1
Fifth stage
Medicine
Lec-7
د.فاخر
22/12/2015
Osteoarthritis
(OA) is the most common form of arthritis. It has a strong
relation with ageing as it's a major cause of pain and disability
in older people
is characterised by focal loss of articular cartilage, subchondral
osteosclerosis, osteophyte formation at the joint margin, and
remodelling of joint contour with enlargement of affected
joints.
Prevalence
• Females are more commonly affected except that hips OA occurs equally in both sexes
• By age of 65, 80% of people have radiological OA 25-30% of them are symptomatic
• The knee and hip are the principal large joints involved, affecting 10-25% of those aged
over 65 years. Even in joints less frequently targeted by OA, such as the elbow,
.glenohumeral joint
Risk Factors
Increasing age
“excessive” joint loading & mobility
Abnormal mechanical forces (e.g. varus & valgus knee deformities)
female sex
Genetic predisposition
Obesity (for knees & hands O.A.)
Muscle weakness
Prior joint disease

2
Pathology
Stages of cartilage loss
• Superficial fissuring (fibrillation)
• Erosions & deep ulcers
• Thinning & hypo-cellularity
• Areas of repair with fibrocartilage
Bone Changes
• Subchondral sclerosis
• Osteophytes
• Subchondral cysts
• Remodeling (shape changes)
Clinical features
Pain
Insidious onset over months or years
Variable or intermittent over time (‘good days, bad days’)
Mainly related to movement and weight-bearing, relieved by rest
Only brief (< 15 mins) morning stiffness and brief (< 5 mins)
‘gelling’ after rest
Usually only one or a few joints painful
Clinical signs
Restricted movement due to capsular thickening, or blocking by osteophyte
Palpable, sometimes audible, coarse crepitus due to rough articular surfaces
Bony swelling around joint margins
Deformity, usually without instability
3
Joint-line or periarticular tenderness
Muscle weakness and wasting
Synovitis mild or absent
Clinical Patterns
Localized interphalangeal OA. (usually DIP)
Generalized OA.
Loading / mobility related OA.
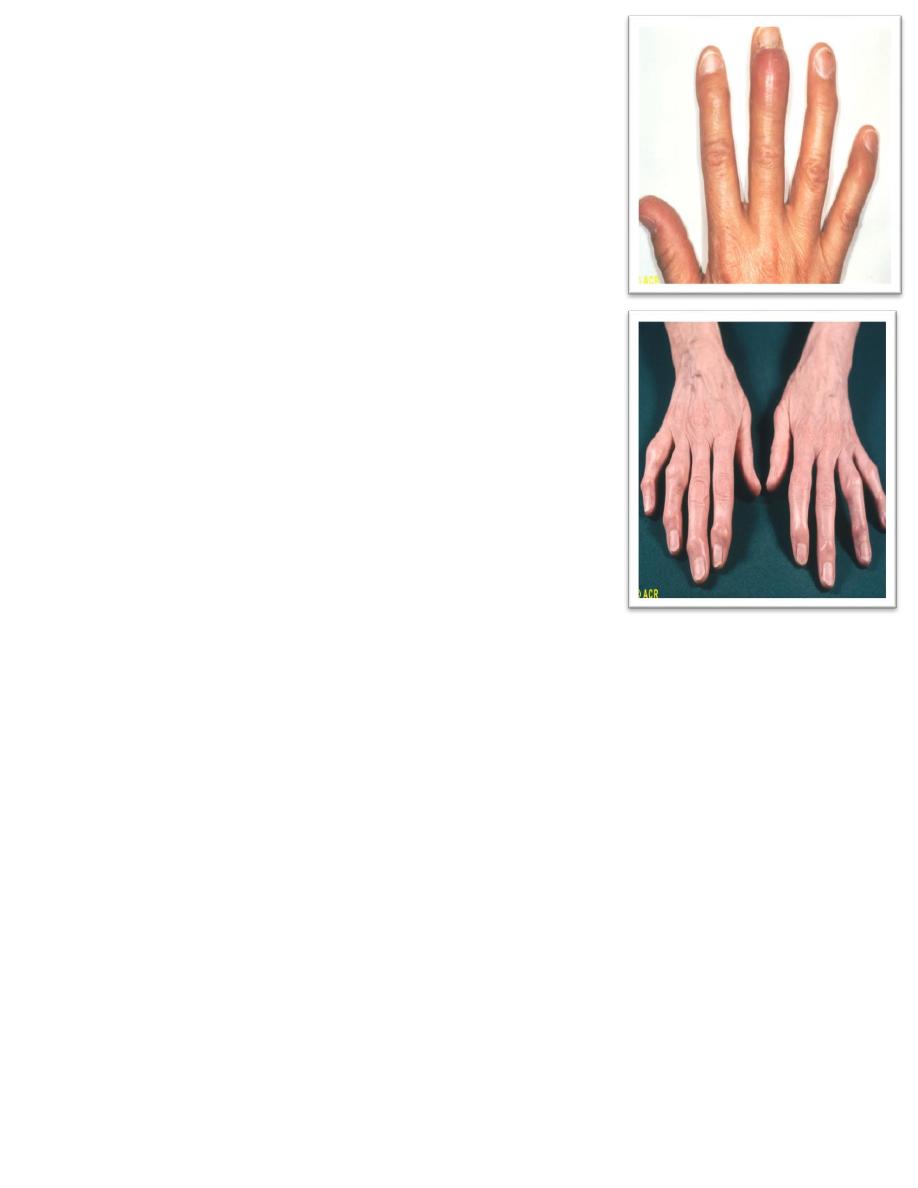
Osteoarthritis: Heberden’s nodes, inflammation
Localized interphalangeal OA. (usually DIP)
• Heberden’s nods appears slowly
• Female & male 10/1
• Strong genetic factor
Osteoarthritis: Heberden’s and Bouchard’s nodes
Generalized OA
• Usually post menopausal women
• Affect 3 or more joints or joints group
• Usually starts in the interphalangeal joints (DIPs & PIPs)
• Tendency to O.A. at other sites specially knee
Investigations
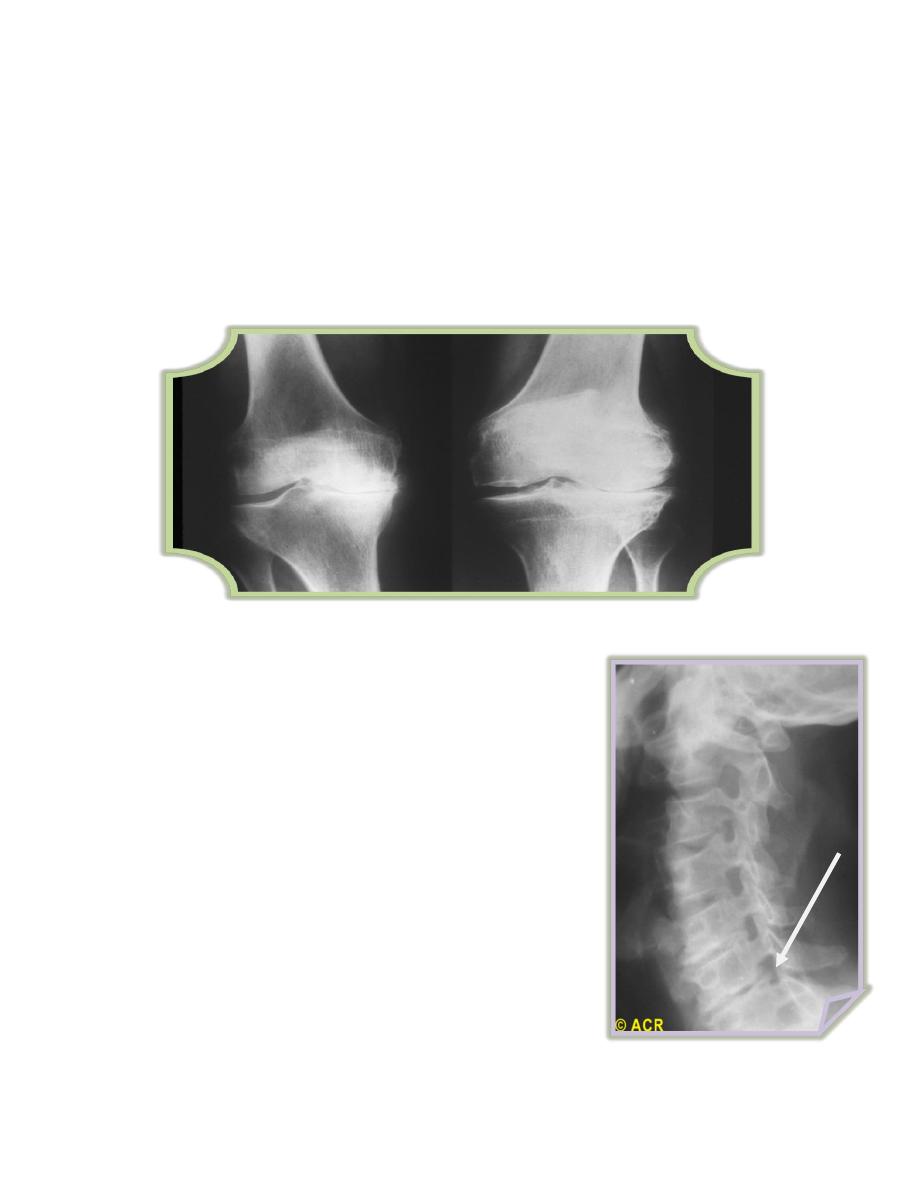
XR findings
Joint space narrowing
Subchondral sclerosis
Osteophyts
Subchondral cysts
4
Deformity contour, slipping XR patient position
Hip : non-weight bearing film
Knee : standing (stressed) AP film
Patellofemoral : flexed skyline view
Osteoarthritis: knees, medial (XR1) and lateral (XR2) cartilage degeneration (Medial loss is the
usual in mobility / loading related O.A. knee)
Osteoarthritis: cervical vertebrae, foraminal encroachment
XR1 =>
<= XR2
5
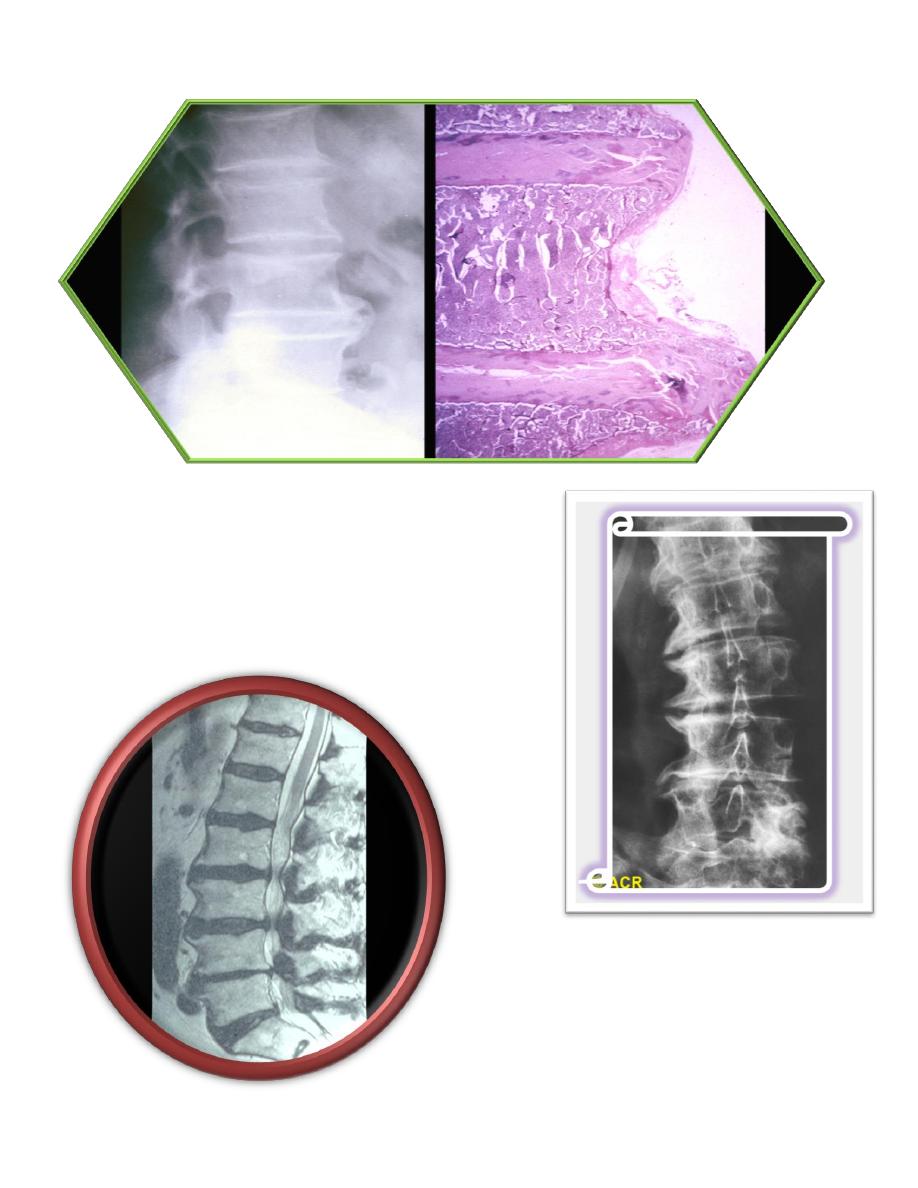
Lumbar vertebrae, osteophytes (radiograph and photomicrograph)
Osteoarthritis: lumbar vertebrae, advanced stages
Spinal stenosis: lumbar spine (MRI) due to O.A.

6
Treatment
• Non pharmacological Reduce obesity
• Avoid static loading e.g. prolonged squatting
• Pacing of activity
• Exercise specially non weight bearing (bicycle …)
• Joint rest techniques :Neck collar
Pharmacological
Oral analgesic : paracetamol
Topical : capsacin & NSAIDs
Systemic NSAIDs
Intra-articular steroids with careful precautions
Intra-articular hyaluronic acid products
Glucosamine & chondroitins sulfate
Surgical
Osteotomy
Total joint replacement (TJR)
Cartilage repair surgery (cartilage auto-graft). Highly specialized centers
Indications : uncontrolled pain & functional disability refractory to conservative therapy
