Poisoning
Taking a history in poisoningWhat toxin(s) have been taken and how much?
What time were they taken and by what route?
Has alcohol or any drug of misuse been taken as well
?
Obtain details of the circumstances of the overdose from family, friends and ambulance personnel
Ask the general practitioner for background and details of prescribed medication
Assess suicide risk (full psychiatric evaluation when patient has physically recovered)
Capacity to make decisions about accepting or refusing treatment?Past medical history, drug history and allergies, social and family history?
Record all information carefully
Patients who are seriously poisoned must be identified early so that appropriate management is not delayed. Triage involves:
immediate measurement of vital signs
identifying the poison(s) involved and obtaining adequate information about them
identifying patients at risk of further attempts at self-harm and removing any remaining hazards from them.
The Glasgow Coma Scale (GCS) is commonly employed to assess conscious level, although it has not been specifically validated in poisoned patients.
An electrocardiogram (ECG) should be performed and cardiac monitoring instituted in all patients with cardiovascular features or where exposure to potentially cardiotoxic substances is suspected.
Patients who may need antidotes should be weighed when this is feasible, so that appropriate doses can be prescribed.
Substances that are unlikely to be toxic in humans should be identified so that inappropriate admission and intervention are avoided
Substances of very low toxicity
Writing/educational materialsDecorating products
Cleaning/bathroom products (except dishwasher tablets which are corrosive)
Pharmaceuticals: oral contraceptives, most antibiotics (but not tetracyclines and antituberculous drugs), H2-blockers, proton pump inhibitors, emollients and other skin creams, baby lotion
Miscellaneous: plasticine, silica gel, household plants, plant food
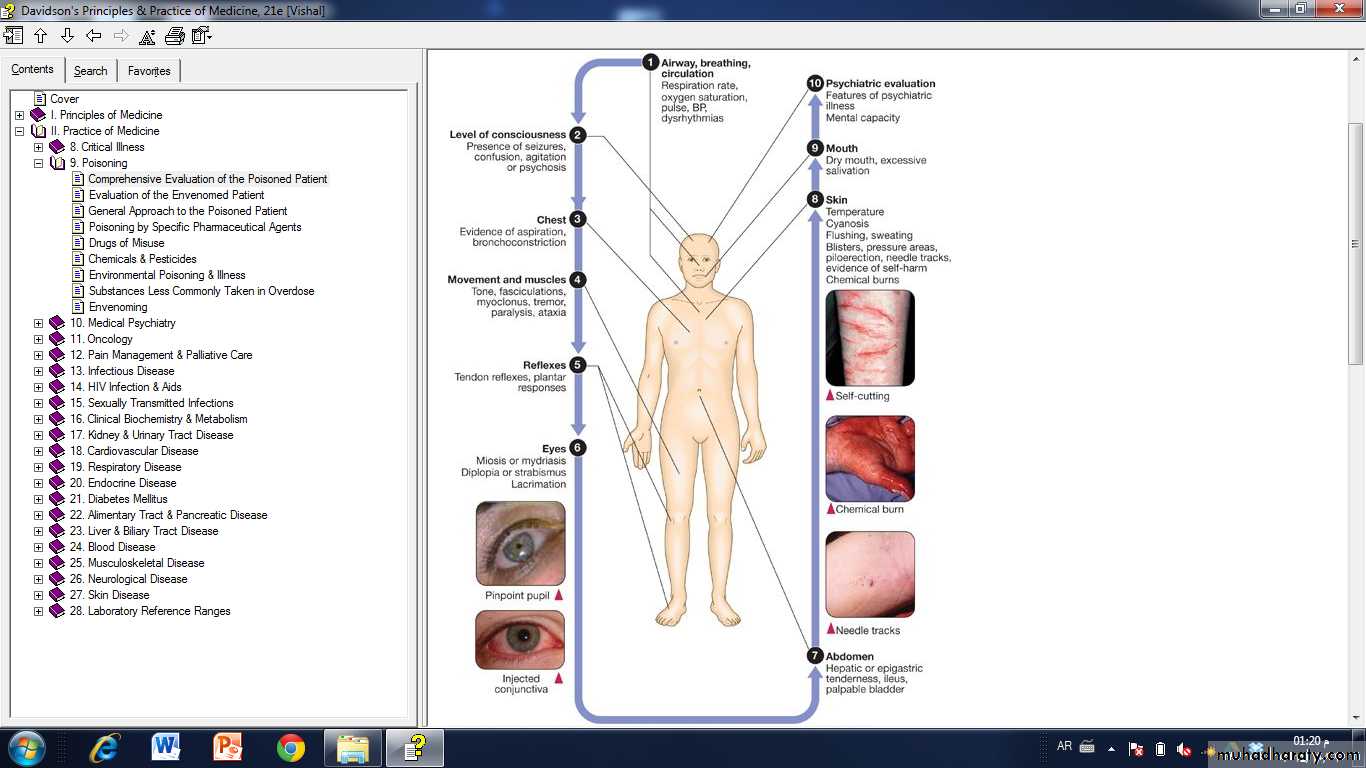
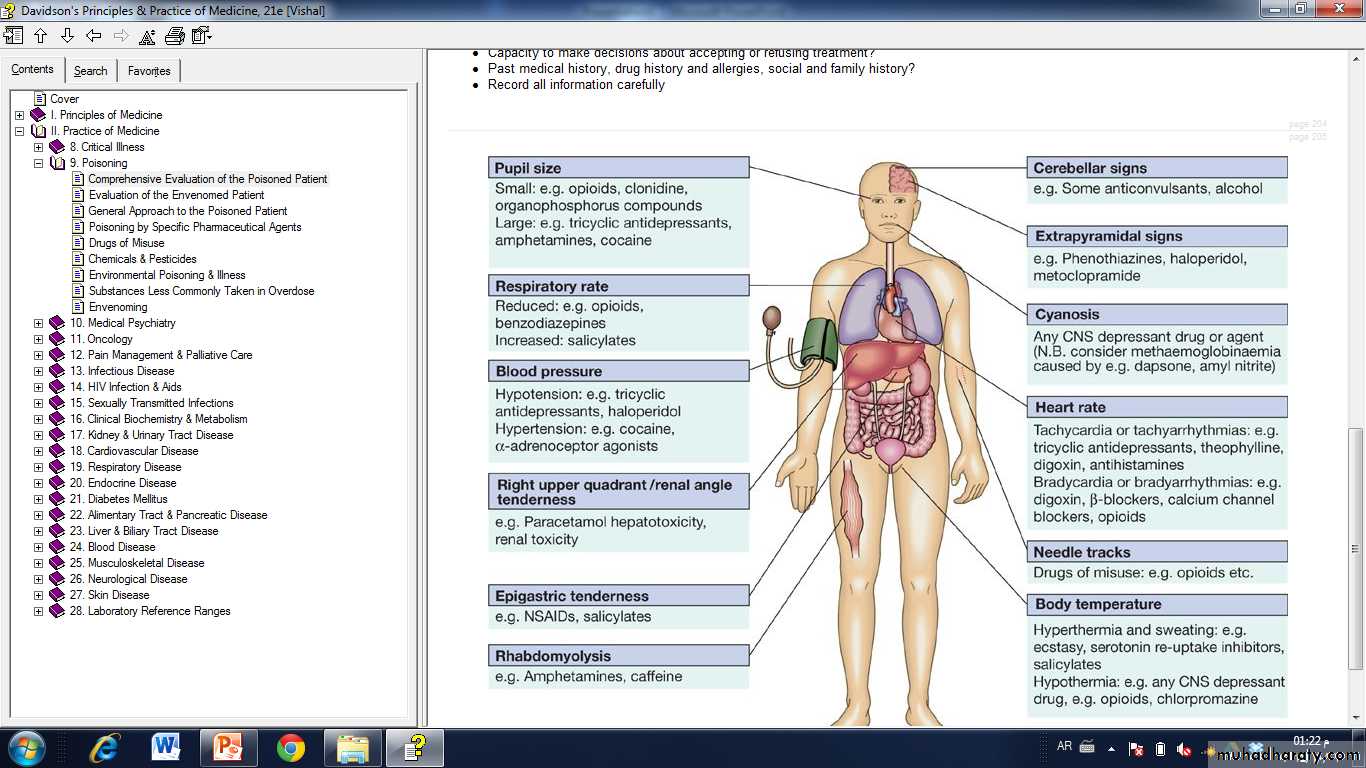
Clinical assessment and investigations
The patient may have a cluster of clinical features ('toxidrome') suggestive of poisoning with a particular drug typePoisoning is a common cause of coma, especially in younger people, but it is important to exclude other potential causes.
Serotonin syndrome
Anticholinergic
Stimulant
Sedative hypnotic
Opioid
Cholinergic muscarinic
Cholinergic nicotinic
Psychiatric assessment
Assess the risk of suicidal attempt
The use or abuse of certain psychotropic materials
Advice and treatment
General management
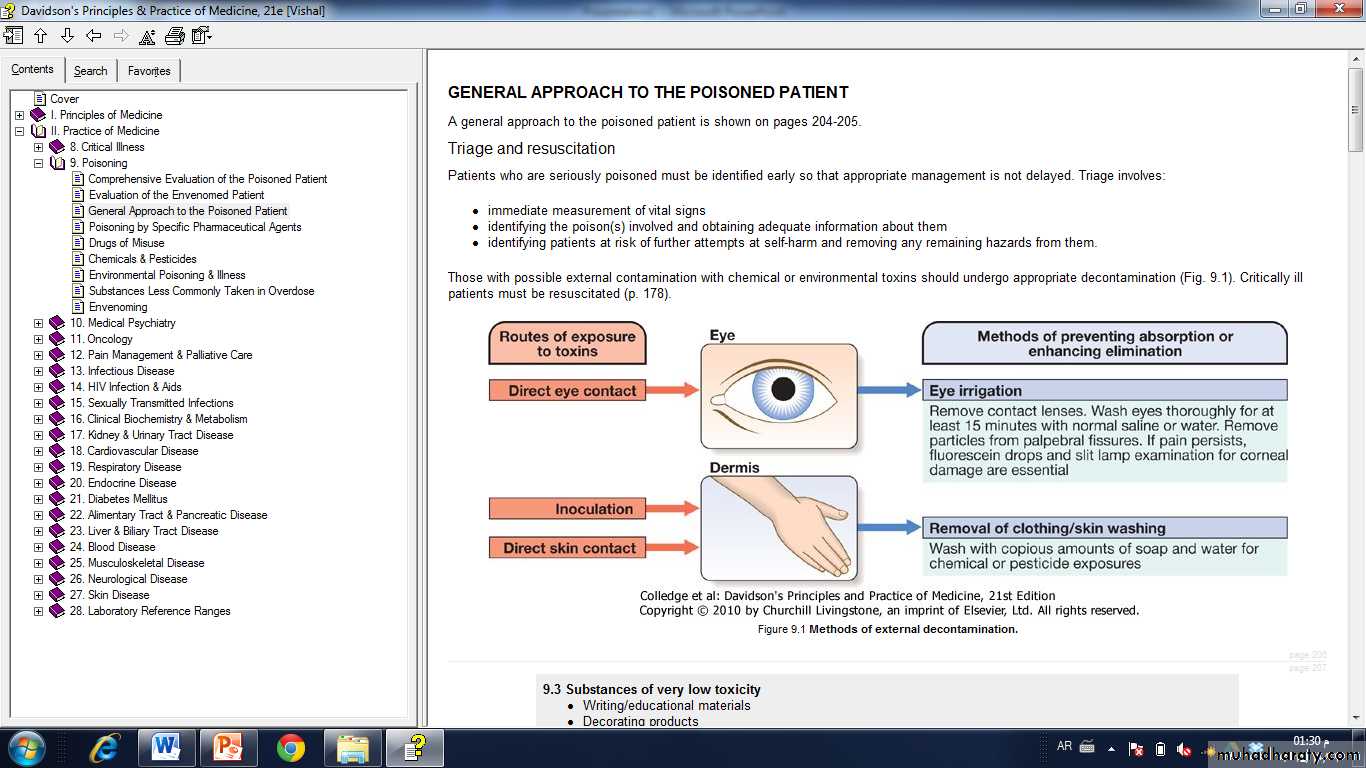
Patients presenting with eye or skin contamination should undergo appropriate local decontamination proceduresGastrointestinal decontamination
Patients who have ingested potentially life-threatening quantities of toxins may be considered for gastrointestinal decontamination if poisoning has been recent.
Induction of emesis using ipecacuanha is now never recommended.
Activated charcoal
Given orally as slurry, activated charcoal absorbs toxins in the bowel as a result of its large surface area. If given sufficiently early, it can prevent absorption of an important proportion of the ingested dose of toxin. However, efficacy decreases with time and current guidelines do not advocate use more than 1 hour after overdose in most circumstancesHowever, use after a longer interval may be reasonable when a delayed-release preparation has been taken or when gastric emptying may be delayed.
Some toxins do not bind to activated charcoal so it will not affect their absorption.
In patients with an impaired swallow or a reduced level of consciousness, the use of activated charcoal, even via a nasogastric tube, carries a risk of aspiration pneumonitis.
This risk can be reduced but not completely removed by protecting the airway with a cuffed endotracheal tube.
Substances poorly adsorbed by activated charcoal
MedicinesIron
Lithium
Chemicals
Acids*
Alkalis*
Ethanol
Ethylene glycol
Mercury
Methanol
Petroleum distillates*
* Gastric lavage contraindicated
Gastric aspiration and lavage
Gastric aspiration and/or lavage is now very infrequently indicated in acute poisoning, as it is no more effective than activated charcoal, and complications are common, especially aspiration. Use may be justified for life-threatening overdoses of some substances that are not absorbed by activated charcoal
Whole bowel irrigation
This is occasionally indicated to enhance the elimination of ingested packets or slow-release tablets that are not absorbed by activated charcoal (e.g. iron, lithium), but use is controversial. It is performed by administration of large quantities of polyethylene glycol and electrolyte solution (1-2 L/hr for an adult), often via a nasogastric tube, until the rectal effluent is clear.Contraindications include inadequate airway protection, haemodynamic instability, gastrointestinal haemorrhage, obstruction or ileus. Whole bowel irrigation does not cause osmotic changes but may precipitate nausea and vomiting, abdominal pain and electrolyte disturbances.
Urinary alkalinisation
Urinary excretion of weak acids and bases is affected by urinary pH, which changes the extent to which they are ionised.Highly ionised molecules pass poorly through lipid membranes and therefore little tubular reabsorption occurs and urinary excretion is increased.
If the urine is alkalinised (pH > 7.5) by the administration of sodium bicarbonate (e.g. 1.5 L of 1.26% sodium bicarbonate over 2 hrs), weak acids (e.g. salicylates, methotrexate and the herbicides 2,4-dichlorophenoxyacetic acid and mecoprop) are highly ionised and so their urinary excretion is enhanced. This technique should be distinguished from forced alkaline diuresis, in which large volumes of fluid with diuretic are given in addition to alkalinisation.
This is no longer used because of the risk of fluid overload.
Urinary alkalinisation is currently recommended for patients with clinically significant salicylate poisoning when the criteria for haemodialysis are not met (see below). It is also sometimes used for poisoning with methotrexate. Complications include alkalaemia, hypokalaemia and occasionally alkalotic tetany (p. 444). Hypocalcaemia is rare.
Haemodialysis and haemoperfusion
These can enhance the elimination of poisons that have a small volume of distribution and a long half-life after overdose, and are useful when the episode of poisoning is sufficiently severe to justify invasive elimination methods.The toxin must be small enough to cross the dialysis membrane (haemodialysis) or must bind to activated charcoal (haemoperfusion)
Haemodialysis may also correct acid-base and metabolic disturbances associated with poisoning.
Haemodialysis and haemoperfusion
These can enhance the elimination of poisons that have a small volume of distribution and a long half-life after overdose, and are useful when the episode of poisoning is sufficiently severe to justify invasive elimination methods.The toxin must be small enough to cross the dialysis membrane (haemodialysis) or must bind to activated charcoal (haemoperfusion)
Haemodialysis may also correct acid-base and metabolic disturbances associated with poisoning.
Poisons effectively eliminated by haemodialysis or haemoperfusion
Haemodialysis
Ethylene glycol
Isopropanol
Methanol
Salicylates
Sodium valproate
Lithium
Haemoperfusion
TheophyllinePhenytoin
Carbamazepine
Phenobarbital
Amobarbital
Antidotes
Antidotes are available for some poisons and work by a variety of mechanisms: for example, by specific antagonism (e.g. isoproterenol for β-blockers), chelation (e.g. desferrioxamine for iron) or reduction (e.g. methylene blue for dapsone).The use of some antidotes is described in the management of specific poisons below.