
Dr. Firas Al-Obaidi
Surgery
Bone and Joint Infections
GENERAL ASPECTS OF INFECTION
I.
Acute haematogenous osteomyelitis
I.
AETIOLOGY
II. PATHOGENESIS
III. PATHOLOGY
IV. MANAGEMENT AND COMPLICATIONS
II. Chronic osteomyelitis
I.
AETIOLOGY
II. PATHOGENESIS
III. PATHOLOGY
IV. MANAGEMENT AND COMPLICATIONS
Infection:
is a condi)on in which pathogenic organisms mul)ply and spread within
the body )ssues.
This usually gives rise to an acute or chronic inflammatory reac)on , which is
the body s way of comba)ng the invaders and destroying them , or at least
immobilising them to a single area.
*
Bone infection differs from soft-tissue infection , since bone consists of a
collection of rigid compartments , it is more susceptible than soft tissues to
vascular damage and cell death from the build-up of pressure in acute
inflammation.
Host susceptibility to infection is increased by:
1- Local factors:
e.g. trauma , scar )ssue , poor circula)on , foreign body , and
chronic bone or joint disease.
2- Systemic factors:
e.g. Malnutri)on , general illness , diabetes , rheumatoid
disease , cor)costeroid usage and all forms of immunosuppression ( acquired or
induced) , and age factor.
Page of
1
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
*
Bacterial colonization and resistance to antibiotics is enhanced by the ability
of certain microbes (including Staphylococcus) to adhere to avascular bone
surfaces and foreign implants , protected from both host defences and
antibiotics by a protein –polysaccharide slime (glycocalyx).
The principles of treatment are:
1
-to provide analgesia and general suppor)ve measures.
2
-to rest the affected part.
3-
to iden)fy the infec)ng organism and administer effec)ve an)bio)c
treatment.
4-
to release pus as soon as it is detected.
5-
to stabilize the bone if it has fractured.
6-
to eradicate avascular and necro)c )ssue.
7-
to restore con)nuity if there is a gap in the bone.
8-
to maintain soL
)ssue and skin cover.
Acute haematogenous osteomyelitis
AETIOLOGY
1.
Acute haematogenous osteomyelitis is mainly a disease of children. When
adults are affected it is usually their resistance is lowered.
2.
Trauma may determine the site of infection , possibly by causing a small
haematoma or fluid collection in a bone , in a patients with concurrent
bacteraemia.
3.
The causal organism in both adults and children is usually Staphylococcus
aureus ( over 70 % of cases ).
4.
Less often one of the other Gram- positive cocci , e.g. Streptocccus pyogenes ,
S. pneumoniae.
5.
In children between 1 and 4 years of age the Gram- negative Haemophilus
influenzae is fairly common cause.
6.
Proteus mirabilis and anaerobic Bacteroides fragilis occasionally cause bone
infection.
7.
Patients with Sickle cell disease are prone to infection by Salmonella typhi.
8.
Unusual organisms are more likely to be found in heroin addicts.
Page of
2
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
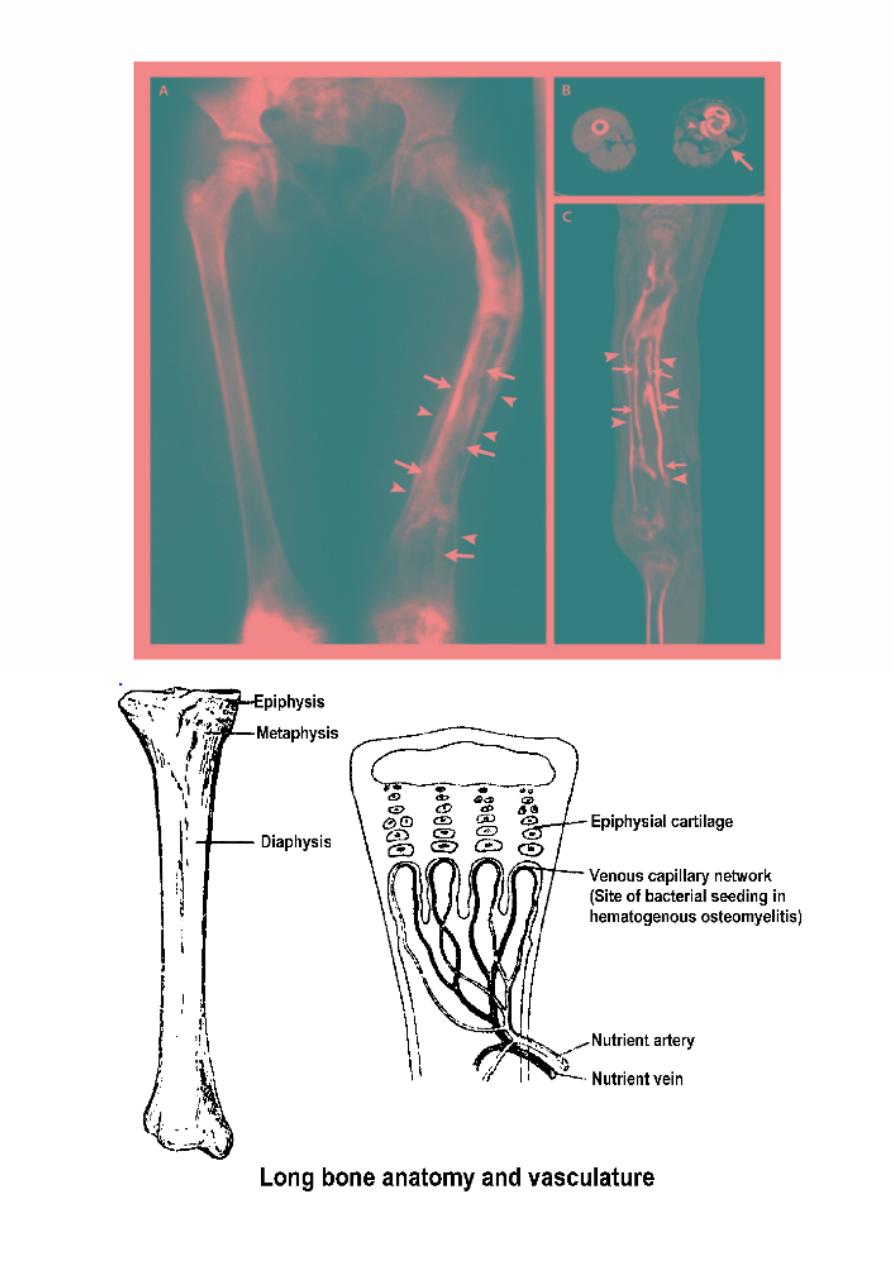
PATHOGENESIS
The infec)on usually starts in the vascular metaphysis of a long
bone, most oLen in the proximal )bia or in the distal or proximal ends of
the femur.
Predilec)on for this site has been aPributed to the peculiar
arrangement of the blood vessels in that area.
The non-anastomosing terminal branches of the nutrient artery
twist back in hairpin loops before entering the large network of sinusoidal
veins, the rela)ve vascular.
Stasis and consequent lowered oxygen tension are believed to
favour bacterial coloniza)on.
In infants , in whom there are s)ll anastomoses between
metaphyseal and epiphyseal blood vessels , infec)on can also reach the
epiphysis.
In adults haematogenous infec)on accounts for only about 20 % of
the cases of osteomyeli)s, mostly affec)ng the vertebrae.
PATHOLOGY
Acute haematogenous osteomyeli)s shows a characters)c
progression marked by:
1-
inflamma)on
, 2-
suppura)on
, 3-
bone necrosis
, 4-
reac)ve new bone
forma)on
, and 5-
resolu)on
and
healing
or
intractable chronicity
.
The pathological picture varies considerably , depending on pa)ent’s
age, the site of infec)on, the virulence of the organism and the host
response.
I.
Inflammation:
Acute inflammatory reac)on with vascular conges)on , exuda)on of
fluid and polymorphonuclear leucocytes infiltra)on.
Page of
3
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
The intraosseous pressure rises rapidly , causing intense pain ,
obstruc)on to blood flow and intravascular thrombosis.
II. Suppuration:
By the second or third day , pus forms within the bone and forces its
way along the Volkmann canals to the surface where it produce a
subperiosteal abscess.
This is much more evident in children , because of the rela)vely
loose aPachment of the periosteum , than in adults.
From the subperiosteal abscess pus can spread along the shaL, to
re-enter the bone at another level or burst into the surrounding soL
)ssues.
The developing physis acts as a barrier to direct spread towards the
epiphysis , but where the metaphysis is partly intracapsular ( e.g. At the
hip , shoulder or elbow ) , pus may discharge through the periosteum into
the joint.
III. Bone necrosis:
The rising intraosseous pressure , vascular stasis , small- vessel
thrombosis and periosteal stripping increasingly compromise the blood
supply , by the end of a week , there is usually microscopic evidence of
bone death.
Pieces of dead bone may separate as sequestra varying in size from
mere spicules to large necro)c segments of the cortex.
IV. Reactive new bone formation:
Is a feature of advancing acute osteomyeli)s , ini)ally the area
around the infected zone is poro)c ( due to hyperaemia and osteoclas)c
ac)vity ).
But if the pus is not released , new bone starts forming on viable
surfaces in the bone and from the deep layers of the stripped periosteum.
Page of
4
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
This is typical of pyogenic infec)on and fine streaks of subperiosteal
new bone usually become apparent on x- ray by the end of the second
week.
With )me this new bone thickens to form involucrum , enclosing the
seqestrum and infected )ssue.
If the infec)on persists , pus and )ny sequestrated spicules of bone
may discharge through perfora)ons ( cloacae ) in the involucrum and
track by sinuses to the skin surface.
*
Note:
if the infection is controlled and intraosseous pressure released at an early
stage , this progress can be stopped.
The bone around the zone of infec)on become increasingly dense ,
this together with periosteal reac)on , results in thickening of the bone.
In some cases the normal anatomy may eventually be
recons)tuted , in others the bone is leL permanently deformed.
*
Note:
if the healing does not occur , a nidus of infection may remain locked inside
the bone, causing pus and sometimes bone debries to be discharged
intermittently through a persistent sinus (or several sinuses), at this stage ,the
infection is chronic osteomyelitis and may last for many years.
V. Resolution and healing:
CLINICAL FEATURES
The pa)ent usually a child over 4 years , presents with severe pain ,
malaise and a fever.
The parents will have no)ced that he or she refuses to use one limb or to
allow it to be handled or even touched.
There may be recent history of infec)on , a sep)c toe , a boil , a sore
throat or a discharge from the ear.
Typically the child looks ill , the pulse rate is likely to be over 100 and the
temp. Is raised.
Page of
5
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
The limb is tender near one of the large joints.
Local redness , swelling , hotness and oedema are later signs.
*
Note:
it is important to remember that all these features may be attenuated if
antibiotics have been administered.
INVESTIGATIONS
1. Plain x-ray:
During the
first week
aLer the onset of symptoms the plain x- ray
shows no abnormality of the bone.
Dissplacement of the fat planes signifies soL )ssue swelling , but
this could as well be due to a haematoma or soL )ssue infec)on.
By the
second week
there may be a faint extra- cor)cal outlines due
to periosteal new bone forma)on .
Later
the periosteal thickening becomes more obvious and there is
patchy rarefac)on of the metaphysis.
*
Note:
an important late sign is the combination of regional osteoporosis with a
localised segment of increased density, Osteoporosis is a feature of metabolically
active, and thus living bone.
The segment that fails to become osteoporo)c is metabolically
inac)ve and possibly dead.
2. Radionuclide scanning:
Radioscin)graphy with Tc ( 99 ) reveals increased ac)vity in both the
perfusion phase and the bone phase .
This is a highly sensi)ve test even in the very early stages , but it has
rela)vely low specificity and other inflammatory lesions can show similar
changes.
Scanning with Ga(67) – citrate or In (111) – labelled leucocytes may
be more revealing.
Page of
6
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
3. Magnetic Resonance Imaging:
It is extremely sensi)ve , even in the early phase of bone infec)on
and can therefore assist in differen)a)ng between soL )ssue infec)on
and osteomteli)s.
4. Laboratory investigation:
The most certain way to confirm the clinical diagnosis is to aspirate
pus or fluid from the metaphyseal subperiosteal abscess, the
extraosseous soL )ssue or an adjacent joint.
Tissue aspira)on will give a posi)ve result in over 60 % of cases
Blood cultures are posi)ve in less than half the cases of proven
infec)on.
The C- reac)ve protein ( CPR ) values are usually elevated within 12
-24 hours and ESR within 24 -48 hours aLer the onset of symptoms.
The WBC count rises and the Hb conc. May be diminished.
*
Note:
in very young and the very old these tests are less reliable and may show
values within the range of normal.
Differential diagnosis
cellulitis:
there is widespread superficial redness and MRI will help to
dis)nguish between bone infec)on and soL )ssue infec)on.
acute suppurative arthritis:
tenderness is diffuse and movement at
the joint is completely abolished by muscle spasm.
-a progressive rise ( doubling ) in CRP values over 24- 48 hours is said to
be sugges)ve of concurrent sep)c arthri)s.
streptococcal necrotizing myositis:
group A beta haemoly)c
streptococci may invade muscles and cause myosi)s.
Careful history , exam and MRI can differen)ate.
Page of
7
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
acute rheumatism:
the pain is less severe and flits from one joint to
another.
There may be signs of cardi)s , nodules ,or erythema marginatum.
sickle cell crisis:
may present with features similar to acute
osteomyeli)s, in area where Salmonella is endemic
Treat those pa)ents
!
with suitable an)bio)cs un)l the infec)on is
definitely excluded.
Gaucher s disease:
(Pseudo- ostei)s) but here there will be enlargment
of spleen and the liver.
Treatments
If osteomyelitis is suspected on clinical grounds, blood and fluid
samples should be taken for lab. Investigation and then treatment started
immediately without waiting for final confirmation of the diagnosis.
There are 4 lines of treatment:
I.
suppor)ve treatment for pain and dehydra)on.
II.
splintage of the affected part.
III.
appropriate an)microbial therapy.
IV.
surgical drainage.
Complications
I.
epiphyseal damage and altered bone growth.
II.
suppura)ve arthri)s.
III.
metasta)c infec)on.
IV.
pathological fracture.
V.
chronic osteomyeli)s.
Page of
8
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
Chronic osteomyelitis
AETIOLOGY
The usual organisms ( and with time there is always a mixed
infection ) are Staphylococcus aureus Escherichia coli
Streptococcus pyogenes, Proteus mirabilis, Pseudomonas aeruginosa
in the presence of foreign implants, Staphylococcus epidermidis, which is
normally non-pathogenic is the commonest of all.
PATHOGENESIS
Acute haematogenous osteomyeli)s, if leL untreated and provided
the pa)ent does not become sep)caemic, will subside into a chronic bone
infec)on with alterna)ng flare – up and spells of apparent quiescence.
*
Note:
there is evidence that bacteria can survive inside osteoblasts and
osteoclasts and be released when the cells die.
PATHOLOGY
Bone is destroyed or devitalized , either in a discrete area around
the focus of infec)on or more diffusely along the surface of a foreign
implant.
Cavi)es containing pus and pieces of dead bone ( sequestra ) are
surrounded by vascular )ssue and beyond that by areas of sclerosis.
There may be chronic reac)ve new bone forma)on( involucrum).
Sequestra act as substrates for bacterial adhesion in much the
Same way as foreign implants , ensuring the presence of infec)on
un)l they are removed or discharged through perfora)ons in the
involucrum and sinuses that drain to the skin.
The sinus may seal off and then reopened somewhere else , when
the )ssue tension rises.
Bone destruc)on and sclero)c briPle bone may laed to pathological
fracture.
Page of
9
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
CLINICAL FEATURES
The pa)ent presents because pain , fever , redness and
Tenderness have recurred ( flare ) or with discharging sinus.
There may be seropurulent discharge and excoria)on of the
surrounding skin.
INVESTIGATIONS
• Plain x- ray = will show bone resorp)on with thickening and sclerosis of
the surrounding bone.
• A sinogram may help to localize the site of infec)on.
• Radioisotope scintigraphy = very sensi)ve.
• MRI and CT scan = are important also in planning for
• Treatment.
• - During the flare , ESR , CRP , and wbc levels may be increased.
*
Note:
superficial swab sample may not reflect the really persistent infection in the
deeper tissues , so sampling from deeper tissue is important.
Page
of
10
12
MH Khafaji

Dr. Firas Al-Obaidi
Surgery
TREATMENT
Antibiotics these are important for:
1.
to prevent spread of infection
2.
to control acute flare.
Local treatment
A sinus may be painless and need dressing simply to protect the
clothing.
Colostomy paste can be used to stop excoriation of the skin.
OPERATION
-
debridement of the necrotic tissue .
-
changing internal fixation to external fixation device.
-
elimination of the dead space.
-
very rarely , amputation.
COMPLICATIONS
1.
an acute exacerbation.
2.
growth abnormalities.
3.
pathological fracture.
4.
joint stiffness.
5.
sinus tract malignancy. ( rare )
6.
amyloidosis.
Page
of
11
12
MH Khafaji
Dr. Firas Al-Obaidi
Surgery
Page
of
12
12
MH Khafaji
