Dysplasia
Dysplasia is change of phenotype (size, shape and organization of tissue). This generally consists of an expansion of immature cells, with a corresponding decrease in the number and location of mature cells.Dysplasia is the earliest form of pre-cancerous lesion which pathologists can recognize in a pap smear or in a biopsy. it can be low grade or high grade.
The term dysplasia is typically used when the cellular abnormality is restricted to the originating tissue and does not invade past the basement membrane, as in the case of an early, in-situ neoplasm. Carcinoma in situ represents the transformation of a neoplastic lesion to one in which cells undergo essentially no maturation. In this state, epithelial cells have lost their tissue identity and have reverted back to a primitive cell form that grows rapidly and with abnormal regulation.
Of course, Invasive carcinoma is the final step in this sequence.
Dysplasia is characterized by four major pathological microscopic changes:
Anisocytosis (cells of unequal size)
Poikilocytosis (abnormally shaped cells)
Hyperchromatism (excessive pigmentation)
Presence of mitotic figures (an unusual number of cells which are currently dividing).
Metaplasia
Metaplasia (Greek: "change in form") is the reversible replacement of one differentiated cell type with another mature differentiated cell type that is more able to withstand the stresses it is faced with.
When cells are faced with physiological or pathological stresses (chronic physical or chemical irritation) they adapt by several ways, one of them is metaplasia. If the stimulus that caused metaplasia is removed, tissues return to their normal pattern of differentiation.
Thus metaplasia is not synonymous with dysplasia and is not directly considered carcinogenic.
Pap smear Technique and Interpretation
FREQUENCY OF SCREENING:
In USA the most recent recommendation is that first screen should be 3 years after the onset of sexual activity Or before age 21 (whichever comes first).
ACOG(American College of Obstetricians and Gynecologists) recommends annual Pap smear screening
American cancer society recommends every other year screening when using liquid – based cytology
After age 30, the interval between screening can be increased to 2-3 years .
More frequent i.e. annual Pap smears are recommended for women :
using DSEImmunocompromised
Previous history of stage 2 or 3 cervical intraepithelial neoplsia (CIN)
INTERPRETEATION OF RESULTS:
The Bethesda guidelines recommend that 8000—12,000 squamous cells be obtained for conventional Pap smear but only 5000 cells for a liquid- based sample.Cells can obscured by blood , mucous and inflammatory cells. If more than 75% of the cells are obscured, the sample is inadequate and a new sample must be tested.
The presence of endocervical cells (at least 10) is required from women older than 40 but it is not mandatory in those younger than 40 years of age.
The pap smear can reveal one of the following:
Negative result: meaning the cells are normal
NILM: negative for intraepithelial lesion or malignancy
Atypical Squamous cells (ASC):
The Bethesda guidelines emphasize the ability to distinguish between HSIL and LSIL. Overall it is thought that 10 – 30% of women with a finding of ASC on a Pap smear have underlying CIN grade 2 or 3, and 0.1% may have invasive cancer.
ASC falls into two different categories:
Atypical Squamous cells of Undetermined Significance (ASC-US): It is estimated that 90 - 95% of all finding of ASC fall into this category of ASC-USWomen with a Pap smear result of ASC-US have a 5 -7% chance of currently having CIN 2 and 3. On the other hand, 39% of women with CIN 2 or 3 have a previous finding of ASC-US on Pap smear.
ASC-US is associated with HPV in about 33 - 67% of cases.
ASC-H: The category of ASC-H describes atypical cells that are morphologically suspicious of HSIL but too few in number to be considered an HSIL .
ASC-H is more highly associated with HSIL than ASC-US and is the most common precursor lesion for CIN. Follow up of women with a finding of ASC-H leads to diagnosis of CIN 2 & 3 in 68%.
Atypical Glandular Cells (AGC): These cells are further subdivided according to whether they are: Endocervical, Endometrial, Or not otherwise specified.
Finding AGC is relatively rare, occurring in 0.17- 1.8% of all Pap smears. However, the presence of these cells has serious medical implications because women with a finding of AGC have 9.7 times higher risk of progressing to CIN 2.
AGC favoring neoplasia: This finding may correspond with high-grade lesions on tissue examination (27-96% of the time)
Adenocarcinoma in situ (AIS): It corresponds with high rates of advanced lesions on tissue examination.
Low-grade and High grade squamous intraepithelial lesion (LSIL and HSIL): Studies have shown that the finding of LSIL is more variable and less reproducible than HSIL and repeatable in only 80% of smears. Bethesda guidelines further specify (with features suspicious of invasion) when histological evidence supporting cancer is present.
COUNSELING WOMEN WITH ABNORMAL PAP SMEAR
Women with abnormal Pap smear findings should be counseled that HPV infection has been linked with the development of cervical cancer, and that HPV is the most common viral STD, affecting up to 70% of the sexually active population.Uterine fibroid (Uterine leiomyoma)
is a benign tumor composed of uterine muscles plus fibrous connective tissue. It is common and present in 20% of all females. It is more in Negros than in white womenIt is of unknown cause and may be found outside the uterine organs (Vagina, broad ligament, vulva)
Female sex hormones have been incriminated as a cause because it rarely appears before puberty and after menopause. In addition, there is a rapid growth during pregnancy, and is frequently seen in conditions associated with hyperestrogenism that are not antagonized by progesterone like anovulation, endometrial Polyps, and endometrial hyperplasia.
Grossly: It is a firm round tumor of hypertrophied uterine wall. It has a pseudo capsule which differentiates it from adenomyosis. Since its blood supply is peripheral, the center is susceptible to degenerative changes.
Cross section of the tumor reveals a solid, smooth, pinkish or white surface with whorl- like appearance.
Microscopically: It is composed of groups & bundles of smooth muscles in a twisted whorl fashion, with some connective tissue .
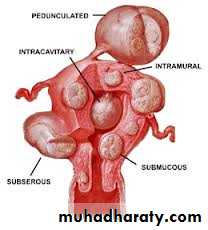
Types:
Intramural (the commonest)
Sub serous myomas: projecting towards the peritoneal cavity ± pedicle may reach a large size without producing symptoms
Interligamentory tumor
Sub mucosal
Cervical
Fibroids may be single or multiple
The clinical presentation depends on the size, number and location of the fibroid and could be one of the following:
Symptomless: discovered accidentally.
Abnormal uterine bleeding: heavy and prolonged.
It may be due to enlargement of uterine cavity by submucous fibroids, increased vascularity of the tumor, or due to necrosis of endometrium overlying the submucous myoma. Frequently, myomas may be associated with polyps and endometrial hyperplasia.
Inter menstrual bleeding in case of submucus fibroid
pain
reappearance of dysmenorrhea (congestive type) due to increase vascularity
Backache incase of posterior fibroids of moderate size with retroversion
Colicky pain in case of sub mucous uterus
can be caused by torsion
Degenerative changes
Abdominal distention
Pressure symptoms which include:
edema due to pressure on vena cava
urinary frequency due to pressure on bladder
dyspnea
Degenerative changes of uterine fibroids:
Occur due to arterial, venous, secondary infections or malignant transformation. There are several types:
Hyaline degeneration:
Here the tumor becomes soft and jellylike, the cells fuse together and form a structureless esonophilic mass.
Cystic degeneration: Liquefaction may occur after menopause leading to cystic cavity formation.
Red degeneration (Necrobiosis): could be diffuse or local. Usually occurs in pregnancy or near menopause that leads to a fibromyomatous pattern.
Pathology: There is thrombosis of peripheral vessels with absence of cell nuclei. The blood vessels are distended with thin wall and are engorged with R.B.C.s. Thus the tumor is stained red and resembles raw meat.
It gives a fishy odor on cutting due to presence of fatty acids. Cystic degeneration may occur in the center and the cyst becomes full with greasy brown debris.
Fatty degeneration
Calcifications: Fat may be deposited in fibroid which undergoes saponification. Co3 and Po4 in blood react with the soppy mass leading to deposition of CaCo3 and calcium phosphate
Grossly: It has a gritty appearance on cross section
A thin peripheral shell can be seen by X -ray
In addition to degenerative changes, complications of fibroids include:
Sarcomatous (malignant) changes Sarcomatous changes that occur in 0.5% of fibroids, 2/3 of sarcoma of the uterus arise from uterine fibroids.Necrosis
Infection
Atrophy
Torsion
Differential diagnosis (of an abdominal mass)
Pregnancy
Ovarian tumor
Endometrial or cervical polyp
Adenomyosis
Treatment
Conservative for small and asymptomatic fibroid.Frequent U/S every 6 months.
LH RH agonist
Surgical
Myomectomy either by laparotomy or laparoscopy
Hysterectomy
Uterine artery embolisation
Endometrial hyperplasia:
Endometrial hyperplasia is when the endometrium becomes too thick. It is not cancer but it can lead to cancer formation in some cases.
Etiology:
Endometrial hyperplasia most often is caused by excess estrogen without progesterone. If ovulation does not occur, progesterone is not made, and the lining is not shed. The endometrium may continue to grow in response to estrogen. The cells that make up the lining may crowd together and may become abnormal (This is called Hyperplasia).
Factors predisposing to endometrial hyperplasia:
Postmenopausal women, when ovulation stops and progesterone is no longer made. It can also occur during perimenopause, when ovulation may not occur regularly.
Long-term use of high doses of estrogen after menopause (in women who have not had a hysterectomy) or estrogen like drugs.
Irregular menstrual periods, especially associated with polycystic ovary syndrome or infertility
Other risk factors include:
Age older than 35 years
White race
Never having been pregnant
Early onset of menarche
Personal history of certain conditions, such as diabetes mellitus, polycystic ovary syndrome, gallbladder disease, or thyroid disease
Cigarette smoking
Family history of ovarian, colon, or uterine cancer
Obesity
Types of endometrial hyperplasia
Endometrial hyperplasia is classified as simple or complex. It is also classified by whether certain cellular changes are absent or present as typical or atypical respectively. These terms are combined to describe the exact kind of hyperplasia:
Simple hyperplasia
Complex hyperplasia
Simple atypical hyperplasia
Complex atypical hyperplasia
Clinical presentation:
The most common sign of hyperplasia is abnormal uterine bleeding.Bleeding during the menstrual period that is heavier or lasts longer than usual
Menstrual cycles that are shorter than 21 days (counting from the first day of the menstrual period to the first day of the next menstrual period)
Any bleeding after menopause
Diagnosis:
Transvaginal ultrasound may be done to measure the thickness of the endometrium.Endometrial biopsy, dilation and curettage, or hysteroscopy is done in cases suspicious of malignancy.
Treatment:
many cases are treated with Progestin (orally, in an intrauterine device, or as a vaginal cream). Duration of treatment depends on the age of the patient and the type of hyperplasia.Treatment with progestin may cause vaginal bleeding resembling menstruation.
If there is atypical hyperplasia, especially complex atypical hyperplasia, there is an increased of cancer so Hysterectomy is done. It is the best option for those who do not want to conceive.
Prevention of endometrial hyperplasia:
Estrogen treatment after menopause should be combined with progestin or progesterone.
If there is irregular menstrual period combined oral contraceptive pills may be recommended.
Decrease weight if obese.