction.
While the nerve impulse carried in ganglion and neuroeffective junction release of neurotransmitters.
Drugs Affecting Autoimmune System
The two Neurotransmitters :1. Acetylcholine
2. Noradrenaline (Norepinephrine)
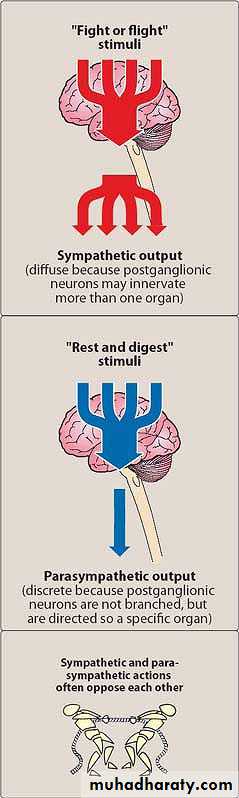
ANS is divided functionlly to :
1. Sympathetic ( dominant in fight, flight, fright), (response to emergencies)
2. Parasympathetic (becomes dominant at rest (secondary cases))
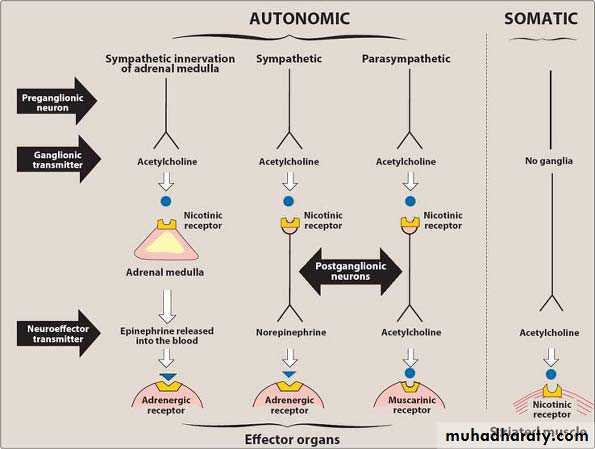
neurotransmitters released and the types of receptors found within the autonomic and somatic nervous systems
Function of Acetylcholine as Neurotransmitter
Acetylcholine is a neurotransmitter at both sympathetic and parasympathetic preganglionic nerve ending.Ach is Neurotransmitter at all parasympathetic postganglionic nerve ending.
It is a Neurotransmitter at sympathetic postganglionic nerve ending, supplying sweating, vasodilatory blood vessels of skeletal muscle.
It is neurotransmitter at neuromuscular junction.
A neurotransmitter at adrenal medula inervated by preganglionic sympathetic NS.
Noradrenaline
Noradrenaline is a neurotransmitter at all sympathetic postganglionic nerve ending except sweating and vasodilatory blood vessel of skeletal muscle.Neurotransmitters (Ach & noradrenaline) exert their effect through interacting with their specific receptors.
Receptors of Ach called colinergic receptor
Types of Cholinergic Receptors :
1. Muscarinic receptor (located on post-synaptic of effector organs such as cardiac muscle, smooth muscle & exocrine muscle)M1, M2, M3, M4, M5 : are types of muscarinic receptor.
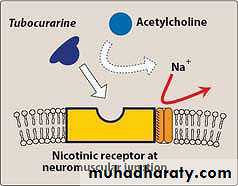
2. Nicotinic receptor (located in the ganglion in the adrenal medula & at skeletal muscle)
Ganglionic blockers specifically act on the nicotinic receptors of both parasympathetic and sympathetic autonomic ganglia
Nicotinic reseptor at ganglion & skeletal muscle are not identical.
Nicotinic receptor at ganglion is blocked by Hexamethonium and is blocked at skeletal muscle by tubocurarine.
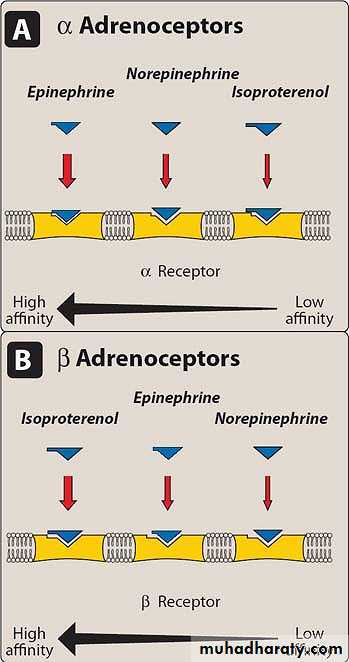
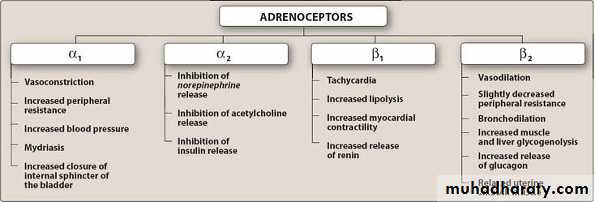
There are 2 types of Adrenal receptor:
1) α α1 and α2Generally stimulation of α receptor is associated with excitation except in GIT
α 1 receptor located post-synaptically on vascular and non-vascular smooth muscle and on exocrine gland .
α2 receptor : mainly located presynaptically stimulation of α2 receptor is associated with inhibition of sympathetic outflow.
Inhibition of α2 receptor is associated with stimulation of sympathetic outflow.
α α1
α2 α2Aα2B
2) β- receptor is 3 types: β1, β2, β3
Generally β-receptor stimulation is associated with inhibition except in heart also in adipose tissue.
β1 present in heart
β2 present in vascular smooth muscle and in exocrine gland.
β3 stimulation is associated with glycolysis (a process in which TG is hydrolysed to free fatty acid & glycerol)
Agonist
Antagonistα1 receptor
Phenylephrine
Prazosine
• α2 receptor
Clonidine
Yohimbine
β1 receptor
Dobutamine
Misoprolol
β2 receptor
Salbutamol
Butoxamine
Adrenergic Receptors
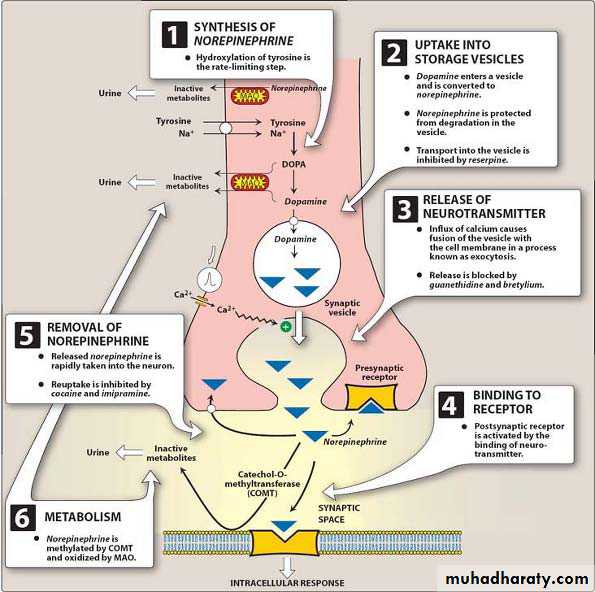
Synthesis and release of norepinephrine from the adrenergic neuron. (MAO = monoamine
oxidase.).Biosynthesis of Noradrenaline
Norepinephrine is synthesized from the amino acid tyrosine by a series of enzymatic steps in the adrenal medulla and postganglionic neurons of the sympathetic nervous system. While the conversion of tyrosine to dopamine occurs predominantly in the cytoplasm, the conversion of dopamine to norepinephrine by dopamine β-monooxygenase occurs predominantly inside neurotransmitter vesicles.
Thus the direct precursor of norepinephrine is dopamine, which is synthesized indirectly from the essential amino acid phenylalanine or the non-essential amino acid tyrosine
Phenylalanine is converted into tyrosine by the enzyme phenylalanine hydroxylase, with molecular oxygen (O2) and tetrahydrobiopterin as cofactors. Tyrosine is converted into L-DOPA by the enzyme tyrosine hydroxylase, with tetrahydrobiopterin, O2, and probably ferrous iron (Fe2+) as cofactors. L-DOPA is converted into dopamine by the enzyme aromatic L-amino acid decarboxylase (also known as DOPA decarboxylase), with pyridoxal phosphate as cofactor. Dopamine is then converted into norepinephrine by the enzyme dopamine β-monooxygenase (formerly known as dopamine β-hydroxylase), with O2 and ascorbic acid as cofactors.
Norepinephrine itself can further be converted into epinephrine by the enzyme phenylethanolamine N-methyltransferase with S-adenosyl-L-methionine as cofactor
The released NA either interact with Adrenergic receptor or metabolised by MAO enzyme or COMT(catechol-O-methyltransferase) in the circulation.
Or re-enters into the varicosities and enter the vesicles.
The release of NA from adrenergic neuron is inhibited by Guanithidine (Anti-HTN drug).
COMT inhibitor : Tolcapon inhibits destruction of NA by COMT. This drug used for Parkinsonism.
MAO inhibitor : chlogylline used for depression because it inhibits destruction of seratonine and NA.
Major Effects Mediated by Adrenoreceptors
DRUGS ACTING ON CNSSympathomimetics/ Adrenergic drugs
Sympathomimetics (Adrenergic drugs) : They facilitate or mimic some or all of the action of sympathetic N.S.They are divided according to their action into 3 :
1. Direct acting: are drugs which produce action by stimulating adrenergic receptors
2. Indirect acting: act by promoting the release of NA from adrenergic neuron (drugs that facilitate NA release, drugs that block NA uptake TSA inhibit NA reuptake to adrenergic neuron)
Mixed acting: are drugs which produce action by stimulating adrenergic receptors & by promoting release of NA from adrenergic neuron.
Sympathomimetics/AdrenomimeticsTherapeutic Agents
Direct actionAlpha and Beta Agonist
Indirect action
Amphetamine
Cocaine
Tyramine
Mixed action
Ephedrine
Pseudoephedrine
OXYMETAZOLINE
It is a directly acting sympathomimetic amine used in symptomatic relief in nasal congestion which increases mucosal secretion.It is used:
• As a nasal decongestant in allergic rhinitis, with or without the addition of antazoline or sodium chromoglycate.
• As a nasal decongestant in sinusitis, in otitis media where there is evidence of obstruction of the eustachian tube especially in subacute serous otitis media and otitic barotrauma.
• As an ocular decongestant in allergic conjunctivitis.
• To ‘whiten’ an inflamed (red) eye caused by a local irritant such as dust or following the removal of a foreign body.
Ephedrine
Ephedrine is useful for the treatment of chronic and moderate type of bronchial asthma, used as nasal decongestant and as a mydriatic without cycloplegia.
It act indirectly and directly on α and β receptors. It increases blood pressure both by peripheral vasoconstriction and by increasing the cardiac output. Ephedrine also relaxes the bronchial smooth muscles.
Pseudoephedrine
It is used as a nasal/sinus decongestant and stimulant or as a wakefulness-promoting agent.The salts pseudoephedrine hydrochloride and pseudoephedrine sulfate are found in many over-the-counter products either as a single ingredient or in combination
with NSAIDs (e.g., aspirin, ibuprofen, etc.).
Amphetamine
It is a psycho-stimulant: To Enhance PerformanceIt is a synthetic compound with structural similarity to ephedrine. It increases the systolic and diastolic blood pressure.
Produces wakefulness and focus (a potent CNS stimulant and causes alertness, insomnia, increased concentration, euphoria or dysphoria and increased work capacity)
Because of its misuse especially by teenagers, its use is limited to the treatment of Attention Deficit Hyperactivity Disorder (ADHD) and narcolepsy.
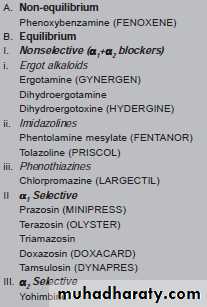
Adrenergic Blockers (antagonists/sympatholytics)
They are drugs that bind to adrenergic receptors but do not initiate the usual intracellular response.Block alpha & beta receptor sites (nonselective)
direct or indirect acting on the release of norepinephrine and epinephrine
Nonselective vs Selective Beta blockers
Nonselective have an equal inhibitory effect on B1 & B2 receptors –
Drugs have lots of interactions due to lots of alpha/beta receptor sites throughout body
use with caution on clients with cardiac failure or asthma
Selective B1 helpful in asthma clients
Therapeutic Uses of Non-Selective β- blockers
1. Hypertension: β- blockers are antihypertensive.Eg. Propranolol suppresses the activation of heart by blocking the β1 receptor. They reduce the work of heart by decreasing the cardiac output and causing a slight decrease in blood Pressure.
2. Glaucoma: Timolol and other ocular β- blockers are used to treat glaucoma. It neither affects the ability of eye to focus for near vision, nor changes pupil size. Used in chronic cases only.
3. Migraine: Effective in reducing migraine episodes due to blockage of catecholamine induced vasodilatation in the brain vasculature. Non selectibe β- blockers decrease the incidence and severity of the attack.
4. Hyperthyroidism: β- blocker blocks the peripheral conversion of thyroxine to triiodothyronine. It controls palpitation, nervousness, tremor & sweating etc.
5. Angina pectoris: β- blockers decrease O2 requirement and work of heart muscle and therefore is effective in reducing the chest pain on exertion which occurs in angina.
6. Myocardial infarction: It blocks the action of circulating catecholamines which would increase the oxygen demand in already ischemic heart muscle thereby limiting the infarct size.
7. Anxiety: Exerts an antianxiety effect during nervousness and panic attacks
8. Cardiac arrhythmias: It is life saving in protecting against serious cardiac arrhythmias. It suppresses tachycardia.
9. Pheochromocytoma
10. Hypertrophic obstructive cardiomyopathy: β- blockers inhibit the inotropic effect of sympathetic stimulation and may reduce intraventricular pressure gradient.
11. Essential tremor: Non selective β blockers are useful.
Selective β- blockers
It is cardioselective beta blocking agent and is devoid of intrinsic sympathomimetic activity. It reduces plasma renin activity in hypertensive patients.Metoprolol may be preferred to a nonselective agent in asthmatics and patients prone to develop hypoglycemia.
Its antianginal action is comparable to that of propranolol. It is metabolised by hydroxylation and excreted.
Alpha Adrenergic blockers
Blockade of alpha adrenergic receptors on vascular smooth muscle inhibits constriction of arteriole and veins.The result in decrease peripheral vascular resistance and a decrease blood pressure.
Blockade of alpha1 receptors in bladder smooth mm results in relaxation and decrease resistance to urine flow.Parasympathetic NSAcetylcholine
Important role in movement: causes muscle contractionAlso found in brain: important role in attention, learning & memory.
Manipulation of Ach level in the brain affects a wide range of cognitive functions including attention, learning & memory.
Ach thought to play a role in memory by maintaining neuron excitability.
Cholinergic Agonists
Acetylcholinesterase inhibitors - inhibit the enzyme acetylchoinesterase (AChE), responsible for breakdown of Ach.This results in increased cholinergic activity (at both nicotinic and muscarinic receptors).
They are :
Direct acting - act on the receptors to activate a tissue response
Indirect acting - inhibit the action of the enzyme cholinesterase (acetylcholinesterase - ACH)
Receptor-Acting Agonist
Acetylcholine: Ach does not penetrate BBB therefore it has no central effect .Carbachole: Has an enhanced binding to Nicotinic receptors. Also binds to muscarinic rec. Used as a topical mitotic agent: treatment of glaucoma.
Bethanechol: Selective to muscarinic receptors.
Eye: contraction of smooth muscle of iris
Ciliary muscle: when muscarinic R. are stimulated, it causes contraction.
Lense become more spherical.
Accomolation for near vision occurs
GIT: treatment of Abdominal distension
Bladder: stimulate the detrusor muslce of the bladder to contract
Methacholine
Nicotine
Indirect cholinergic agents
Anticholinersterase agent or ChEstrase inhibitors.
They prevent the degradation of acetylcholine esterase therefore prolong life of Ach.
They divide to reversible and irreversible ChEsterase inhibitors.
To Treat symptoms of Alzheimer's Disease by increasing central cholinergic activity and parasympathetic tone.
Physostigmine, Neostigmine
Physostigmine
It can cross the BBBUsed to treat myasthenia gravis, glaucoma, Alzheimer's disease and delayed gastric emptying.
Antidote of choice for the central nervous system effects of anticholinergic drug overdoses.
SE: Convulsion, muscle paralysis secondary to over-stimulation of the cholinergic R.
Generalized excessive cholinergic stimulation
Alzheimer’s diseaseDeficit in cholinergic transmission.
Degenerative disease of the cortex with loss of acetylcholine-producing cells and cholinergic receptors; characterized by progressive dementia.Symptoms: memory loss, confusion, mood swings, personality changes, hallucinations.
Cholinergic agonists can reduce symptoms and slow down disease progression.
Cholinergics such as: donepezil, rivastigmine and tacrine are indicated.
Cholinergic Antagonists
Muscarinic blockers
Neuromuscular blocking agents- inhibit the efferent impulses to skeletal muscle via the nicotinic muscle receptor (NM)
Ganglionic blockers- inhibit the nicotinic neuronal receptor (NN) of both parasympathetic and sympathetic ganglia
Cholinergic AntagonistsMuscrinic antagonists
AtropineScopolamine
Homatropine
Cyclopentolate
Tropicamide
Pirezepine
Pharmacological Action of Cholinergic Antagonists (Therapeutic uses )
CVS: Atropine is used for counteracting bradycardiaGIT: reduces salivary gland secretion & GI motility (Antispasmodic)
Pulmonary system: Reduces bronchial secretions and stimulates bronchodilation.
Urinary system: bladder wall relaxation
Eye: mydriasis.
Motion sickness: Scopolamine is indicated (CNS)
Sweat glands: suppresses sweating especially in children.
MEBEVERINE It shows effect on colonic muscle activity. It is indicated in smooth muscle spasm.
IPRATROPIUM BROMIDE : Treatment of COPD