Skin tumors
Benign epidermal tumorsPremalignant epidermal tumours
Malignant epidermal tumours
Tumours of the dermis
Benign epidermal tumors
Seborrhoeic keratosisun-related to sebaceous glands. Usually arise after the age of 50 years. multiple but may be single. common on the face and trunk.
distinctive ‘stuck-on’ appearance. flat, raised, filiform or pedunculated. Surface smooth or verrucous. yellow–white to dark brown–black.
ugly or easily traumatized ones can be removed with a curette, or by cryotherapy.
Skin tags (acrochordon)
common benign outgrowths of skinSkin tags are most common in obese women
around the neck and within the major flexures.
look unsightly, catch on clothing and jewellery.
soft skin-coloured or pigmented pedunculated papules.
Small lesions can be snipped off with fine scissors, frozen with liquid nitrogen or destroyed with electrodessication.
Naevi
skin lesion that has a localized excess of one or more types of cell in a normal cell site.may be composed mostly of
keratinocytes
melanocytes
connective tissue elements
mixture of epithelial and connective tissue
Linear epidermal naevus follow Blaschko’s lines. Keratinocytes in these lines appear as wart-like growth
Keratolytics lessen the roughness
small epidermal naevi may be excised.
Melanocytic naevi localized benign tumours of melanocytes.
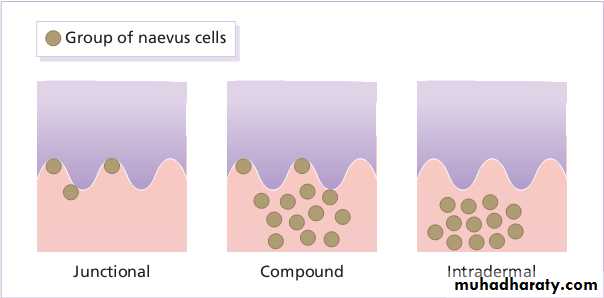
The ‘junctional’ type (proliferating melanocytes in clumps at the dermo-epidermal junction).A ‘compound’ naevus has both dermal and junctional components.
the melanocytes in an‘intradermal’ naevus are all in the dermis.
Spitz naevi develop over a month or two as solitary pink or red nodules up to 1 cm in diameter, common on the face and legs. Benign, excision is best.
Blue naevi striking grey–blue color, appear on the limbs, buttocks and lower back. usually solitary.
Mongolian spots Pigment in dermal melanocytes , bruise-like greyish areas seen on the lumbosacral area of most Down’s syndrome and many Asian and black babies. They usually fade during childhood.
Sebaceous naevus A flat hairless area at birth, usually in the scalp, become more yellow and more raised at puberty. Risk of basal cell carcinomas in adult life.
Malignant change should be considered if the following changes occur in a melanocytic naevus: Enlargement, increased or decreased pigmentation, altered shape, altered contour, inflammation, ulceration, itch, or bleeding.
Excision is needed when:
naevus is unsightly;
malignancy is suspected
risk as large congenital melanocytic naevus
naevus repeatedly inflamed or traumatized.
Epidermoid and pilar cysts Common and occur on the scalp, face, behind ears, trunk. often have a central punctum.
The lining of a cyst resembles normal epidermis (an epidermoid cyst) or the outer root sheath of the hair follicle (a pilar cyst).
excision
incision followed by expression of contents + removal of the cyst wall.Milia
small subepidermal keratin cysts. common on face in all age groups. appear as tiny white papules of 0.5 –2 mm. contents of milia can be picked out with a sterile needle.Premalignant epidermal tumours
Actinic keratoses discrete rough-surfaced pink or grey scaling macules or papules usually less than 1 cm in diameter appear on sun-damaged skin, middle-aged and elderly.The effects of sun exposure are cumulative.
Their rough surface better felt than seen.
Transition to an invasive squamous cell carcinoma, if enlarges, becomes nodular, ulcerates, bleeds.
Freezing with liquid nitrogen effective. Shave removal or curettage for large lesions
Multiple lesions treated with 5-fluorouracil, Imiquimod, 3% Sodium diclofenac gel.Malignant epidermal tumours
Basal cell carcinoma (rodent ulcer) most common, appear on faces of elderly. Prolonged sun exposure main factor. destroys tissue locally.Nodulo-ulcerative small glistening translucent, skin-coloured papule. Central necrosis leaves an ulcer with an adherent crust and a rolled pearly edge. Coarse telangiectatic vessels run across surface.
Excision with 0.5 cm of surrounding normal skin. Radiotherapy.Cryotherapy, curettage, cautery . photodynamic therapy for superficial lesions.
Squamous cell carcinoma
ultraviolet radiation, X-rays and chronic inflammation.DNA of human papilloma virus
may arise as thickenings in an actinic keratosis or, de novo, as small scaling nodules; rapidly growing lesions
may start as ulcers with a granulating base and an indurated edge.
common on the lower lip, in the mouth.
Tumours more than 2 cm in diameter greater than 4 mm in depth, poorly differentiated; perineural involvement; immunosuppresion more likely to metastasize.
low-risk tumours should be excised with a 0.5-cm border of normal skin. Wider excision (6 mm or more) is recommended for high-risk tumours. Palpation of regional nodes is important in work-up . Radiotherapy is effective.
Intra-epidermal squamous cell carcinoma
Bowen’s disease Usually single, these slowly expanding pink scaly plaques. Their border is sharply defined, with reniform projections and notches giving them an amoeboid shape.3% progress into squamous cell carcinoma.
Cryotherapy or curettage are the treatments of choice for small lesions on face or trunk
excision is an alternative. Photodynamic therapy useful for large lesions on lower legs.
Topical 5-fluorouracil , imiquimod helpful for multiple lesions.
Keratoacanthomatous squamous cell carcinoma
occur mainly on the exposed skin of fair individuals. More than two-thirds are on the face and most of the rest are on the arms.The lesion starts as a pink papule that rapidly enlarges. After 5 – 6 weeks the centre of the nodule forms either a keratinous plug or a crater.
lesion may resolve spontaneously over 6–12 months leaving an ugly depressed scar.
Excision, curettage and cautery are both effective.
Malignant melanoma
Genetic SusceptibilitySunlight
Pre-existing melanocytic naevi
Eighty percent of invasive melanomas are preceded by a superficial and radial growth phase, shown clinically as the expansion of an irregularly pigmented macule or plaque. Most are multicoloured mixtures of black, brown, blue, tan and pink. reniform projections and notches.
Lentigo maligna melanoma on exposed skin of elderly. An irregularly shaped pigmented macule (a lentigo maligna)
Superficial spreading melanoma in Caucasoids.
Acral lentiginous melanoma on palms and soles
Nodular melanoma appears as a pigmented nodule with no preceding n situ phase. rapidly growing and aggressive type.
Subungual melanomas painless areas of pigmentation expanding under nail,onto the nail fold (Hutchinson’s sign).
An excision biopsy, with a 2–5 mm margin of clearance laterally and down to the subcutaneous fat, is recommended for all suspicious lesions.
If the histology confirms the diagnosis of malignant melanoma then wider excision, including the wound of the excision biopsy. A minimum of 0.5 cm clearance for melanomas in situ and 1 cm clearance is required for all invasive melanomas.
If lymph node involvement is suspected fine needle aspiration done. If involvement is confirmed then block dissection of involved group of nodes.
Chemotherapy may be palliative
Tumours of the dermis Benign dermal tumours
Malformations1.Salmon patches (‘stork bites’) present in 50% of all babies, caused by dilatated capillaries in superficial dermis. dull red, often telangiectatic macules,on the nape of the neck, the forehead and the upper eyelids.
Nuchal lesions may remain
unchanged, patches in other
areas usually disappear in a year.
2. Port-wine stains present at birth, caused by dilatated dermal capillaries. pale, pink–purple macules on face or trunk. They persist, in middle age may darken and become studded with angiomatous nodules. flash lamp-pumped pulsed dye laser, sessions can begin in babies.
3.Haemangiomas
Capillary cavernous haemangioma appear within a few weeks of birth and grow for a few months, forming a raised compressible swelling with a bright red surface.Spontaneous regression then follows
Bleeding follow trauma, ulceration in napkin area.
Observation and encouragement.. If lesions ulcerate, bleed repeatedly, interfere with feeding or with vision, high doses of systemic steroids successful in proliferative phase.
pulsed dye lasers for large lesions in infancy.
cherry angiomas common on the trunks of the middle-aged and elderly. They are small bright red papules and of no consequence.
Lymphangiomas lymphangioma circumscriptum appears as a cluster of vesicles resembling frog spawn. Excision wide and deep.
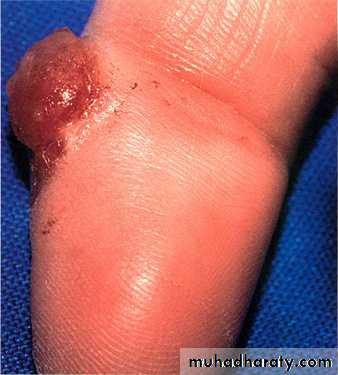
Pyogenic granulomas common benign acquired haemangiomas. develop at sites of trauma, over course of a few weeks, as bright red raised, raspberry-like lesions which bleed easily. removed by curettage under local anaesthetic with cautery to the base.
Dermatofibromas
benign tumours are firm, discrete, usually solitary dermal nodules, on extremities of young adults.Iceberg effect in that they feel larger than they look.
The overlying epidermis is often lightly pigmented and dimples when the nodule is squeezed.
may follow minor trauma or an insect bite.
It should be excised.
Lipomas common benign tumours of mature fat cells in subcutaneous tissue. single or many.
common on proximal limbs,can occur at any site. irregular lobular shape,soft rubbery consistency,rarely painful.
removed only doubt about diagnosis, painful, unsightly or interfere with activities
Cutaneous T-cell lymphoma ( mycosis fungoides)
usually evolves slowly.three clinical phases: the patch, plaque,tumour
The patch stage may last for years, consists of scattered, erythematous, slightly pigmented, sharply marginated, scaly patches.
some patches become indurated and palpable: the plaque stage.
Some then turn into frank tumours which may become large (occasionally like mushrooms, hence the term ‘mycosis fungoides’) and ulcerate.
Topical steroids, and UVB treatment, in the patch stage.
In the plaque stage, psoralen with ultraviolet A (PUVA), oral retinoids,α-interferonIndividual tumours respond well to low-dose radiotherapy.
Systemic chemotherapy is disappointing.