CERVICAL SPONDYLOSIS
Dr. Moneer K. Faraj
Consultant Neurosurgeon
College of Medicine, Baghdad. Uni.
DEFINITION
Degenerative alterations of the cervical spine
PATHOGENESIS
It is an aging process (“wear and tear”,
degeneration) which may be accelerated due to
trauma or disease e.g. Rheumatoid arthritis.
It represents a mixed group of pathologies
involving the intervertebral discs, vertebrae,
and/or associated joints.
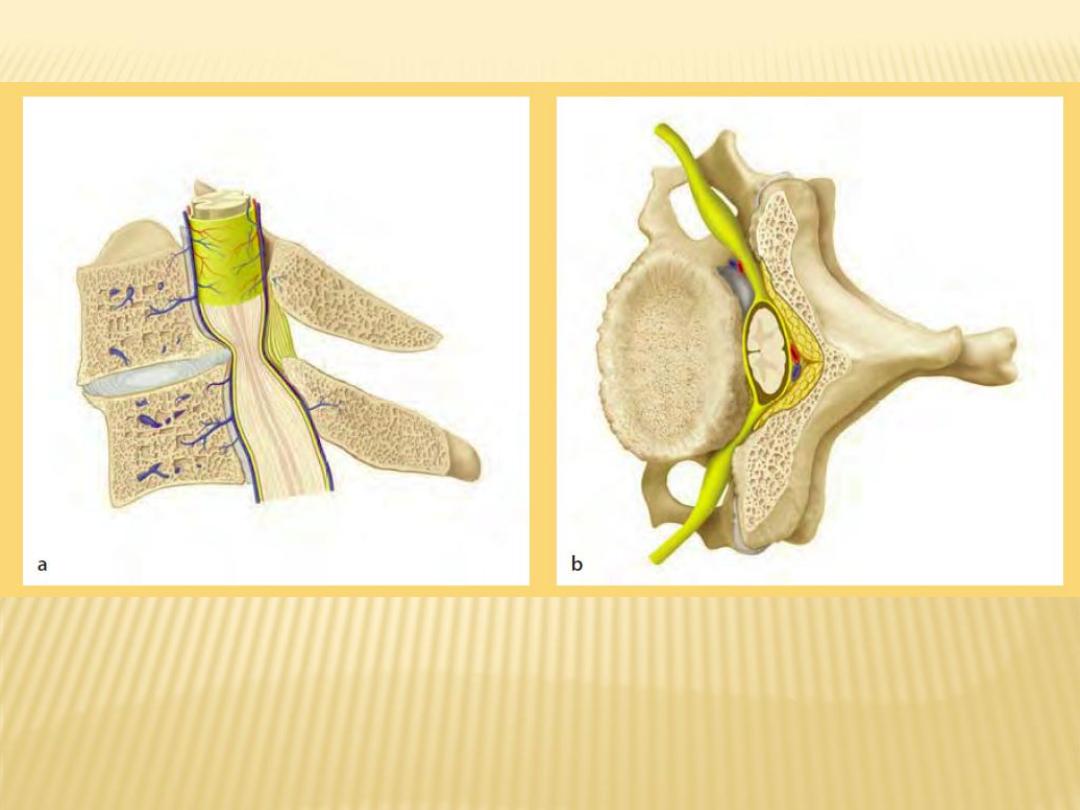
The disc height decreases leading to disc bulging.
Micro instability results in reactive hyperostosis
with formation of osteophytes at the vertebral
endplates which can penetrate into the spinal
canal and compromise the spinal cord and nerve
roots.
Osteophytes of the uncovertebral and facet joints
reduce the mobility of the segment.
Segmental instability leads to a hypertrophy of the
yellow ligament and causes a narrowing of the
spinal canal and foramen
Cervical Kyphosis may occur in late stages
EPIDEMIOLOGY
The prevalence of neck pain ranges between
17%and 34%in a general population.
Cervical Spondylosis mainly affects individuals
in the 4th and 5th decades of life .
HISTORY
:
CLINICAL FEATURES
A. The spondylotic syndrome
The pain arises from the motion of the degenerated
segment accentuated by movement and during specific
positions (e.g. reading, computer work, driving).
Pain during the night may indicate severe facet joint
osteoarthritis
Pain is often associated with non-dermatomal shoulder
girdle pain.
Patients often report vague numbness, thermal sensations,
and tingling.
vertigo and dizziness are not uncommon but their causes
are not well explored
Headaches are frequent concomitant symptom.
B. Radicular Syndrome:
radicular pain, i.e. pain following a
dermatomal distribution. The sensory, motor
and reflex deficits are dependent on the
affected nerve root.
It is important to note that the pain not only
radiates into the skin (dermatome) but also
into the muscles (myotomes) and bone
(sclerotomes
C. Myelopathic Syndrome:
can begin very subtly. The leading symptoms
are numbness, clumsy, painful hands with
disturbed fine motor skills (particularly
writing skills).
Later they presents with long tract signs, gait
disturbance and sphincter disorders
SIGNS
:
CLINICAL FEATURES
In patients with spondylotic syndrome, findings
are:
stiff neck with limited range of cervical motion
neck pain on extension and rotation
referred pain on motion (occiput, shoulder,
upper limb)
chronic trapezius myalgia
In patients with radiculopathy, frequent findings
are :
sensory deficit
motor deficit
reflex deficits
positive Spurling test or neck compression test
which is performed with the patient in the
sitting position. The neck is extended and
rotated to the side of the pain. Then, a careful
axial compression of the head is applied; if
positive, the patient reports pain radiating
along the compromised nerve root
In patients with cervical myelopathy,
frequent findings are:
atrophy of the interosseous muscles
muscle weakness
spasticity, hyperreflexia, and clonus
pathologic reflexes, positive Babinski sign
sensory and vibratory deficits
gait disturbances (broad, abrupt and jerky)
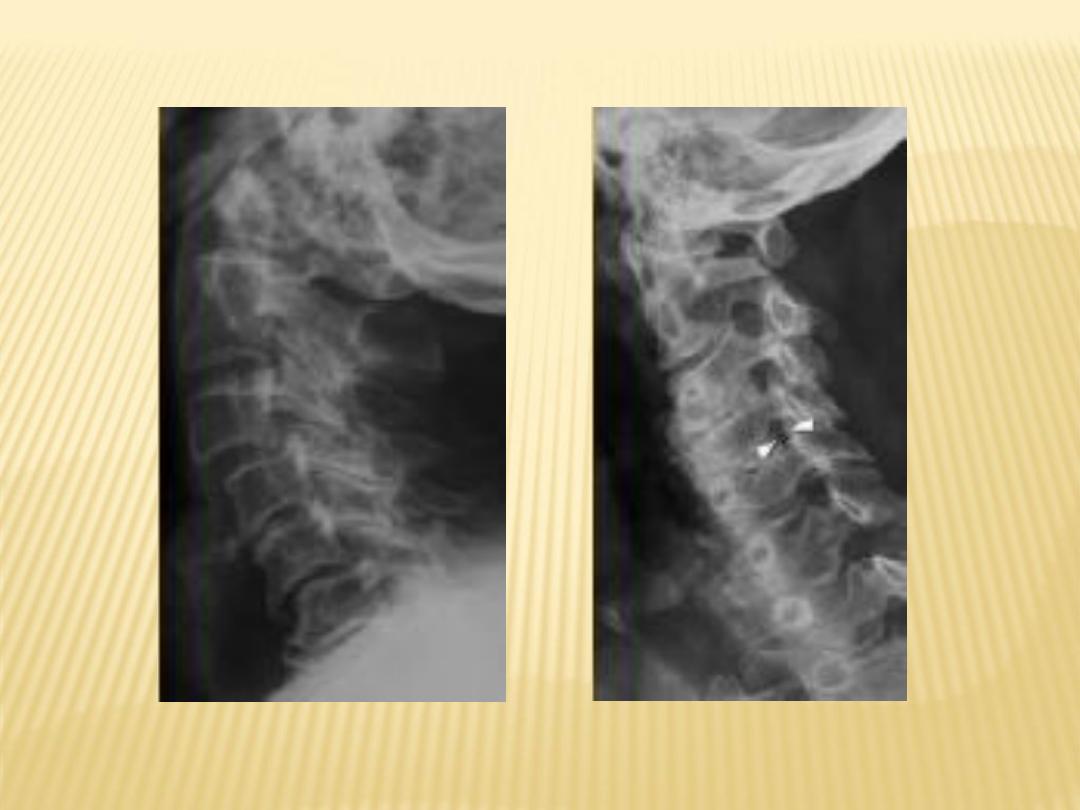
INVESTIGATIONS
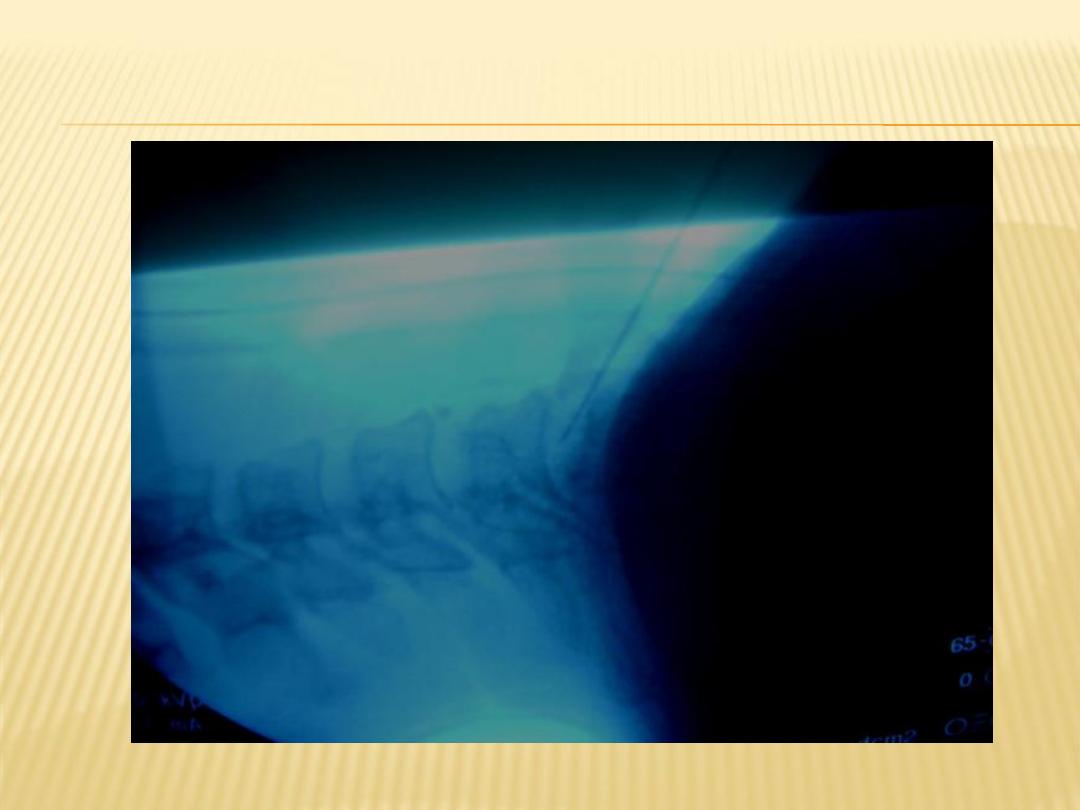
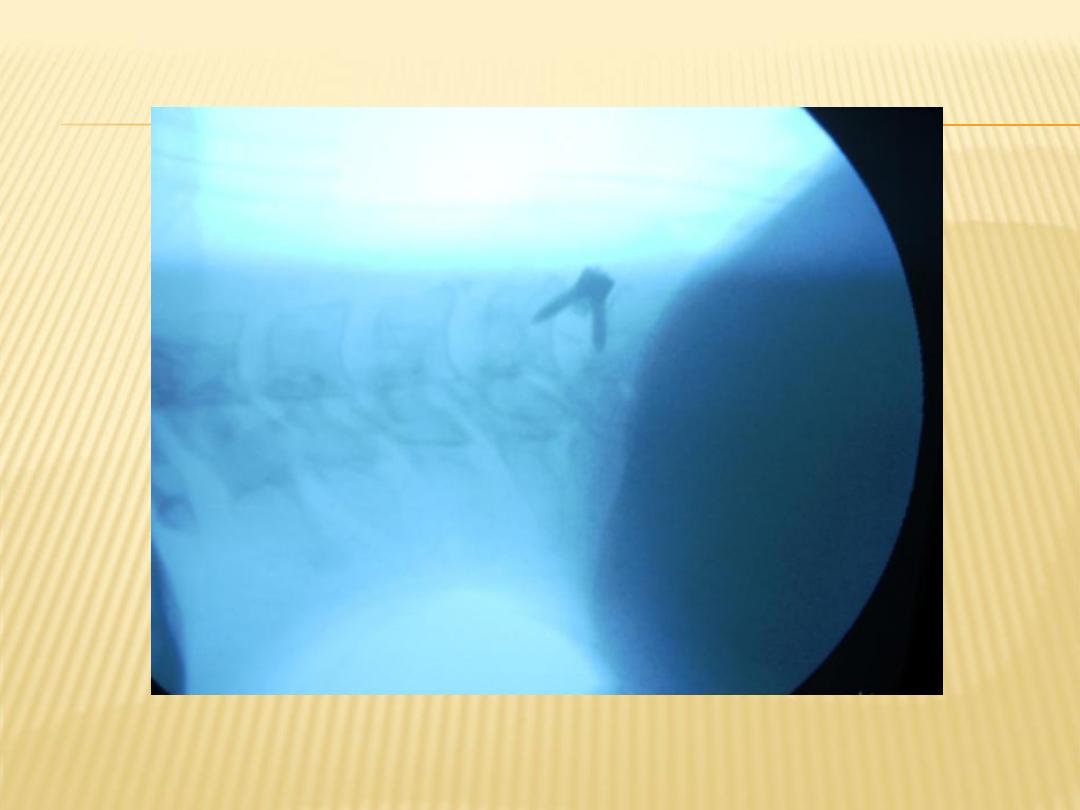
Plain Cervical spine X- Ray:
sagittal profile (e.g. loss of lordosis, kyphosis)
sagittal spinal canal diameter (<10mm at risk of
developing Cervical myelopathy .
spinal alignment and bony relationship (e.g.
spondylolisthesis)
disc space narrowing
bony vertebral structures (vertebral collapse,
osteophytes)
facet joint osteoarthritis
Narrow intervertebral foramen on oblique views

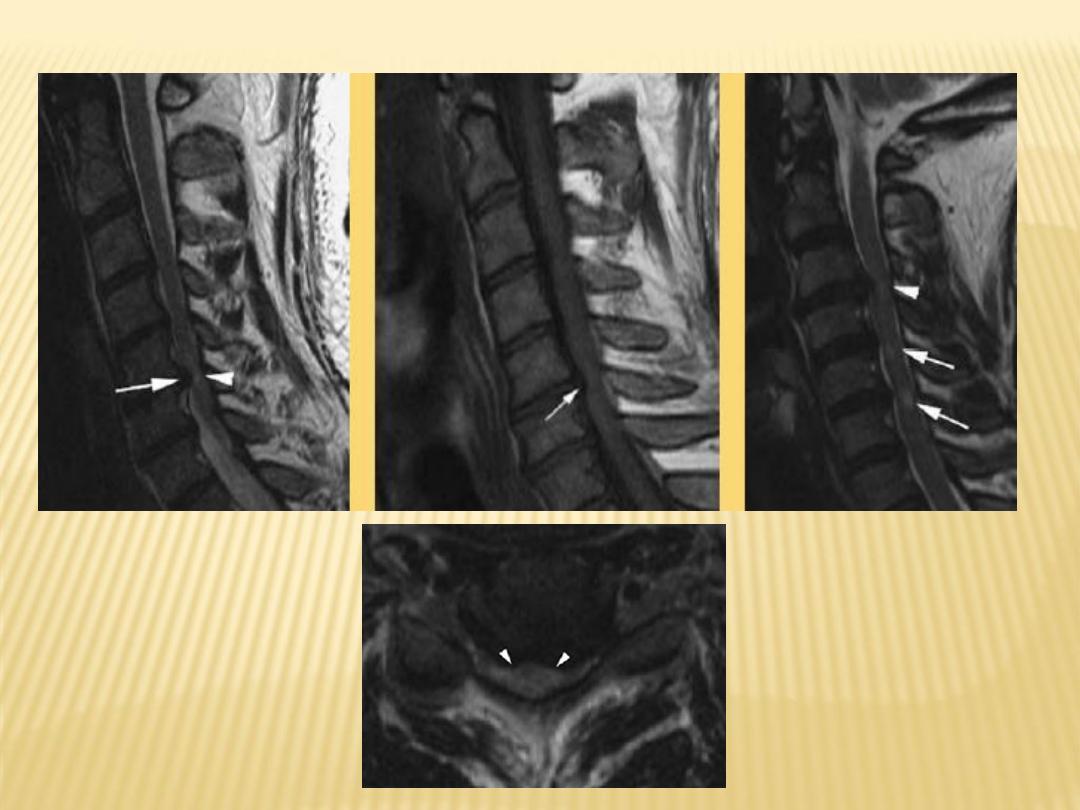
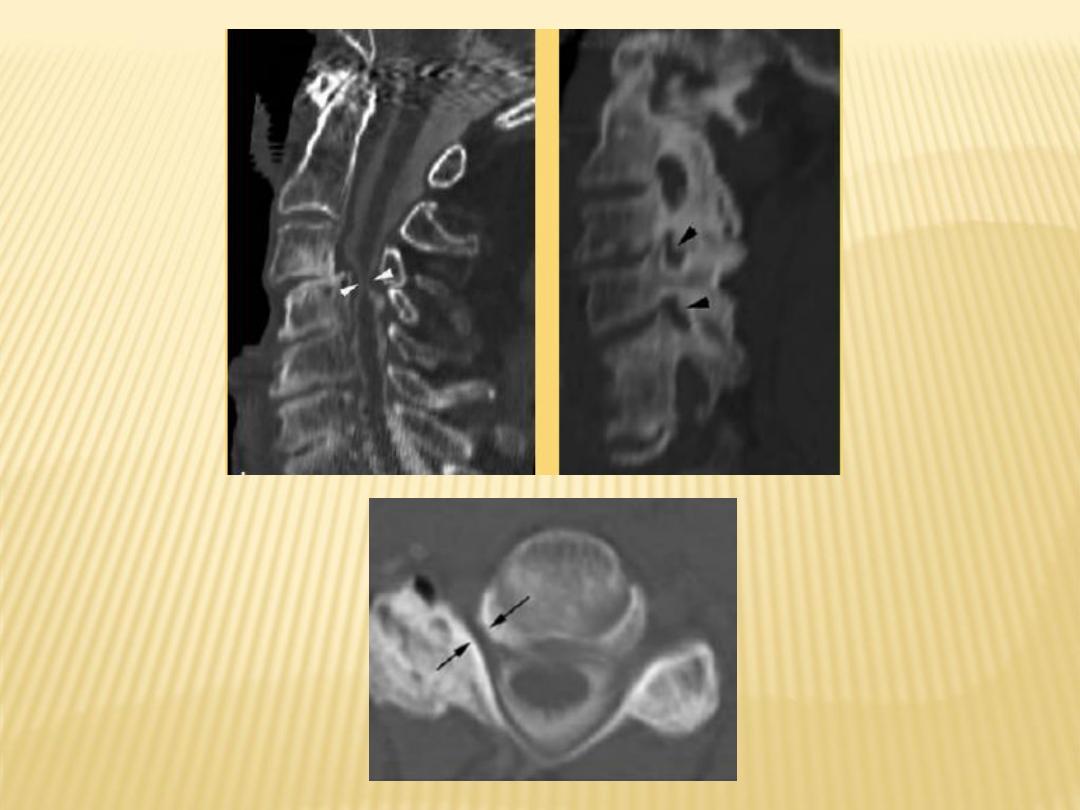
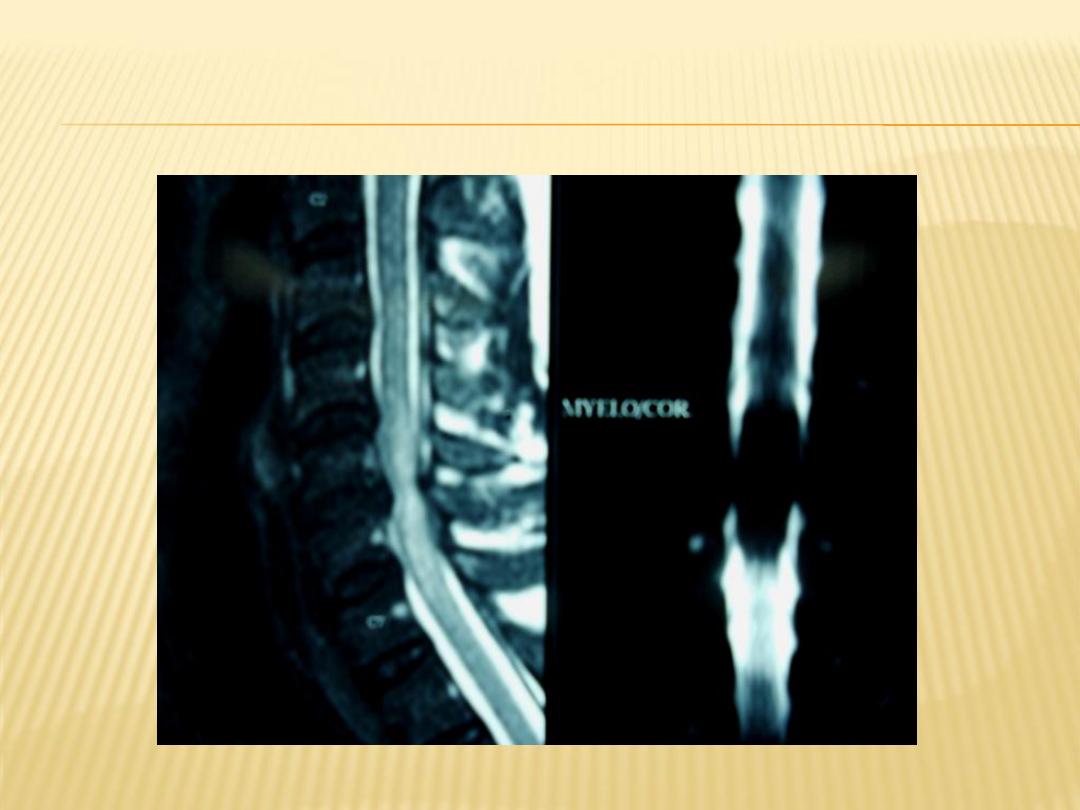
MRI: will shows detailed disc and neuronal
element changes.
CT- Scan: will shows bony pathologies
Neurophysiological studies (EMG, NCS)
. Helpful in differentiating radiculopathy
from peripheral neuropathy.
. They allow the recognition of subclinical
myelopathy
DIFFERENTIAL DIAGNOSIS
nerve entrapment syndromes
shoulder girdle disorders (rotator cuff tears,
impingement syndrome, tendinitis)
acute brachial plexopathy ,brachial
plexitis/neuritis (e.g. herpes zoster)
thoracic outlet syndrome
amyotrophic lateral sclerosis
tumors (e.g. Pancoast tumors)
coronary heart disease
TREATMENT
General objectives of treatment:
relieve pain
prevent neurological deterioration
improve functional limitations
reverse or improve neurological deficits
Oral Medications
Drug treatment for neck pain disorders consists
of:
analgesics
NSAIDs
muscle relaxants
psychotropic drugs
Cervical Collar
The treatment effect of cervical collars is
unproven
in acute neck pain.
Manipulative therapy particularly, traction has
been reported to result in short-term relief of
radiculopathy
SURGICAL THERAPY : INDICATIONS
progressive, functionally important motor
deficit
persistent pain despite non-surgical treatment
for at least 6 weeks
progressive myelopathy despite non-operative
care
progressive kyphosis with neurological deficits
THE GOAL OF CERVICAL SPONDYLOTIC
MYELOPATHY TREATMENT PRIMARILY IS
TO ARREST PROGRESSION
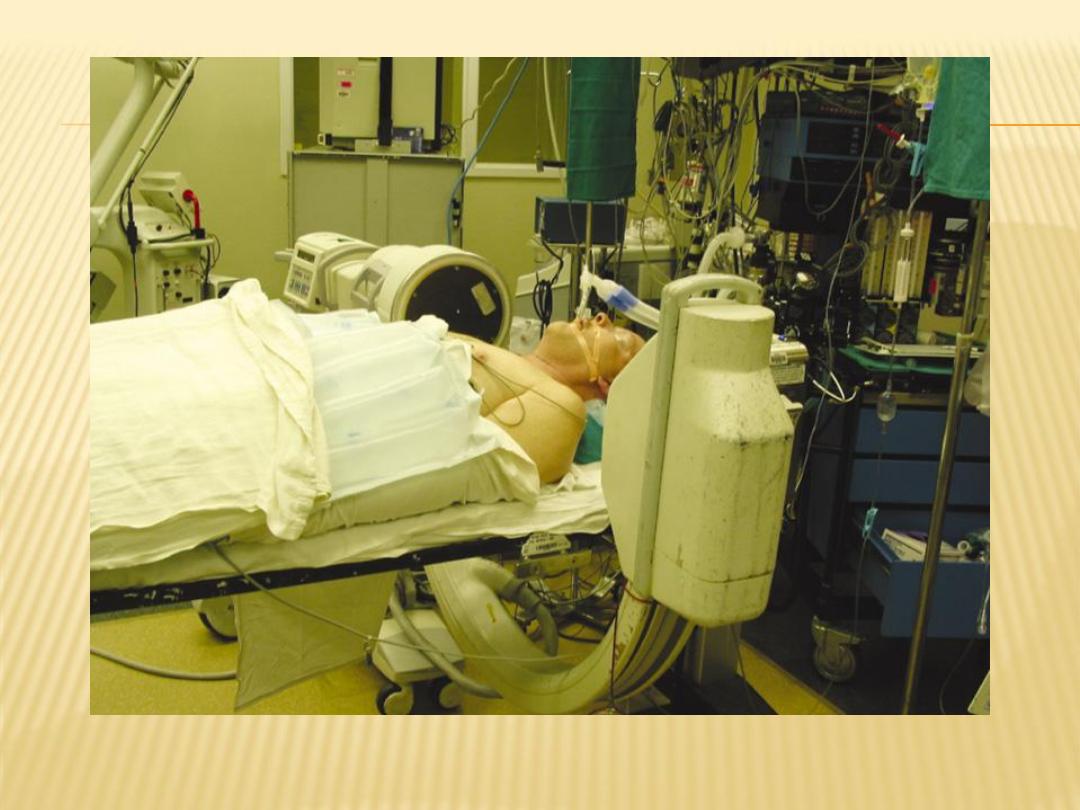
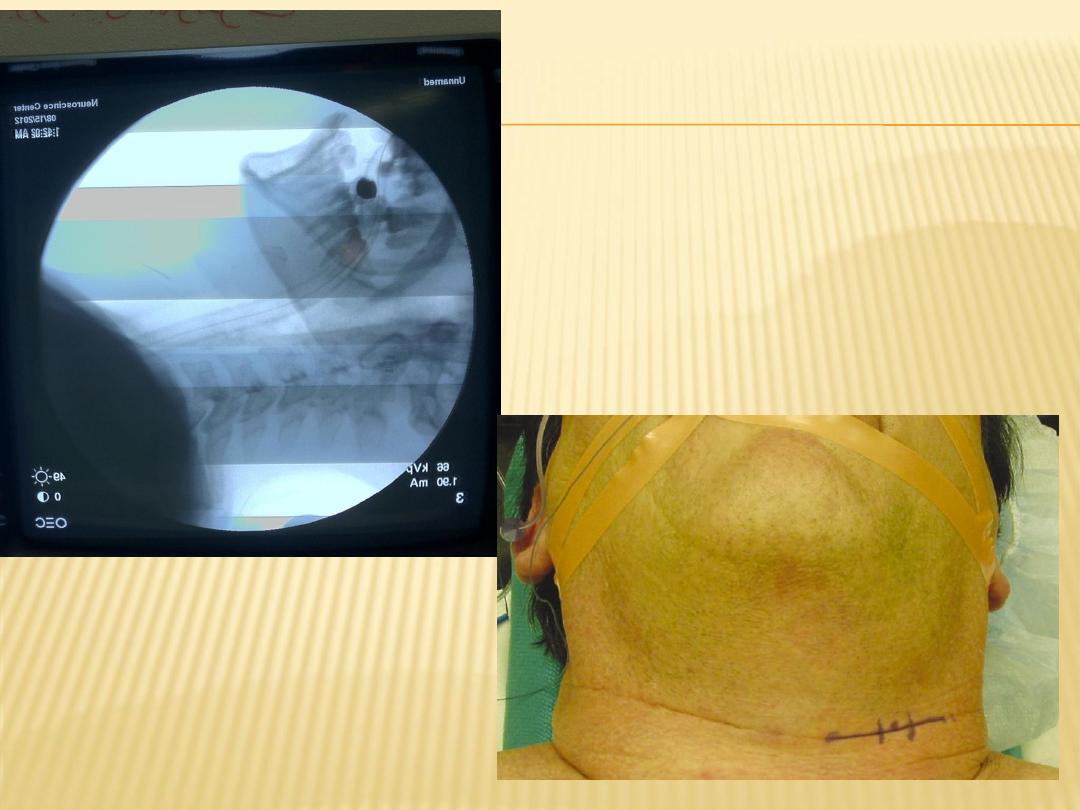
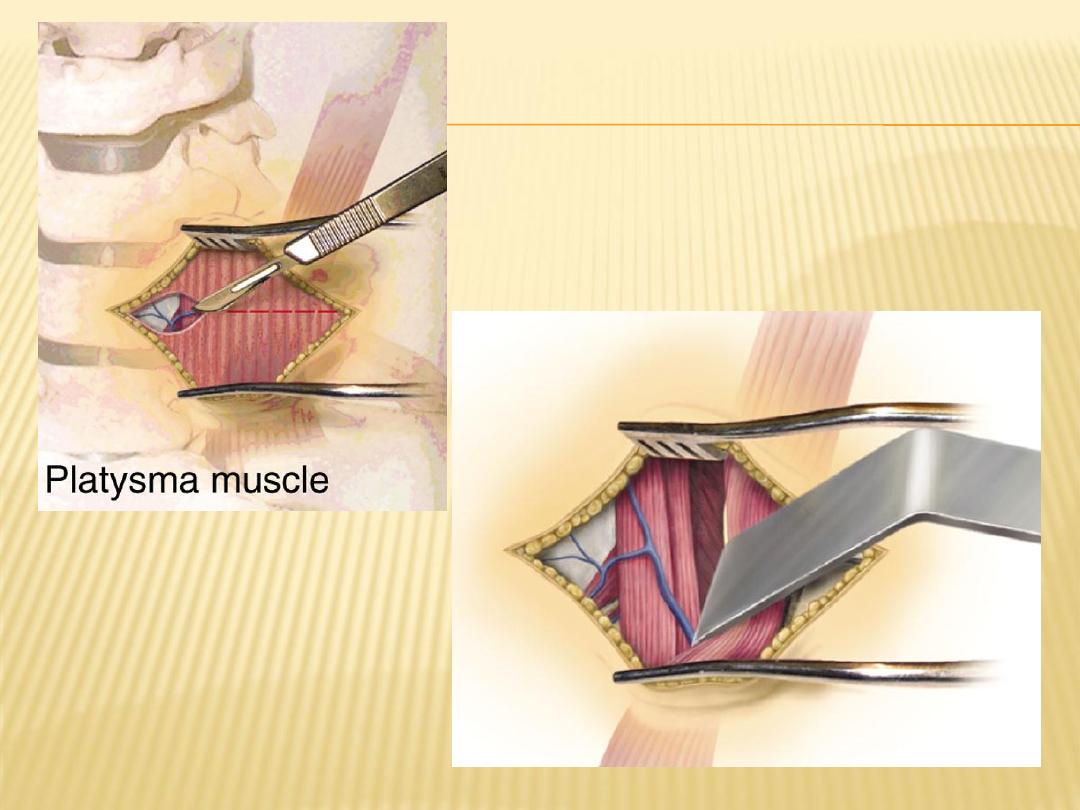
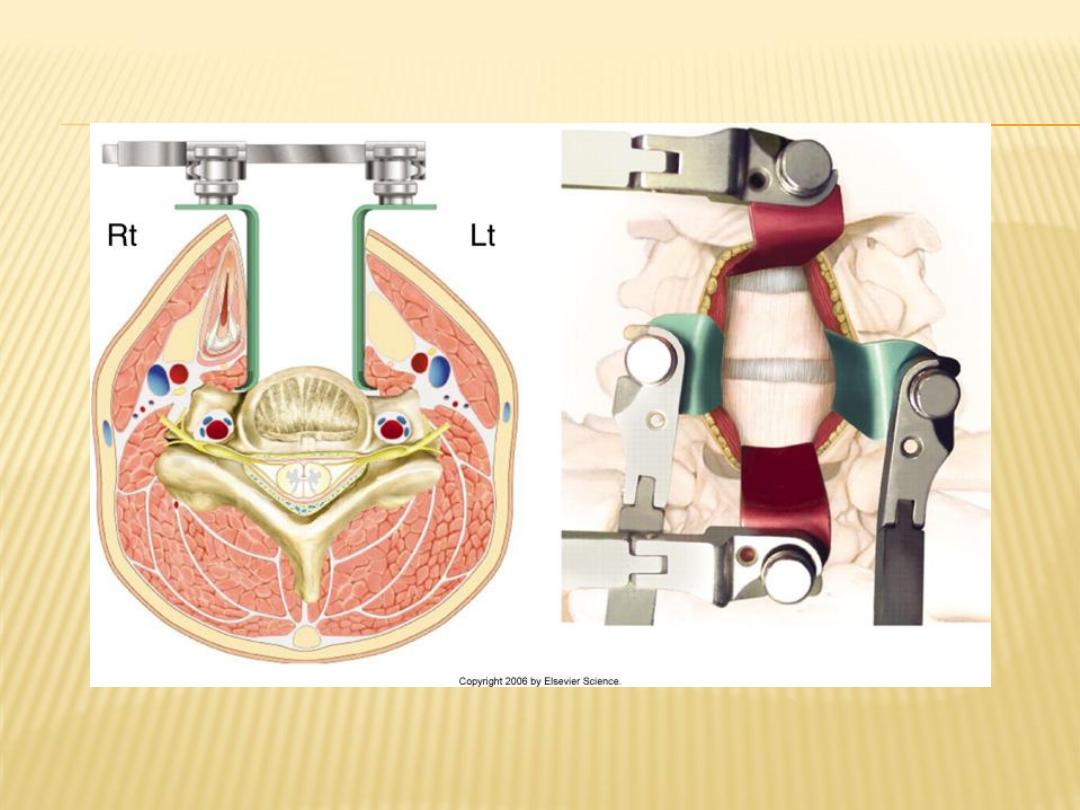
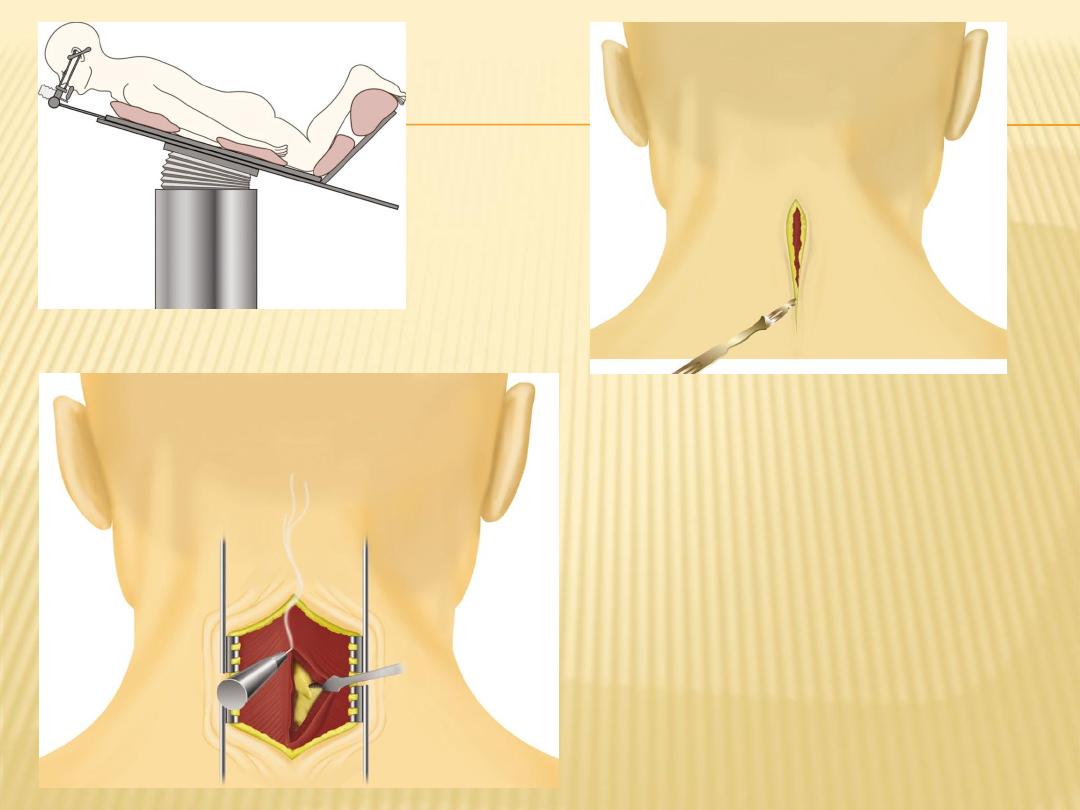
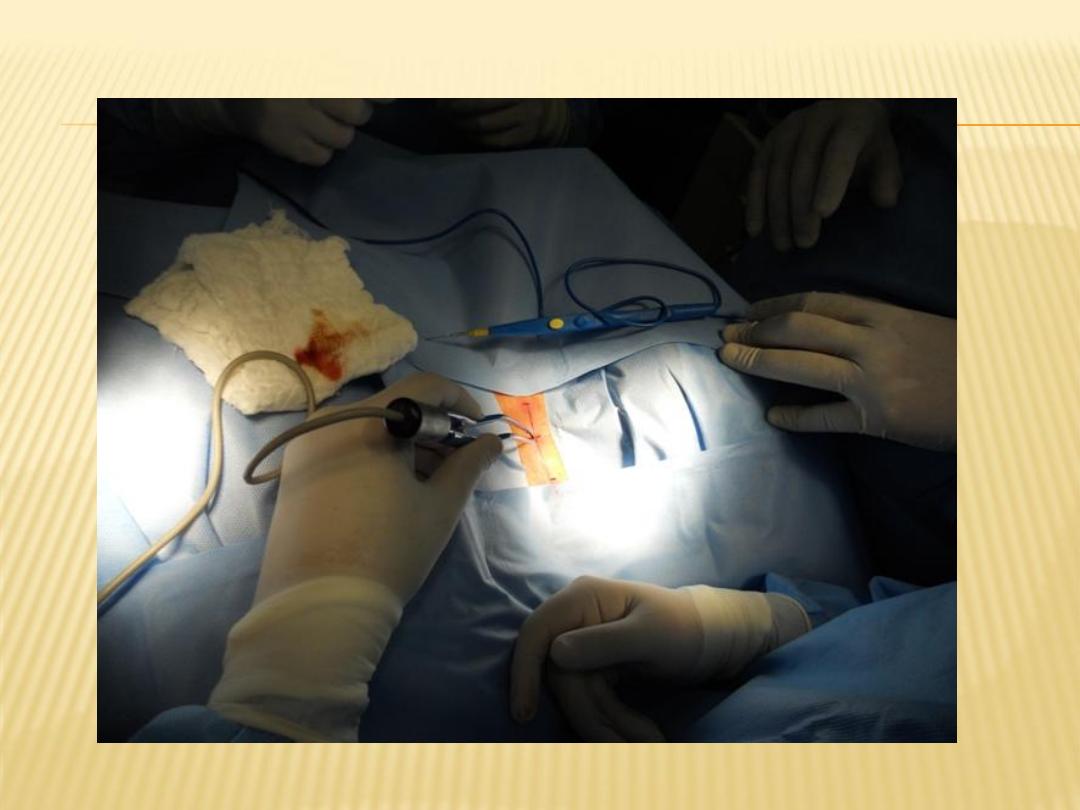
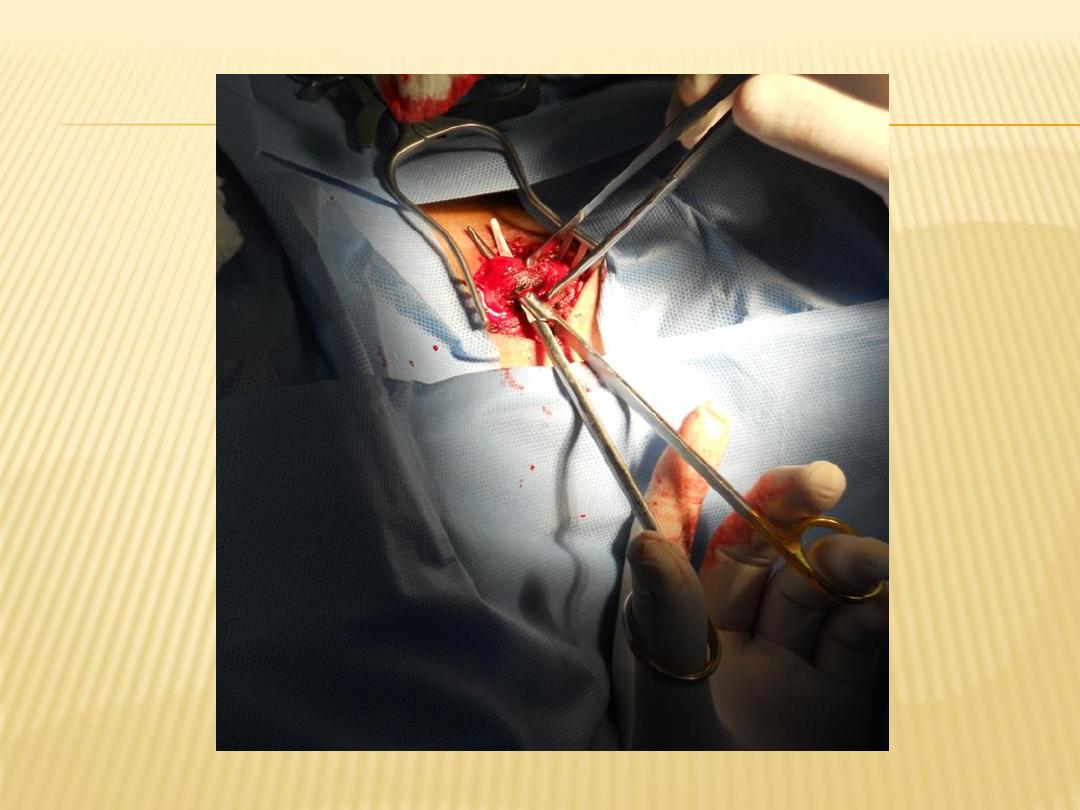
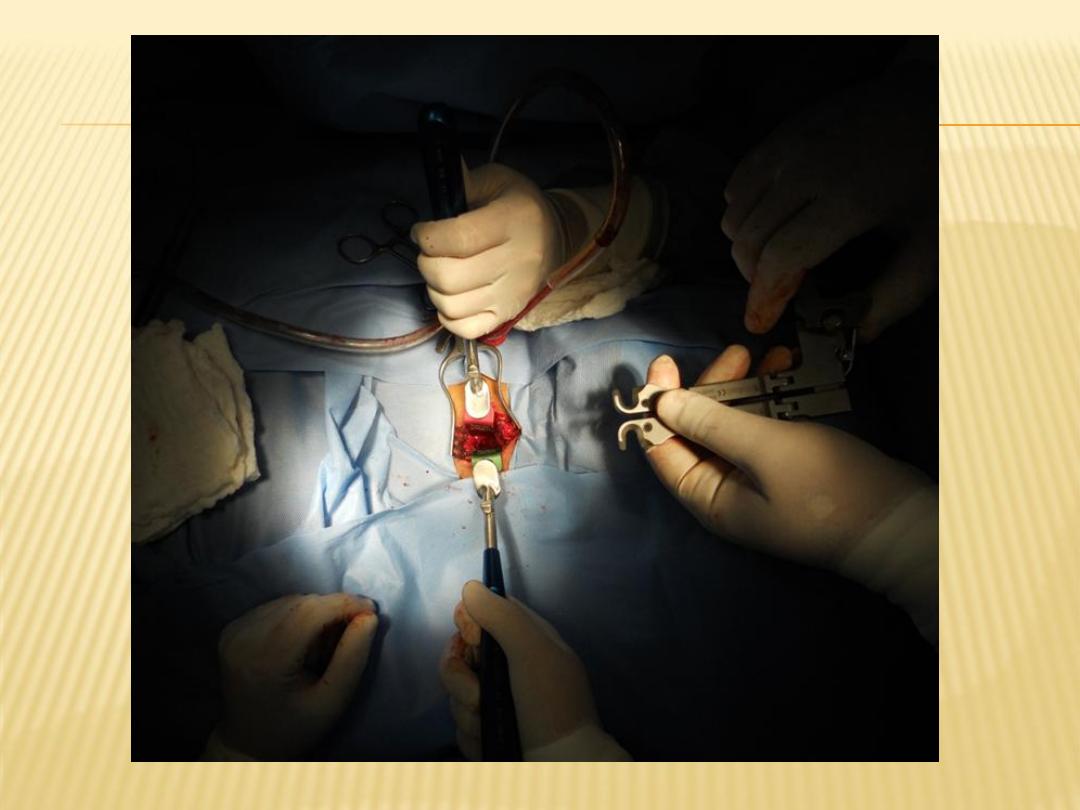
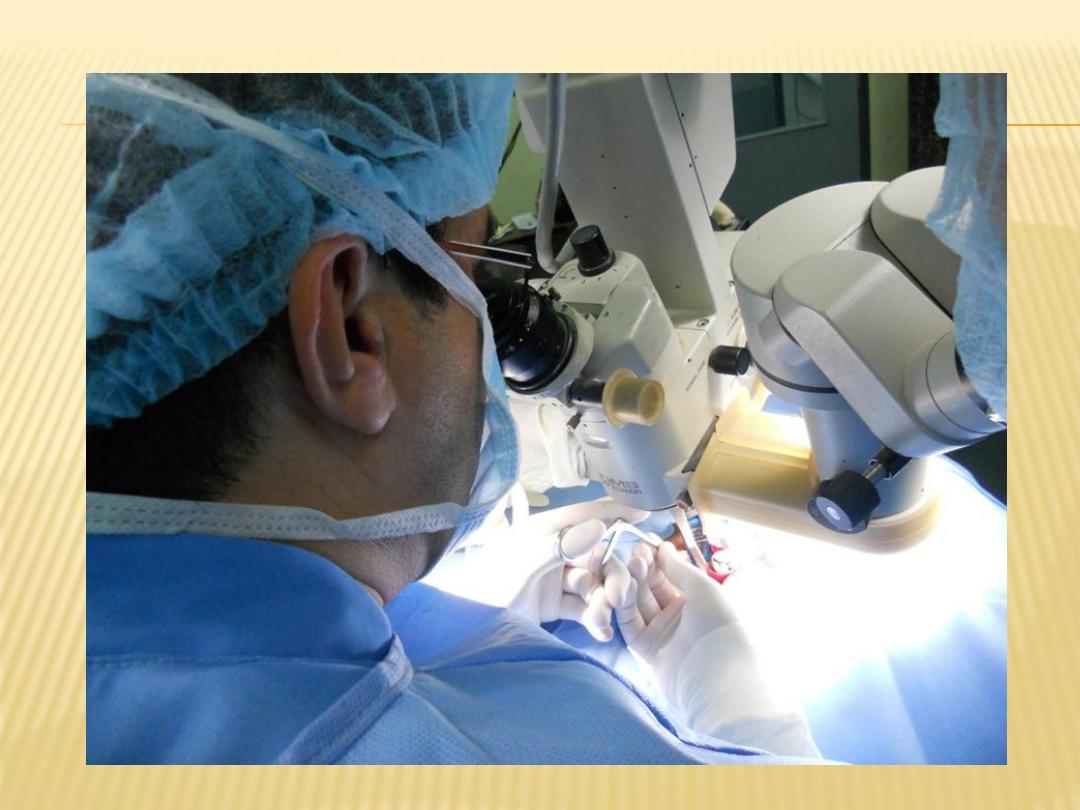
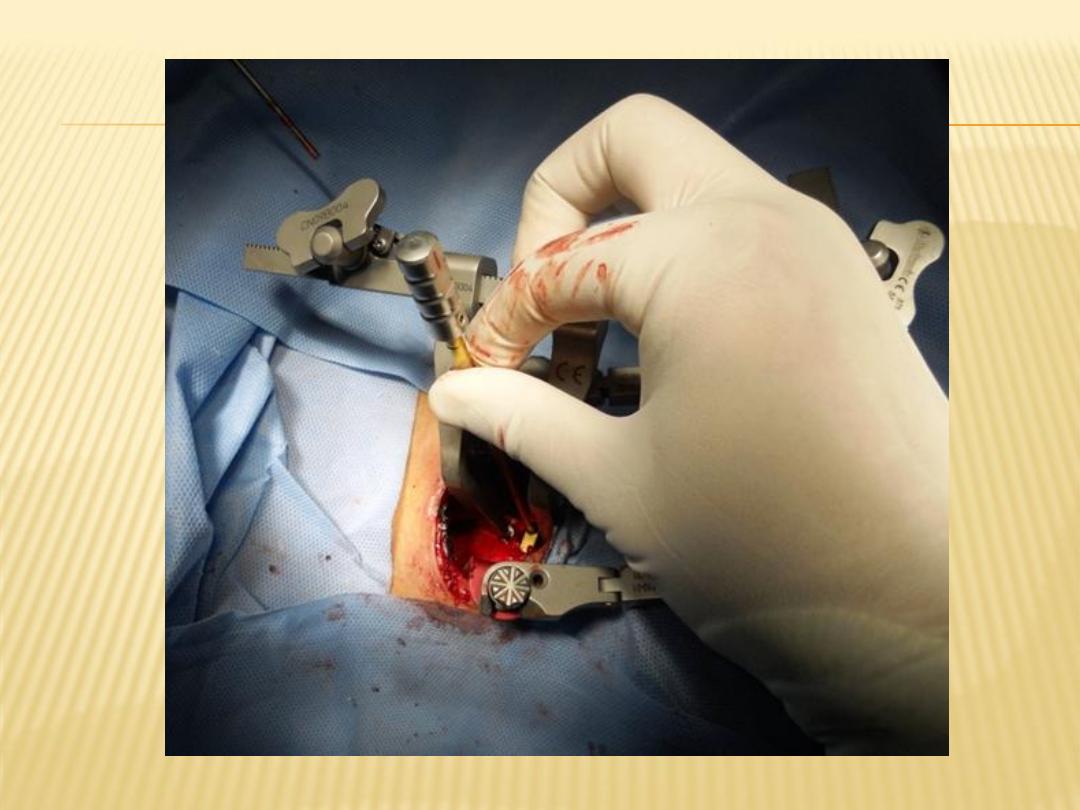
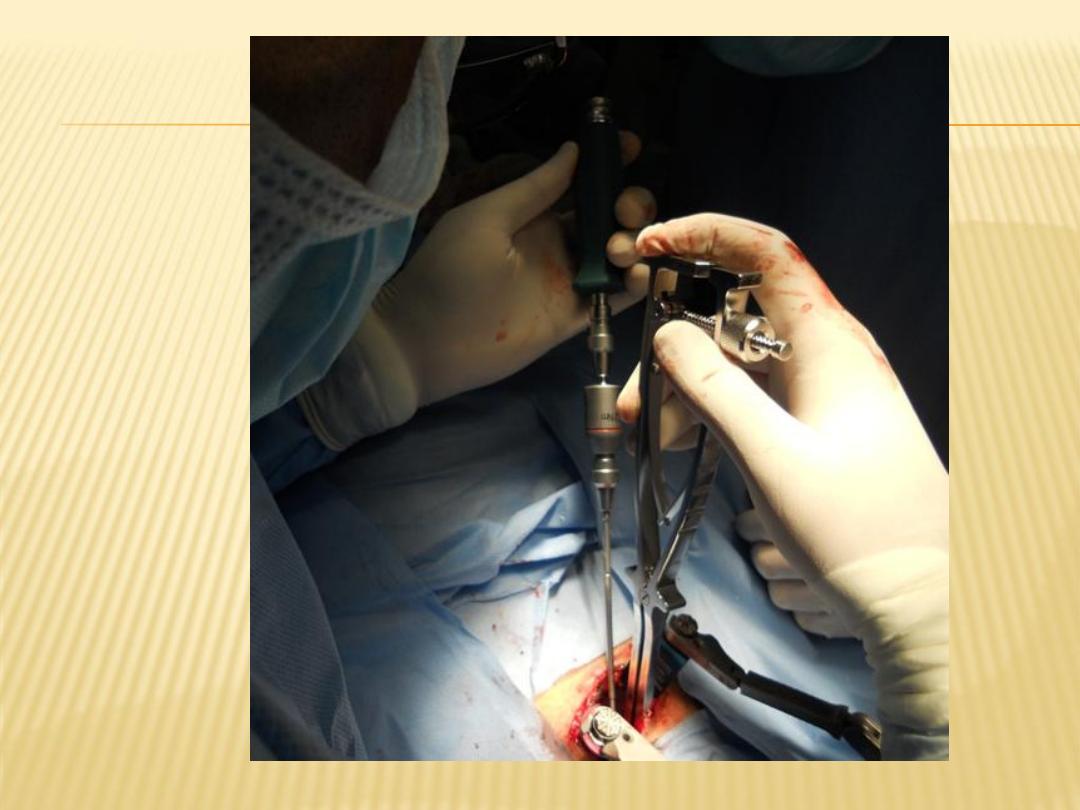
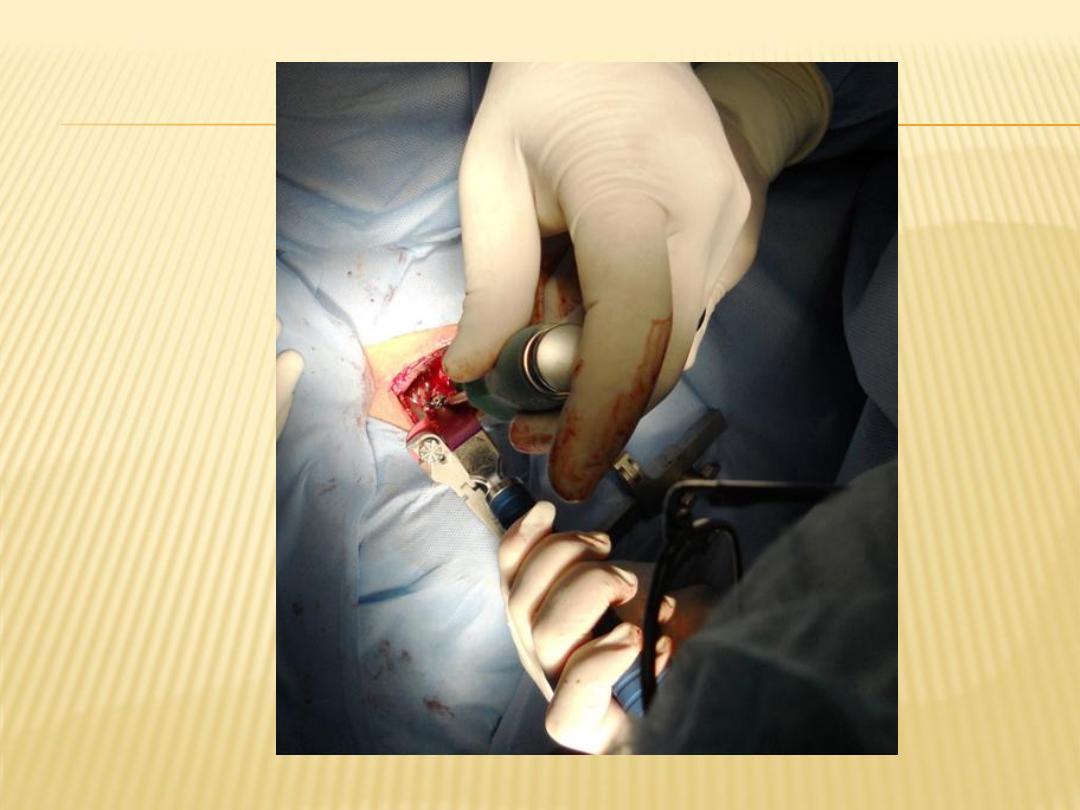
Anterior Cervical Approach
is indicated :
1- Cervical disc lesion
2- predominant anterior compression elements
3- Cervical myelopathy with kyphosis
Types:
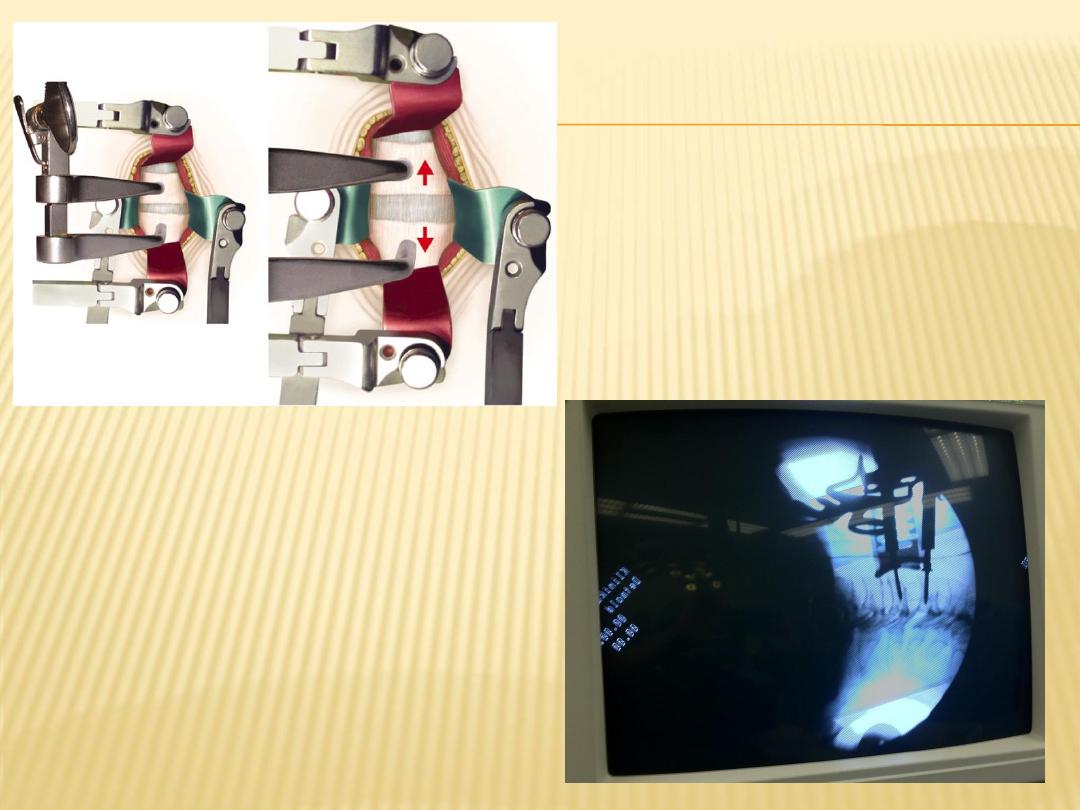
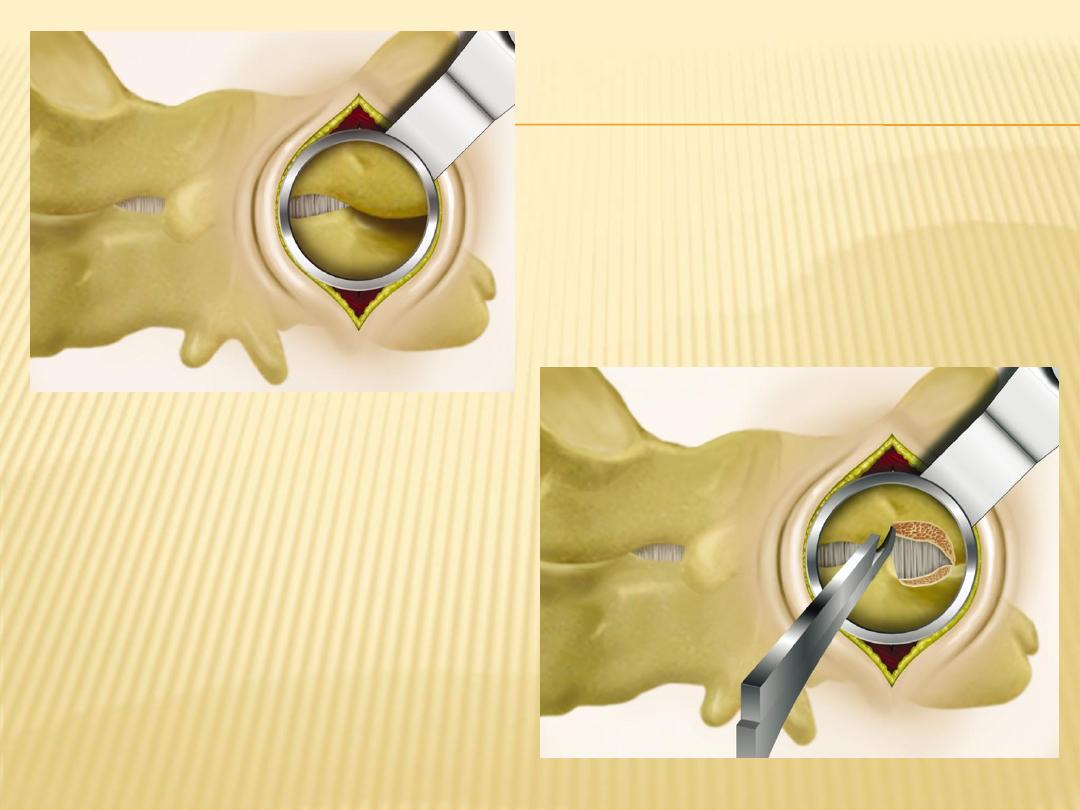
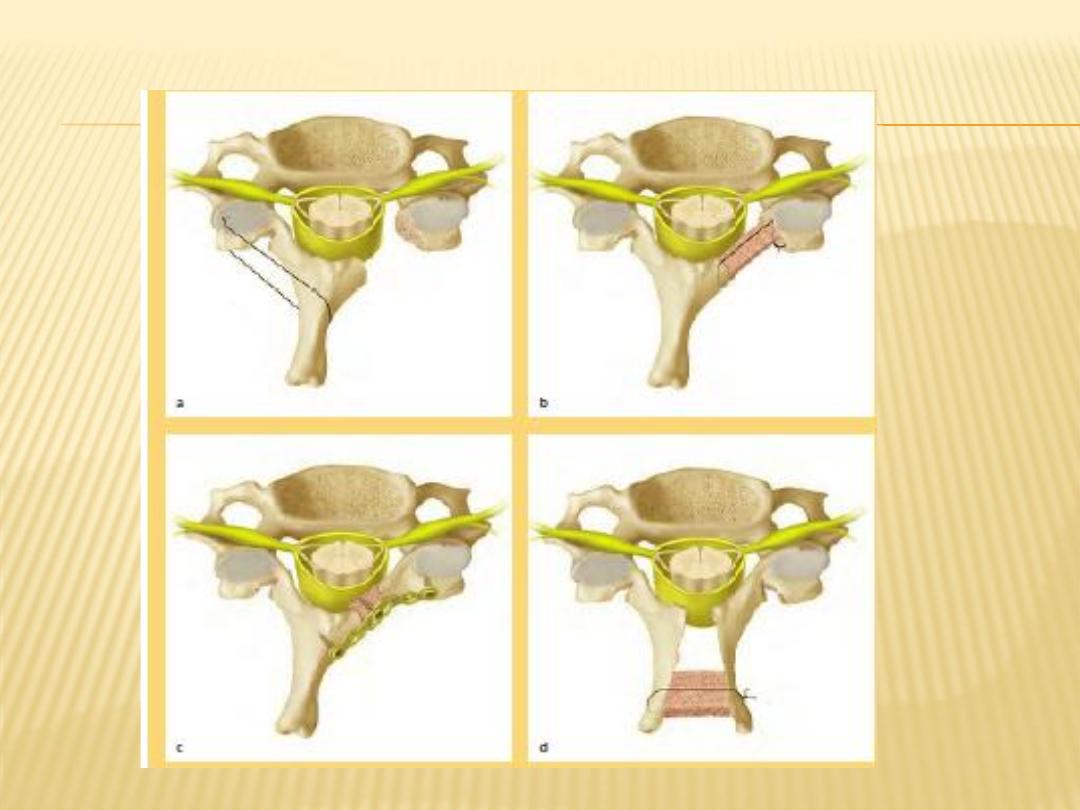
1-Anterior cervical discectomy and fusion: remains the
gold standard for Cervical Spondylotic Radiculopathy
2-Anterior cervical corpectomy with fusion

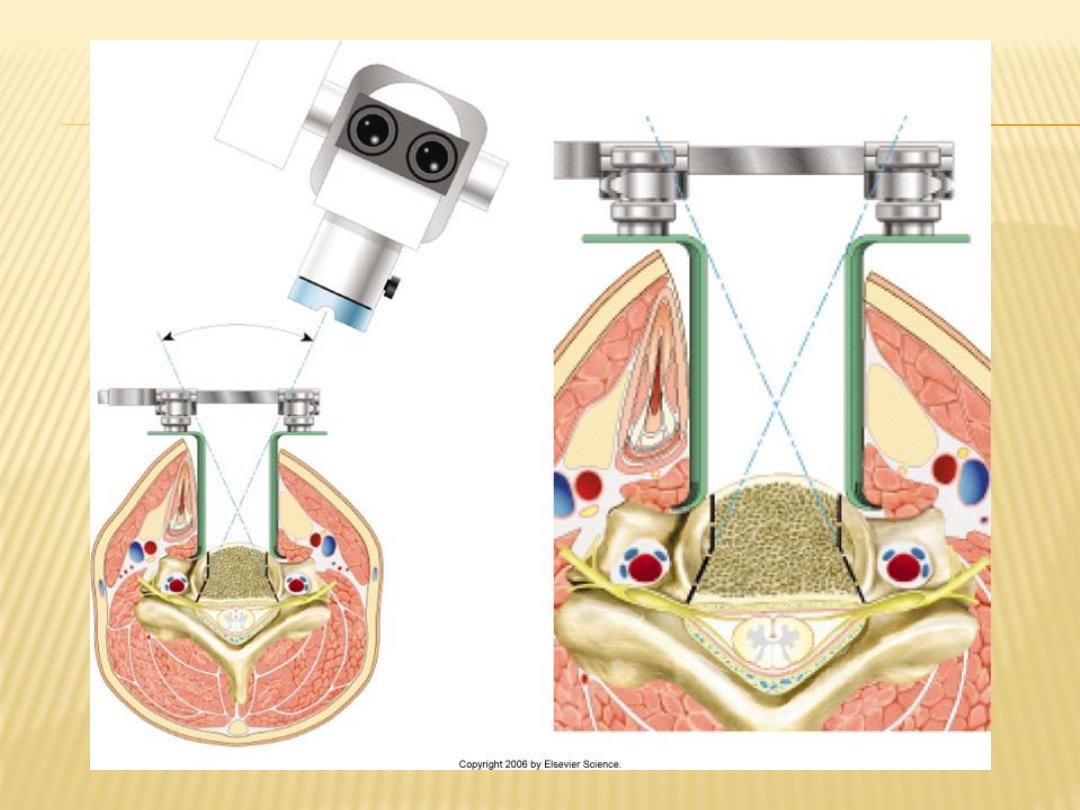
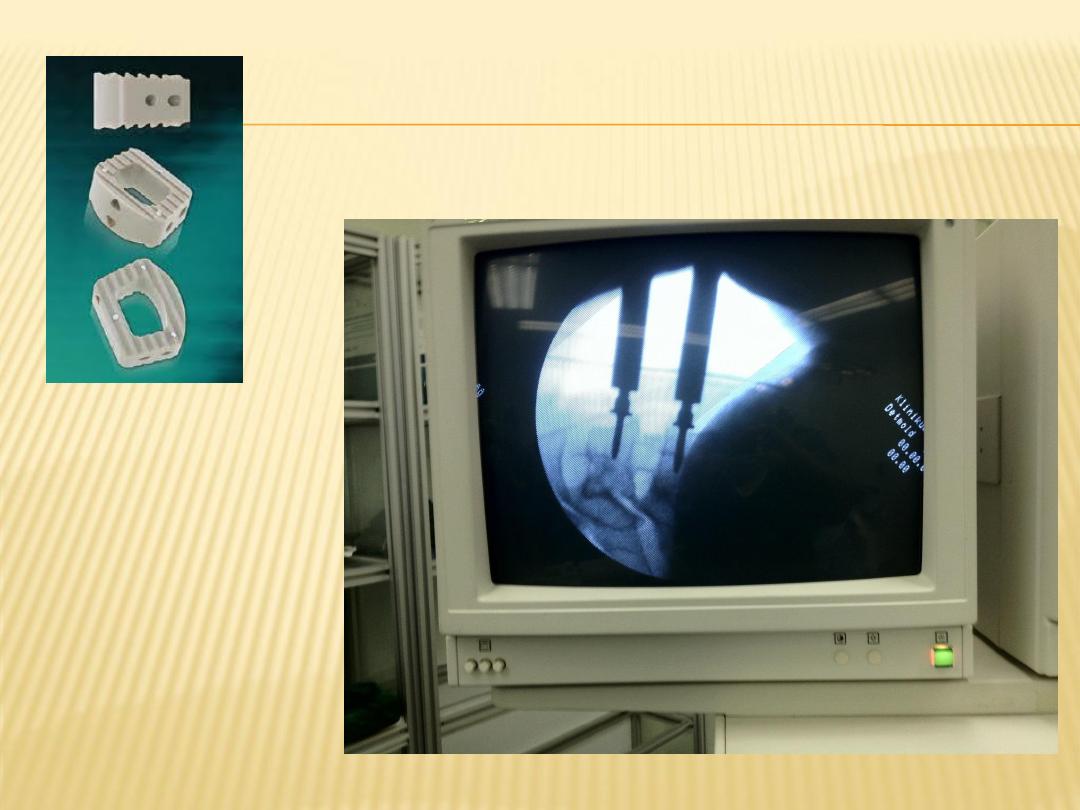

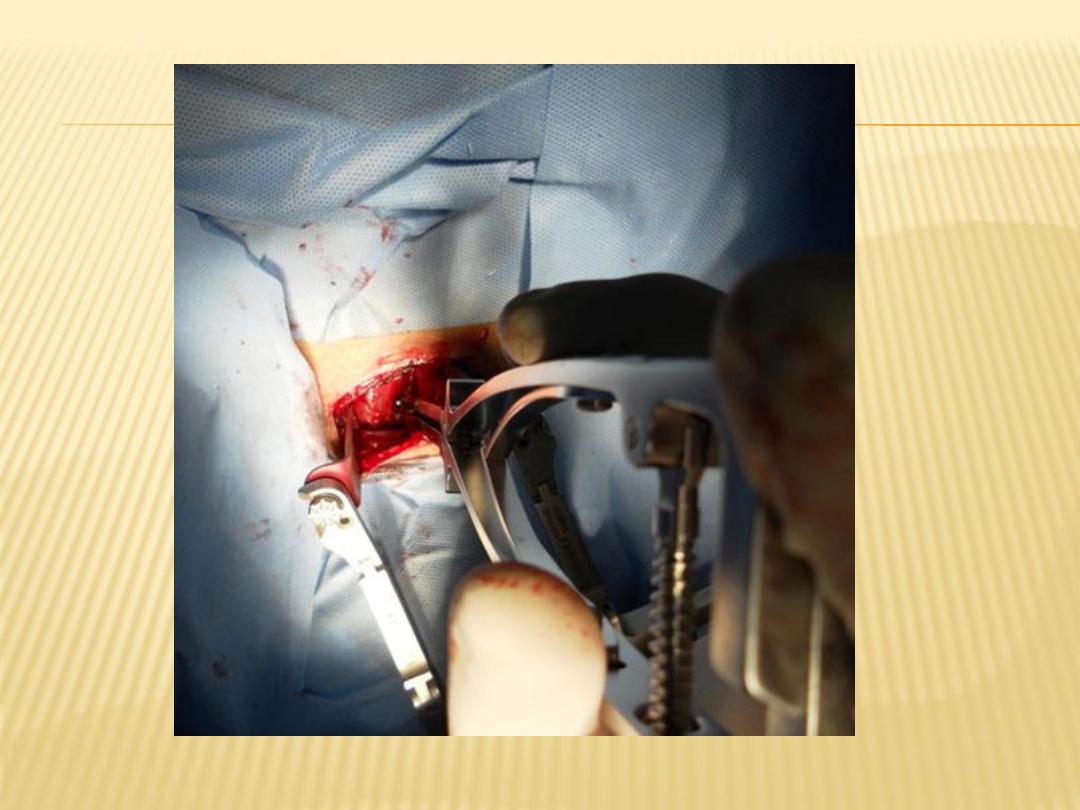
Posterior cervical approach
is indicated:
1.
multilevel cervical myelopathy
2.
predominant posterior neural compression
3.
cervical myelopathy with preserved cervical
lordosis
Types:
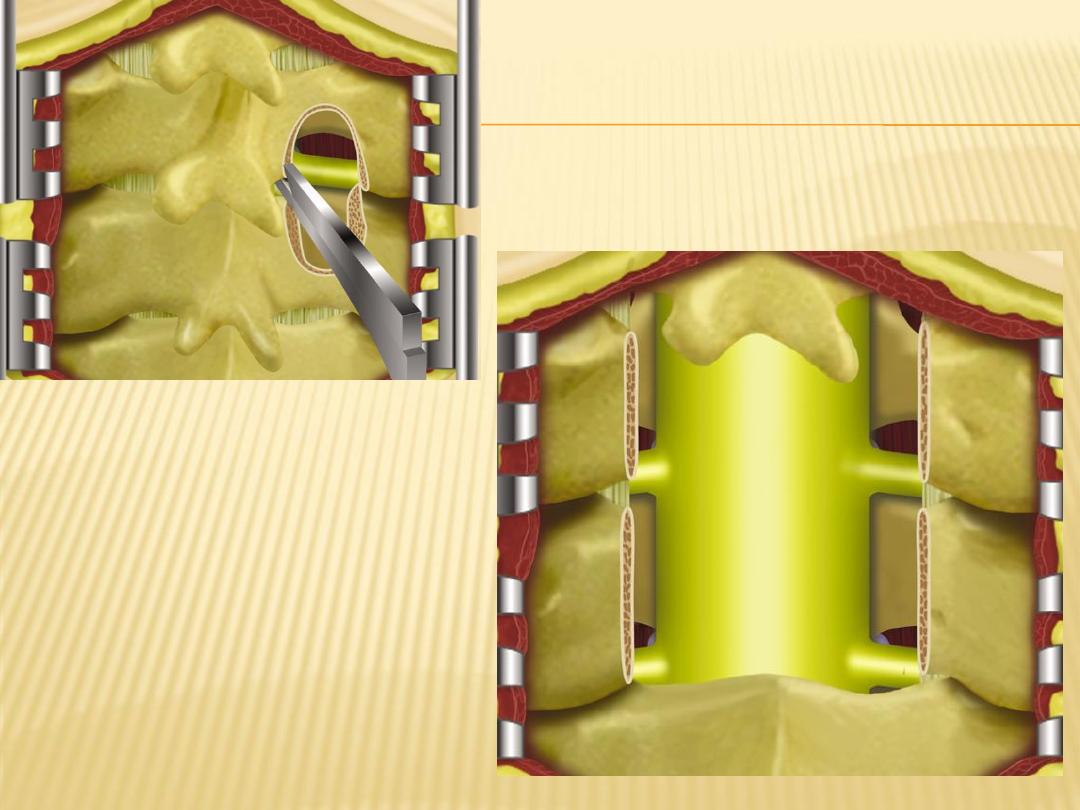
1.
Laminectomy
2.
foramenotomy
3.
laminoplasty:
POSTOPERATIVE COMPLICATIONS
cerebrospinal fluid leak (0.2–0.5%)
recurrent laryngeal nerve injury (0.8–3.1%)
dysphagia (0.02–9.5%)
Horner’s syndrome (0.02–1.1)
cervical nerve root injury (0.2–3.3%)
hematoma (0.2–5.6%)
Tetra paresis (0.4%)
death (0.1–0.8%)
infection (0.1–1.4%)
esophageal perforations (0.2–0.3%)
non-union (dependent on technique)
graft dislodgement/collapse (dépendent on technique ,
instrumentation failure (dependent on technique

THANK YOU



