Terminology
Periodontiumis a functional system of different tissues, investing and supporting the teeth, including cementum, periodontal ligaments, alveolar bone and gingiva. The main function of the periodontium is to attach the tooth to the bone tissue of the jaws and to maintain the integrity of the surface of the masticatory mucosa of the oral cavity
Periodontology
is the fundamental dental science that deal with scientific study of the periodontium in health and disease.Periodontics
is that branch of dentistry that deals with diagnosis and treatment of diseases and condition of the supporting and surrounding tissues of the teeth or their implanted substitutes.GINGIVA:
The gingiva is that part of the masticatory mucosa which covers the alveolar process and surrounds the cervical portion of the teeth. It consists of an epithelial layer and an underlying connective tissue layer called the lamina propria.The oral mucosa (mucous membrane) is continuous with the skin of the lips and the mucosa of the soft palate and pharynx. The oral mucosa consists of:
(1)The masticatory mucosa, which includes the gingivaand the covering of the hard palate,
(2) The specializedmucosa, which covers the dorsum of the tongue,
(3) The remaining part, called the lining mucosa.
Figure (1-1): The gingiva (G), the periodontal ligament (PL), the root cementum (RC), and the alveolar bone (AP). The alveolar bone consists of two components, the alveolar bone proper (ABP) and the alveolar process
Clinical features:
The gingiva is divided anatomically into marginal, attached, and interdental areas.
Marginal Gingiva: or (unattached gingiva) is the terminal edge or border of the gingiva surrounding the teeth in collar like fashion.
Free gingival groove: a shallow linear depression, about 1 mm in width, it separate the marginal gingiva from attached gingiva. It forms the soft tissue wall of the gingival sulcus. It may be separated from the tooth surface with a periodontal probe.
Gingival sulcus: is the shallow crevice or space around the tooth bounded by the surface of the tooth on one side and the epithelium lining the free margin of the gingiva on the other. It has a V shape. Probing depth of a clinically normal gingival sulcus in humans is 2 to 3 mm.
Attached Gingiva: It is firm, resilient, and tightly bound to the underlying periosteum of alveolar bone. The facial aspect of the attached gingiva extends to the relatively loose and movable alveolar mucosa, from which it is demarcated by the mucogingival junction.
The width of the attached gingiva is the distance between the mucogingival junction and the projection on the external surface of the bottom of the gingival sulcus or the periodontal pocket.
width of the keratinized gingiva also includes the marginal gingiva
The width of the attached gingiva is generally greatest in the incisor region and less in the posterior segments.
least width in the first premolar
The width of the attached gingiva increases with age and in supraerupted teeth.
Figure (1-2): Diagram showing anatomic landmarks of the gingiva
- On the lingual aspect of the mandible, the attached gingiva terminates at the junction with the lingual alveolar mucosa, which is continuous with the mucous membrane lining the floor of the mouth. The palatal surface of the attached gingiva in the maxilla blends with the equally firm, resilient palatal mucosa.
C-Interdental Gingiva: It occupies the gingival embrasure; it can be pyramidal or have a "col" shape. In the former, the tip of one papilla is located immediately beneath the contact point.
Gingival embrasure: is the interproximal space beneath the area of tooth contact.
The shape of the gingiva in a given interdental space depends on:
The contact point between the two adjoining teeth.
The presence or absence of some degree of recession.
Figure (1-3): Diagram comparing anatomic variations of the interdental col in the normal gingiva (left side) and after gingival recession (right side). A, B, Mandibular anterior segment, facial and buccolingual views, respectively.C, D, Mandibular posterior region, facial and buccolingual views, respectively. Tooth contact points are shown in B and D
1.2. Microscopic features:
Gingival Epithelium:
The gingival epithelium is stratified squamous epithelium which is supported by fibrous connective tissue which is called lamina properia. The epithelium covering the gingiva may be differentiated as follows:
Oral epithelium which faces the oral cavity.
Oral sulcular epithelium which faces the tooth without touching it.
Junctional epithelium which provides the contact between the gingiva and the tooth surface.
Figure (1-4) the composition of the gingiva and the contact area between the gingiva and the enamel (E).
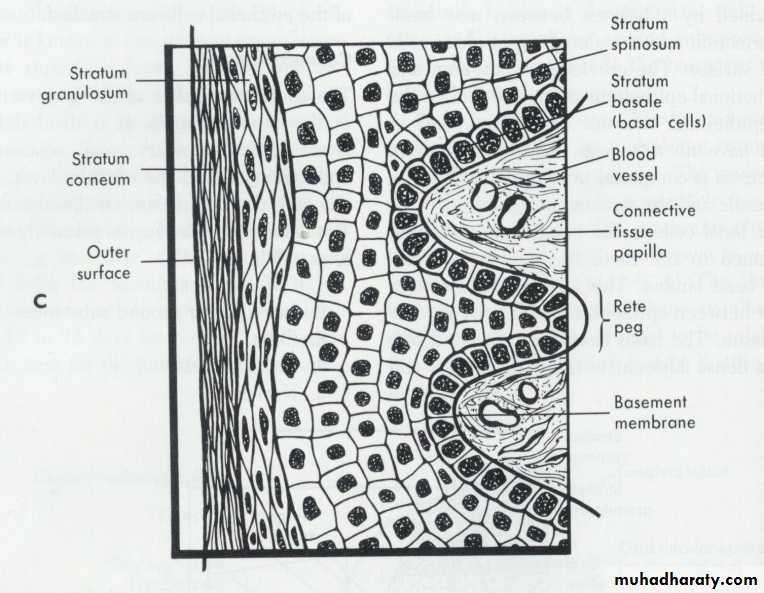
The boundary between the oral epithelium (OE) and the underlying connective tissue (C.T.) has a wavy course. The C.T. portions project into the epithelium are called C.T. papillae and are separated from each other by epithelial ridges- so- called rete pegs.
In normal non-inflamed gingiva, rete pegs and C.T. papillae are lacking at the boundary between J.E. and its underlying C.T. So that, a characteristic feature of the O.E. and the O.S.E. is the presence of rete pegs, while these structures are lacking in J.E.
- The oral epithelium is a keratinized stratified squamous; epithelium can be divided into the following:
1) Stratum basale.
2) Stratum spinosum.
3) Stratum granulosum.
4) Stratum corneum.
In the outer cell layers the nuclei are lacking. Such an epithelium is called Orthokeratinized, but often the cells of stratum corneum of human masticatory mucosa contain remnants of nuclei and in such a case the epithelium is denoted Parakeratinized.
Other cells of OE:
In addition to previously mentioned keratin producing cells which comprise about 90% of total cells population there are three types of cells
Melanocytes: pigment producing cells.
Langerhans cells: play a role in defense mechanism.
Non-specific cells: form other types of cells.
All the 3 types of cells are stellate and lighter in color than keratinocytes so they are called (clear cells).
The epithelial cells are attached to each other by numerous desmosomes (pairs of hemidesmosomes), and the basal layer is attached to the underlying basement membrane also by hemidesmosomes. The presence of large number of desmosomes indicates that the adhesion between the epithelial cells is solid.
The composition of desmosomes:
A desmosome consists of two adjoining hemidesmosomes separated by a zone containing electron-dense granulated material (GM), and a hemidesmosome comprises the following structural components:
1) The outer leaflets (OL) of the cell membrane of two adjoining cells.
2) The thick inner leaflets (IL) of the cell membrane.
Figure (1-6): A desmosome can beconsidered to consist of two adjoining hemidesmosomes separated by a zone containing electrondensegranulated material (GM).Thus, a desmosome comprises the following structural components: (1) the outer leaflets (OL) of the cell membrane of two adjoining cells, (2) the thick inner leaflets (IL) of the cell membranes and (3) the attachment plaques (AP), which represent granular and fibrillar material in the cytoplasm.
3) The attachment plaques (AP), which represent granular and fibrillar material in the cytoplasm.