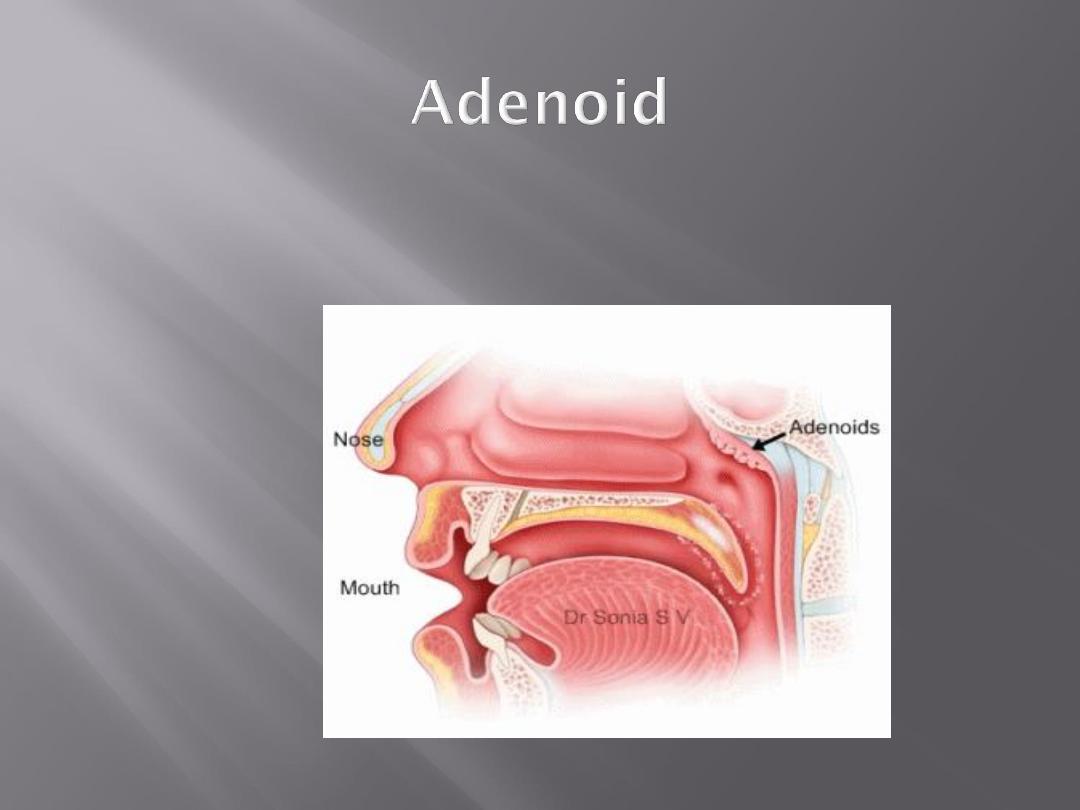
situated at the junction of the
posterior wall and roof of the
nasopharynx
composed of lymphoid tissues
covered by columnar epithelium
it is present at birth
physiologically enlarged up to 6
years then regress and completely
disappears by the age of 20
1- Recurrent attacks of rhinitis
and adenoid infection.
2- Allergy
3- Idiopathic

Nasal obstruction
Mouth breathing and snoring
Nasal discharge
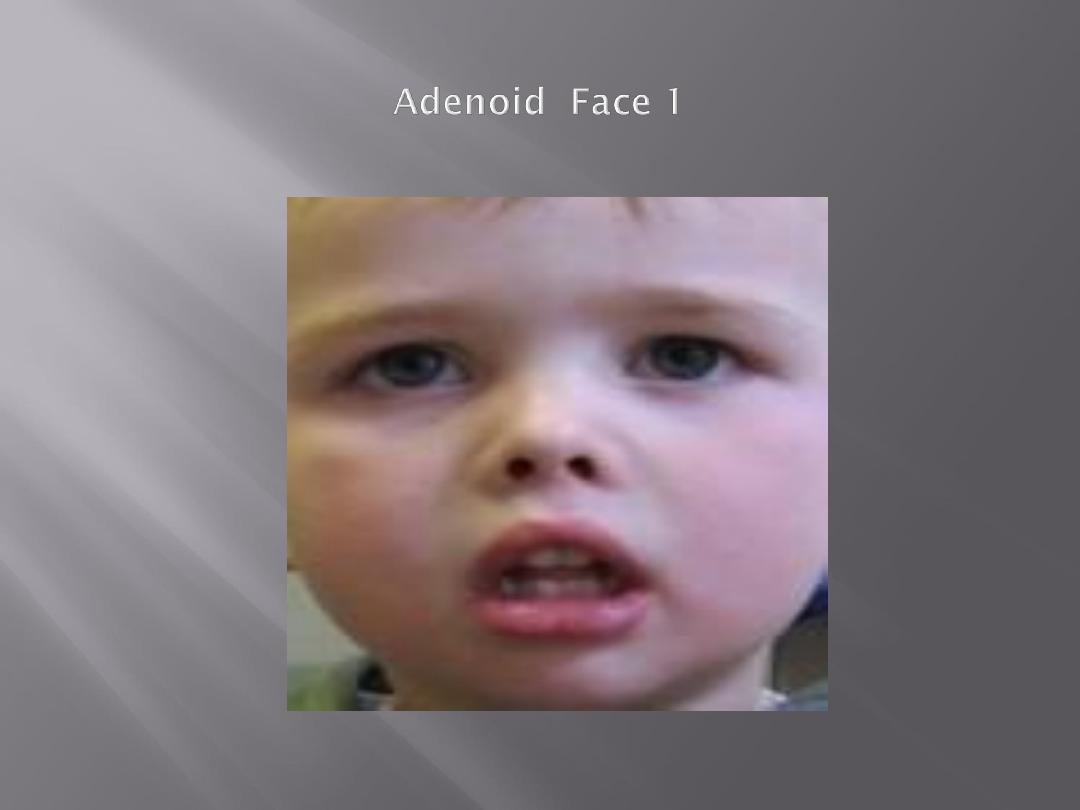
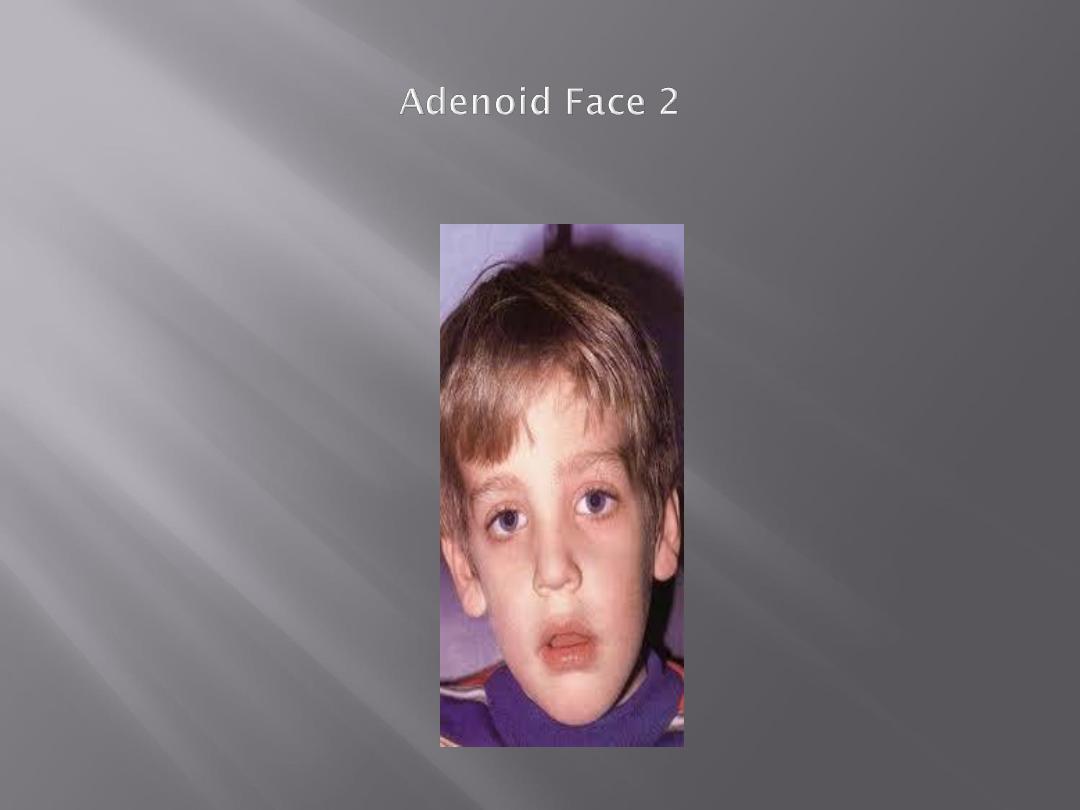
Adenoid face:
elongated face, dull expression,
nasal discharge, open mouth,
hitched-up upper lip, prominent
and overcrowded upper teeth,
high-arched palate
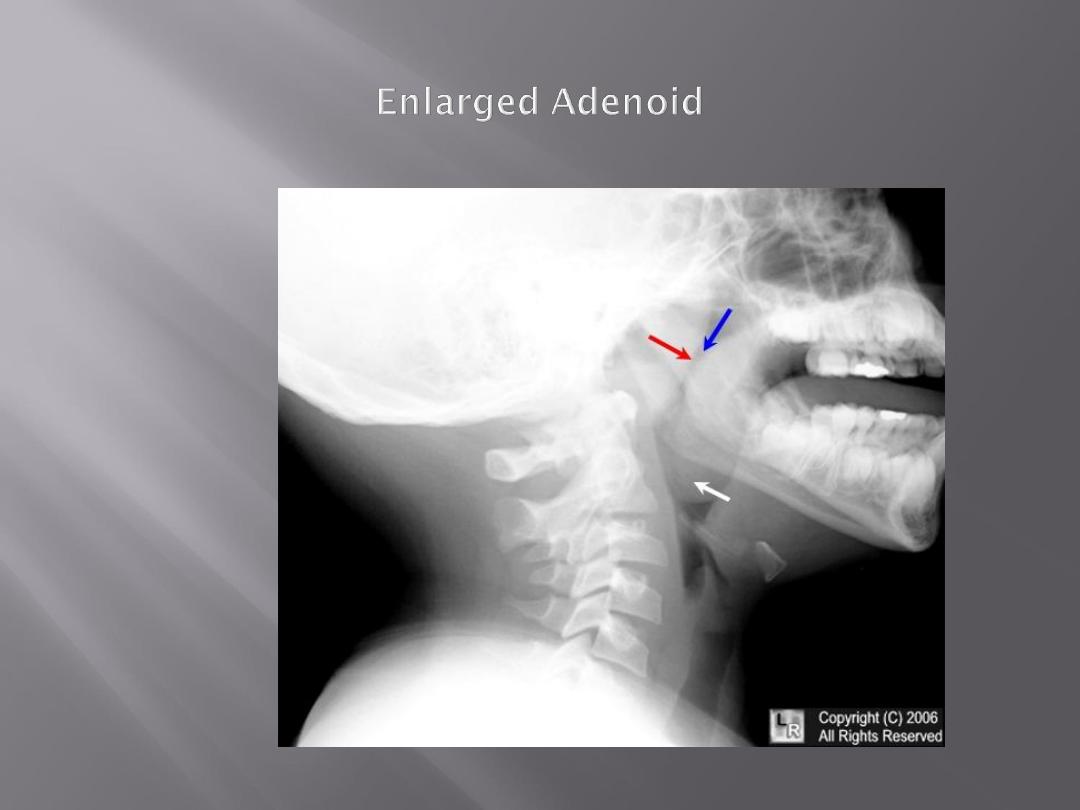
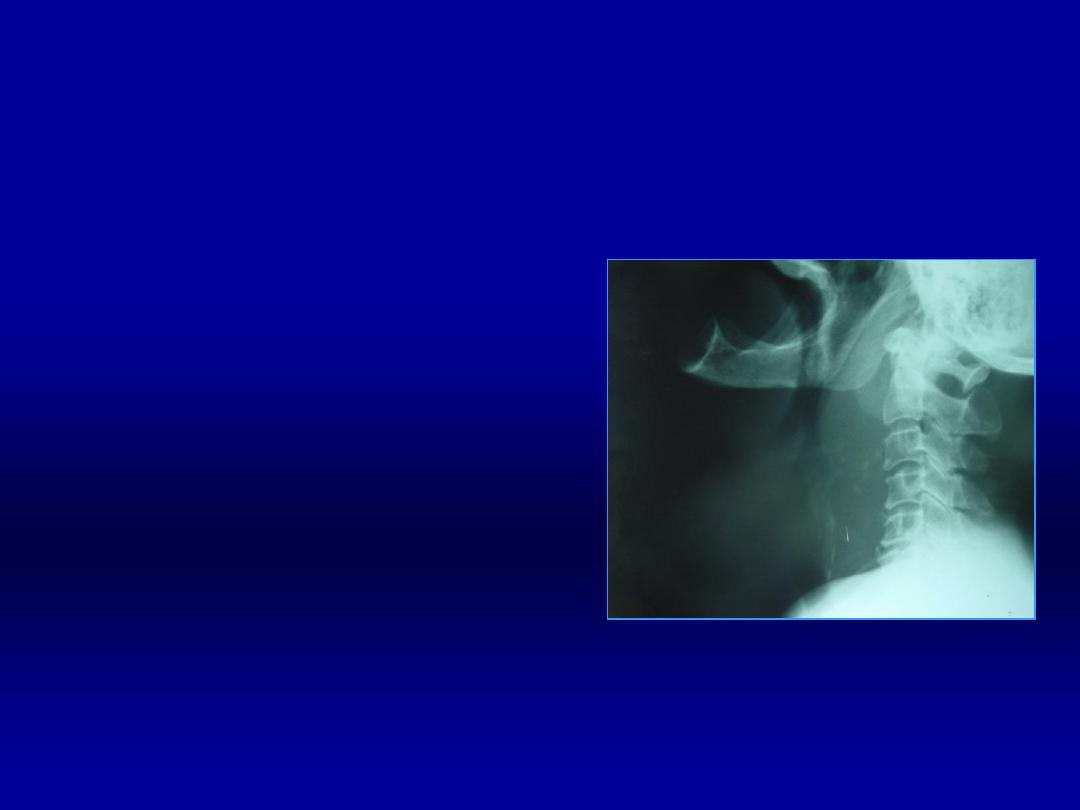
nasopharyngoscopy
X-ray nasopharynx lateral view

When symptoms are not severe,
decongestant nasal drops +
antihistamines is the treatment of
choice. Antibiotics if there is
bacterial infection.
Marked symptoms, treatment is
adenoidectomy
Differential diagnosis:
1- other causes of nasal obstruction (septal
deflection, nasal polyps, allergic rhinitis)
2- orthodontic anomaly
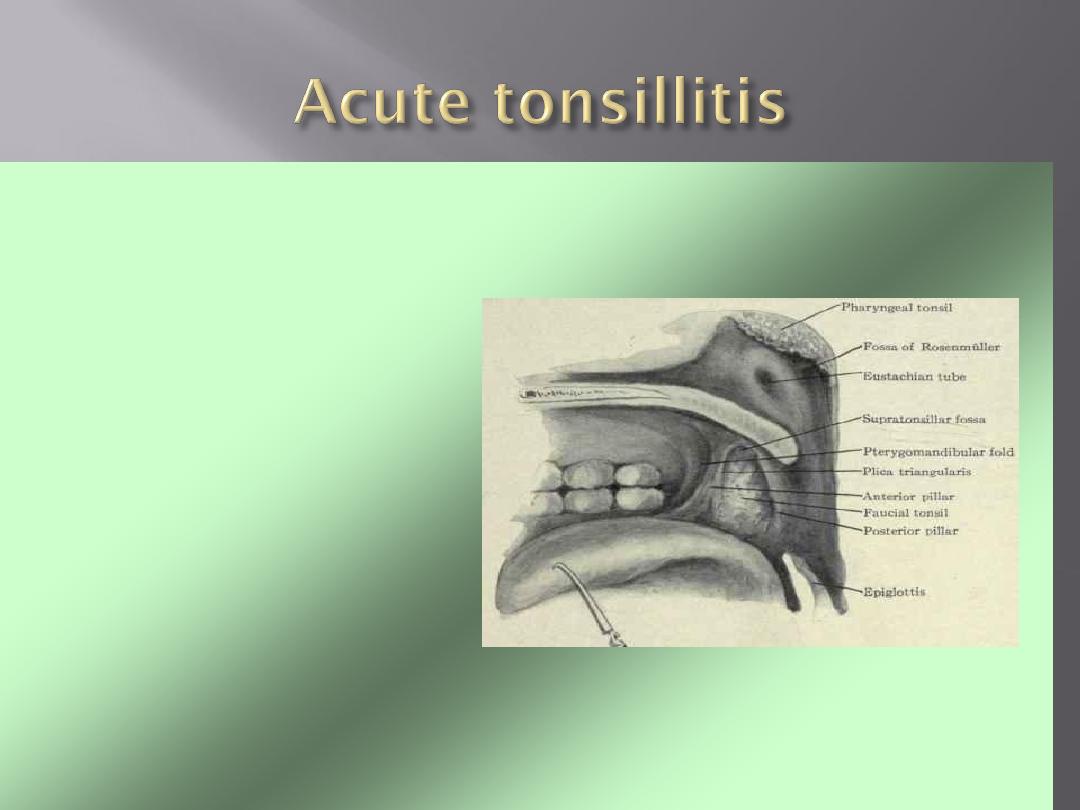
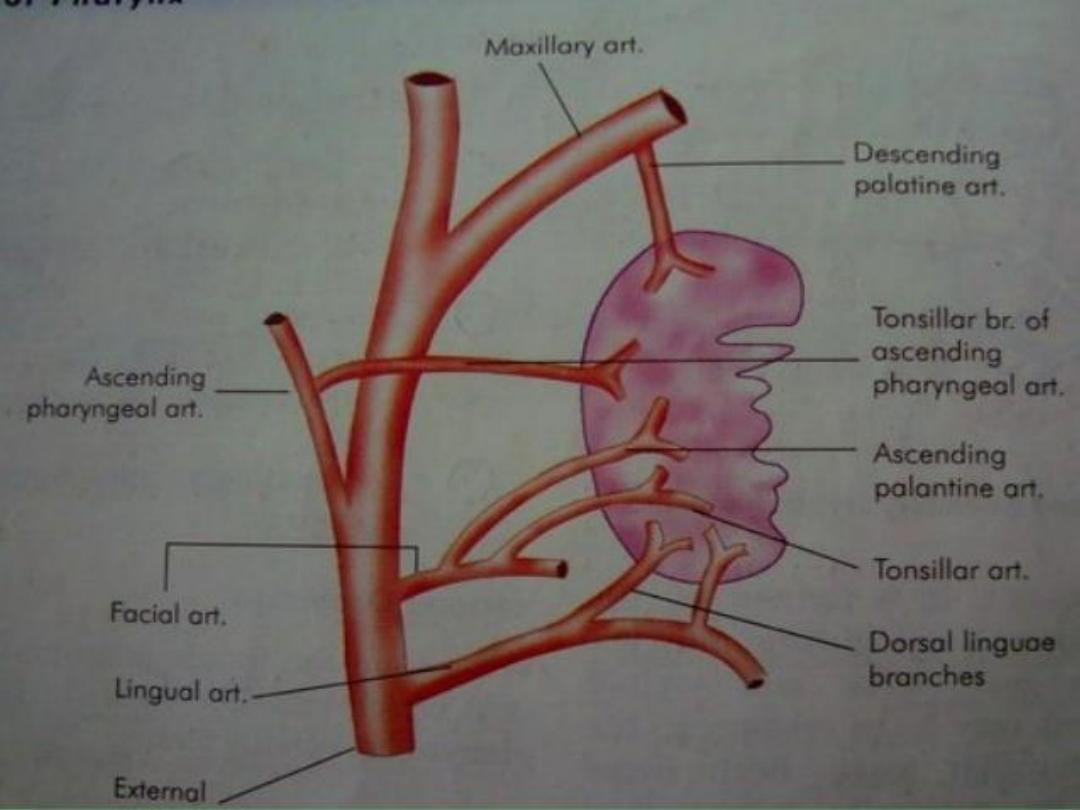
• Palatine tonsils are
large lymphoid
tissue
situated in
the lateral wall of
the oropharynx
.
• They form lateral
part of the
Waldeyer's ring
.
• Tonsil
occupies
the
tonsillar fossa
between diverging
palato-pharyngeal
and palatoglossal
folds
• Tonsil has
two surfaces
, medial and
lateral;
two borders
anterior and
posterior;
two poles
upper and
lower.
• Medial surface
is covered by
squamous epithelium and
presents
15-20 crypts
usually plugged with
epithelial and bacterial debris

• Lateral surface
extends deep to
surrounding boundaries. It
is coated
with a fibrous sheet
, an extension
of pharyngobasilar fascia
called
capsule of the tonsil.
• The
capsule is loosely attached to
the muscular wall
but antero-
inferiorly it is attached firmly to the
side of the tongue just in front of
insertion of palatoglossus and
palatopharyngeus muscles
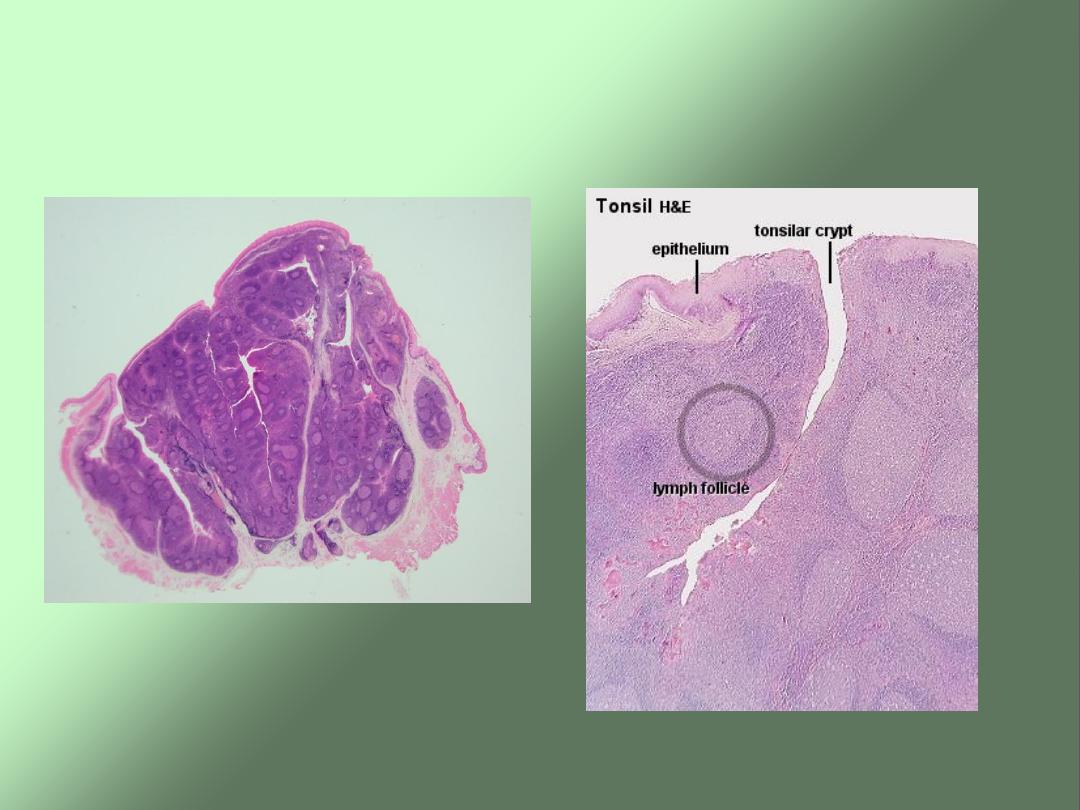
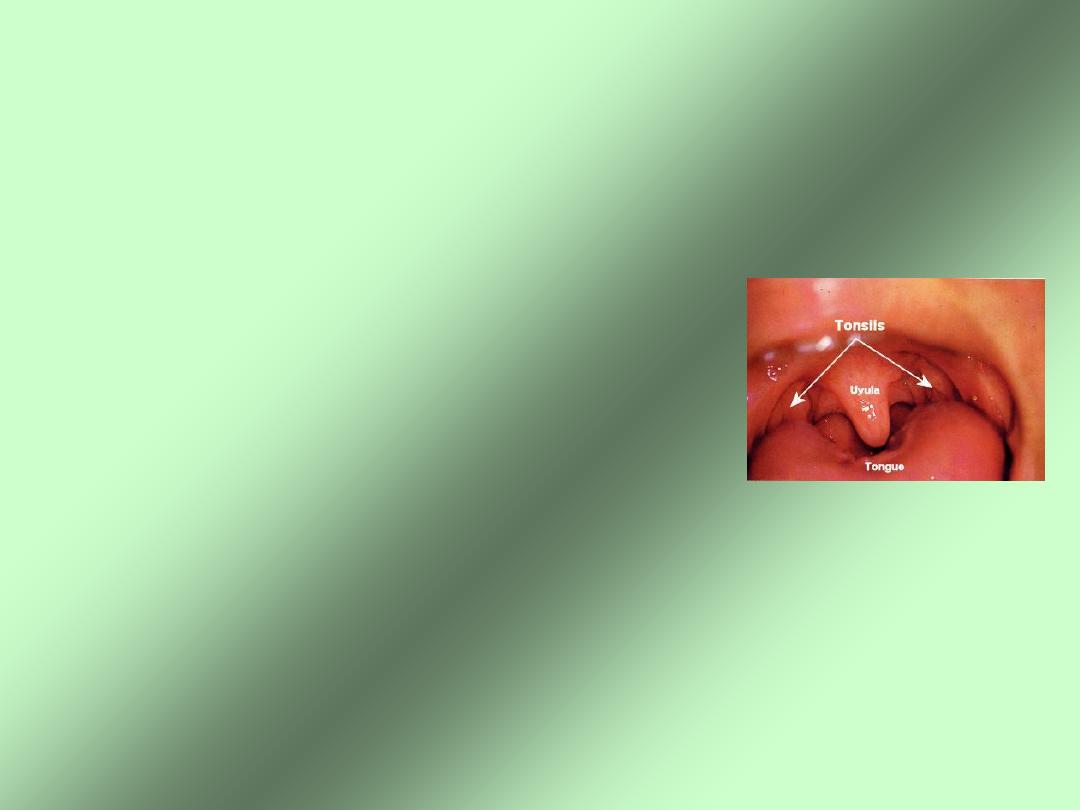
Tonsils-Gross & Microscopic

Acute tonsillitis
Aetiology:
beta hemolytic strept.,viral inf.may be primary.
Pathological types:
1- parynchymatous
2- follicular
Clinical features:
1- sore throat
2- odynophagia
3- pyrexia
4- malaise
5- exam.: enlarged tender cervical LN.

Classification (pathological types)
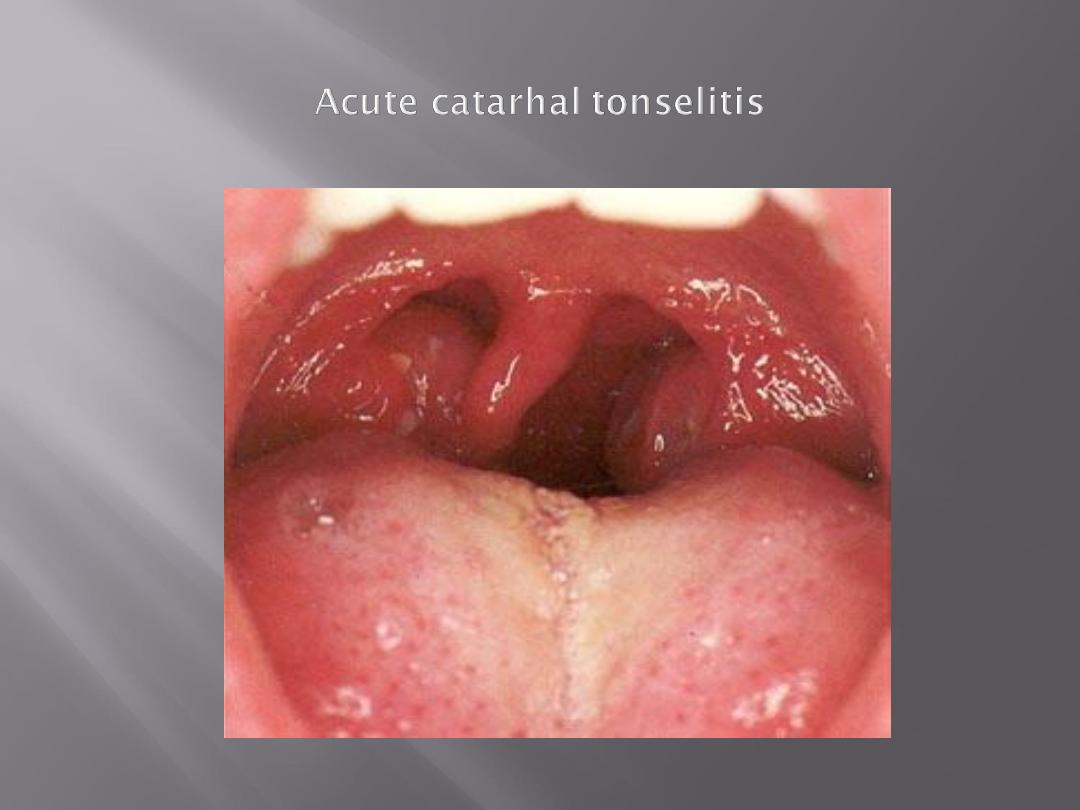
1- Acute catarrhal or superficial
tonsillitis: Here tonsillitis is a
part
of generalized pharyngitis
and
seen in viral infections
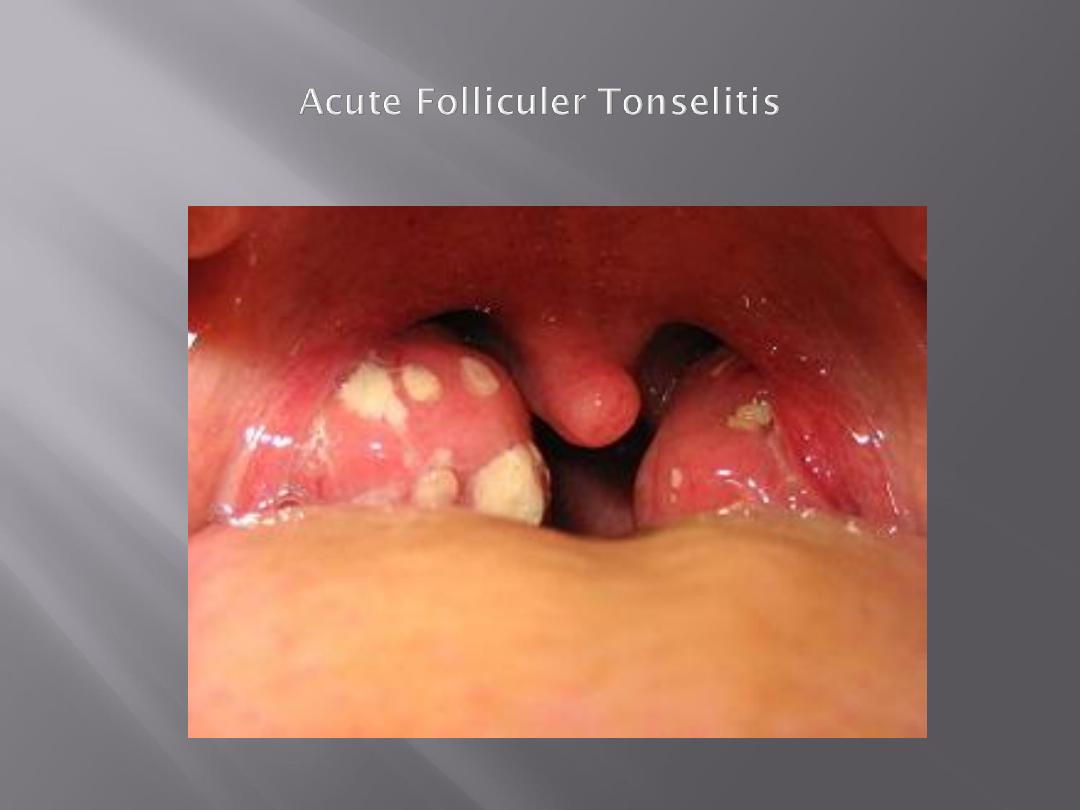
2-Acute follicular tonsillitis: In
which tonsillar
crypts
become filled
with
purulent materials

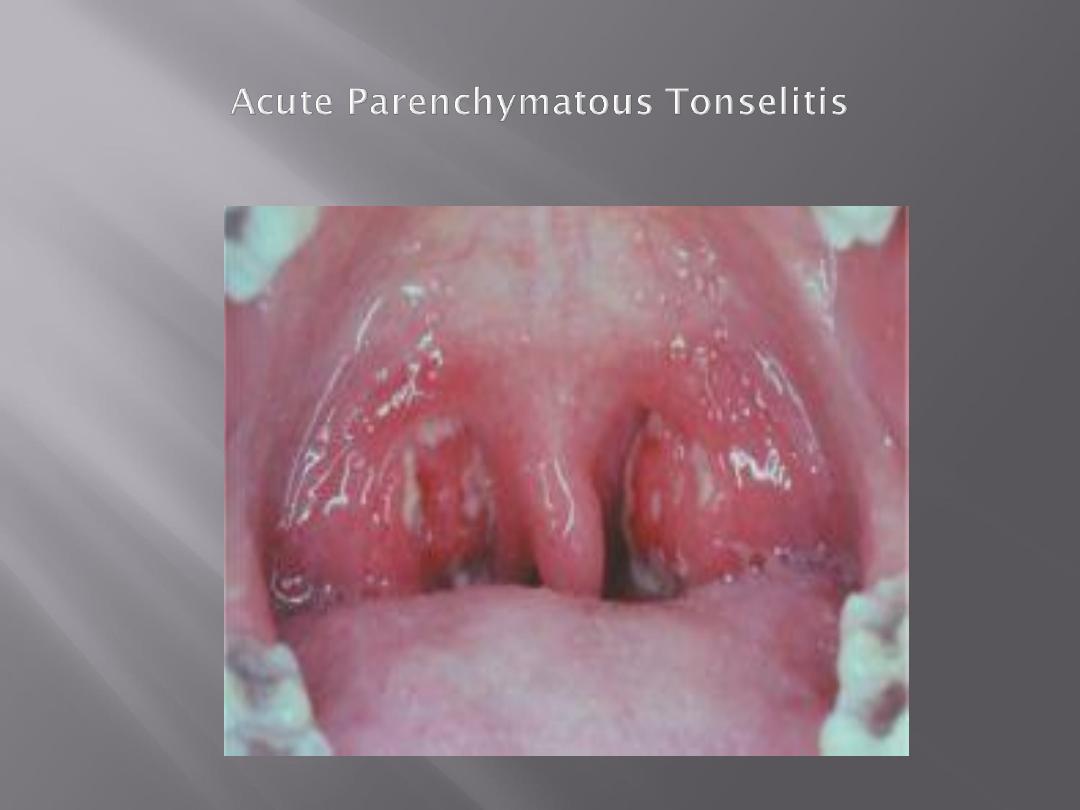
3-Acute parenchymatous
tonsillitis: Here tonsils are
uniformly enlarged and red
4- Acute membranous
tonsillitis: The exudates in the
crypts coalesces to form
membrane on the surface

Affects school-age children but
adults can also be affected. It is
rare in infants (< 1 year age) and
persons above 50 years.
More common in winter months.
Group A beta hemolytic streptococci
Haemophilus influenzae
Streptococcus pneumoniae
Staphylococci
Tuberculosis (in
immunocompromised)
Viruses: adenovirus, Epstein-Bar
virus and herpes simplex virus
sore throat
difficulty in swallowing + pain
fever (can be accompanied by
rigors and chills)
ear ache
headache
generalized body fatigue

breath is foetid and tongue is coated
hyperaemia of the pillars, soft palate
and uvula
red and swollen tonsils with yellowish
spots in the crypts (follicular tonsillitis)
, whitish membrane on the medial
surface of the tonsils (membranous
tonsillitis) or enlarged and congestive
tonsils with swollen uvula (acute
parenchymatous tonsillitis)
enlarged and tender jugulodigastric
lymph nodes

bed rest + plenty of fluids
analgesia (Aspirin or
Paracetamol)
antimicrobial (Penicillin is the
drug of choice) should be
continued for 7 -10 days

Differential diagnosis
1- Scarlet fever
2- Diphtheria
3- Infectious mononeucleosis
4- Blood dyscrasia:leukemia, agranulocytosis
5- Vincent’s angina

Complications:
General
1-Rheumatic fever
2- Glomerulonephritis
3- Septicemia
Local
1- Peritonsillar abscess(quinsy)
2-Paratonsillar abscess
3- Retropharyngeal abscess
4- Otitis media
5- Lower resp.tract infection
Acute rheumatic fever and
glomerulonephritis:
• These diseases are of unknown aetiology
and follow infection with Beta-haemolytic
streptococcus. The current belief is that
antibodies produced against the
streptococcus may in some instances
cross react with patient’s own tissue.
• Thus the effect on tissue may be an
arthritis, endocarditis or myocarditis or a
dermatitis or rheumatic chorea
(inflammation of cerebral cortex and basal
ganglia).
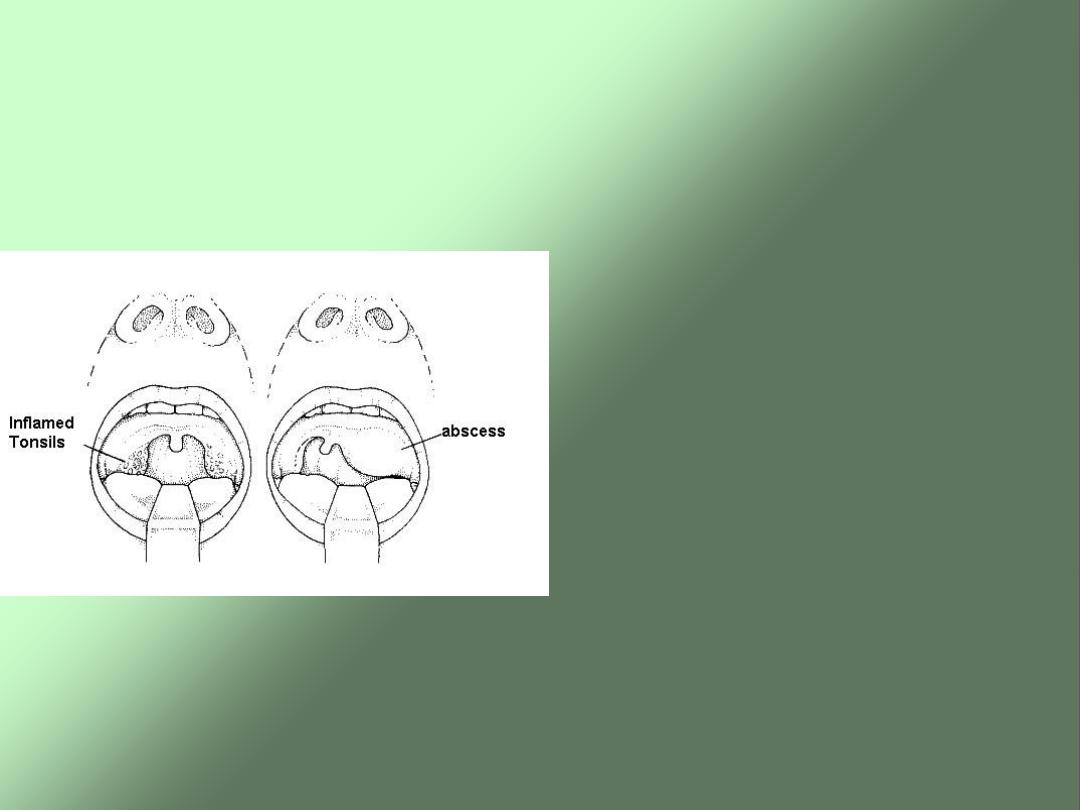
Peritonsillar Abscess or Quinsy
• It is a collection of
pus between fibrous
capsule of the tonsil
usually at its upper
pole and the superior
constrictor muscle of
pharynx.
• It usually occurs as a
complication of the
acute tonsillitis or it
may apparently arise
de novo with no
preceding tonsillitis.

Bacteriology
• The bacteriology of acute
tonsillitis and peritonsillar
abscess is different although one
is a complication of the other.
• The
bacteriology of the quinsy is
characterized by mixed flora with
multiple organisms both aerobic
and anaerobic
.

Clinical Features
• Fit and young adult
with a prior history of
repeated attacks of acute tonsillitis.
• Preceded by a sore throat
for 2-3 days
which gradually becomes severe and
unilateral.
• At this stage
patient is ill with fever
, often
a headache and
severe throat pain made
worse by swallowing
.
• There might be
referred otalgia
, pain and
swelling in the neck due to infective
lymphadenopathy.
The patient’s voice
develops a characteristic
‘plummy
’ quality.
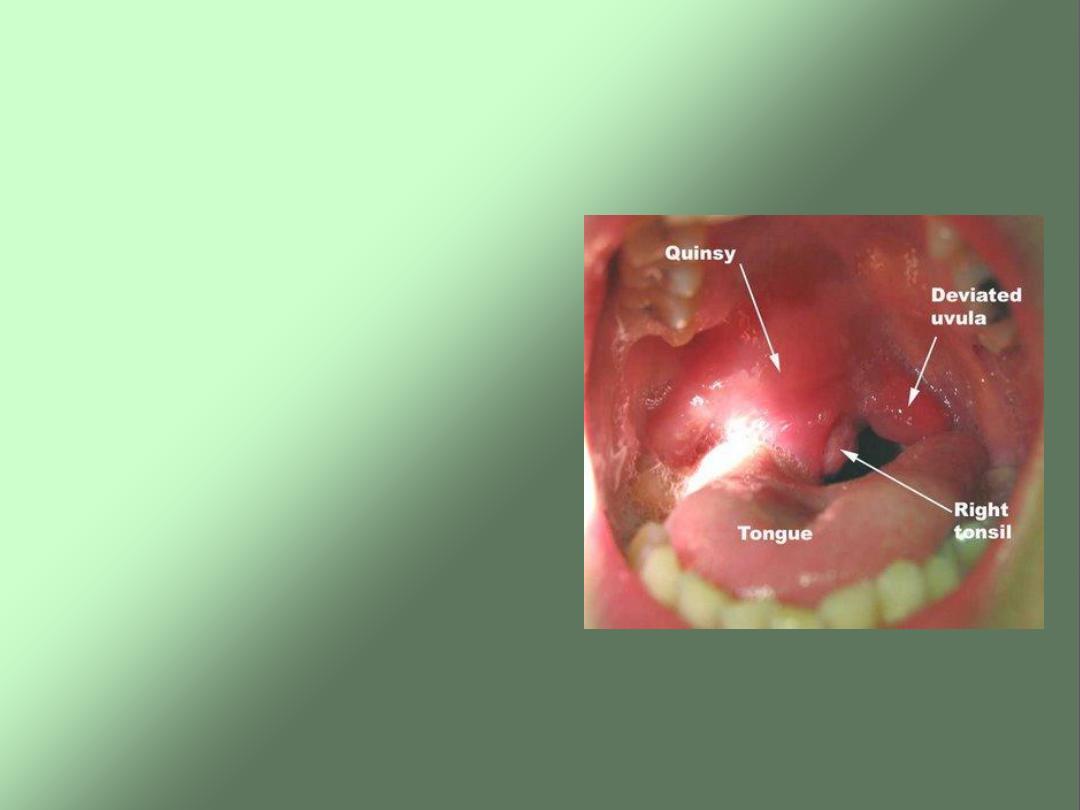
Signs
• Ill looking patient
• Pyrexia
• Often with severe
trismus
• Striking asymmetry
with oedema and
hyperaemia of the soft
palate.
• Enlarged hyperaemic
and displaced tonsil
• Usually enlarged lymph
nodes in JD region.
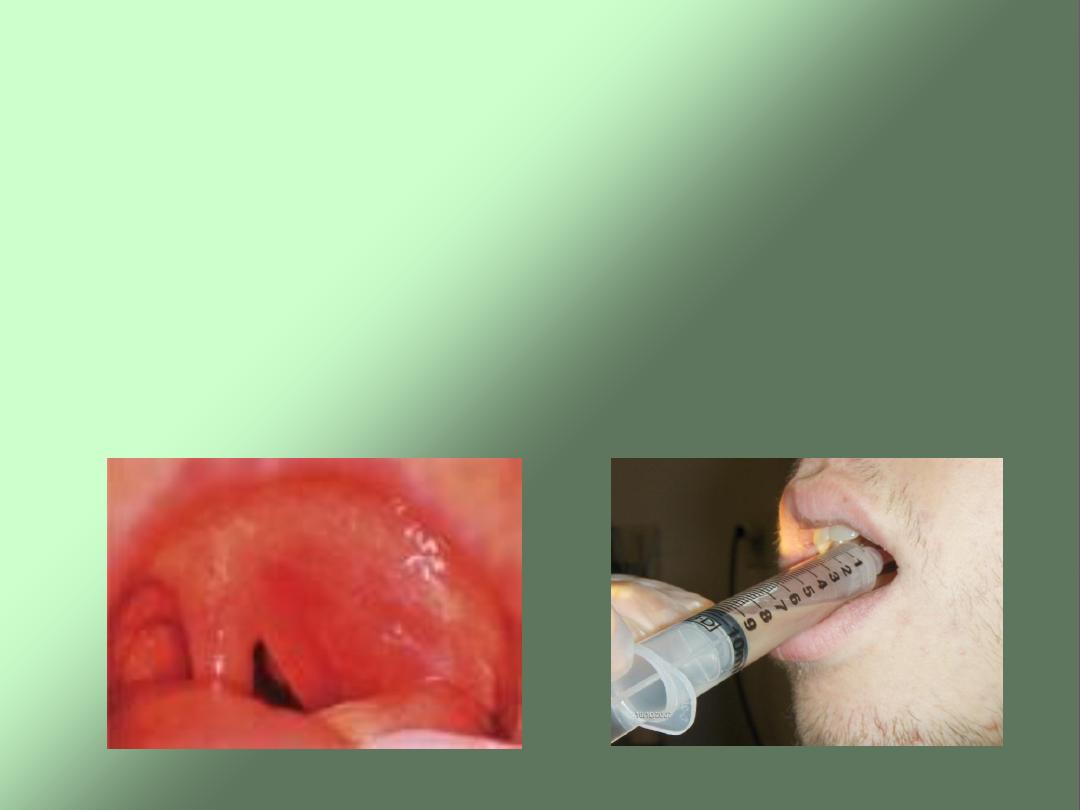
Treatment
• Preferably admitted to hospital and treated
with analgesics and antibiotics.
• In a patient with an early peritonsillar
abscess which is really a peritonsillar
cellulitis incision and drainage are not
recommended.
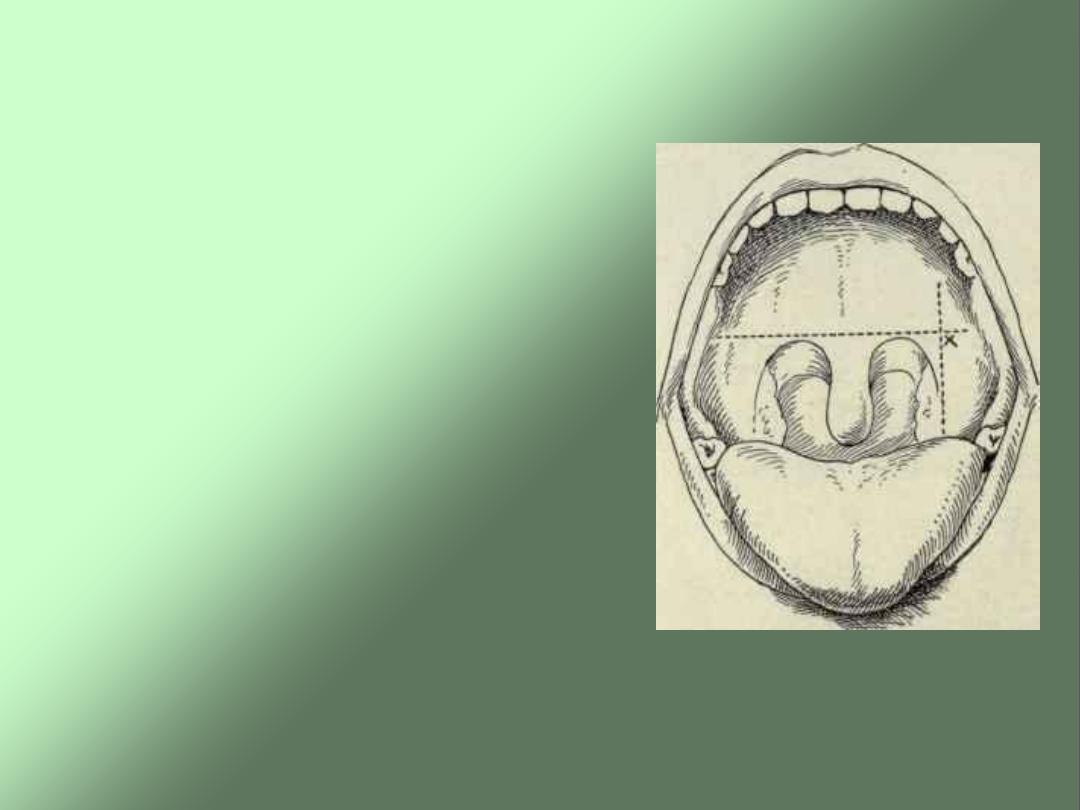
• Indications for I/D
include marked
bulging of soft palate
or failure of an
assumed PTab to
respond to adequate
antibiotics. This is
undertaken at the
point of maximum
bulge
.
• Interval tonsillectomy
after 6 weeks.
• Abscess tonsillectomy.

PARAPHARYNGEAL SPACE
INFECTION
•
Most common cause
:
Peritonsillar infection
•
Typical
finding
1.
Trismus
2.
Angle mandible
swelling
3.
Medial
displacement of lateral
pharyngeal wall
Others : fever, limit neck
motion,neurologic
deficit (C.N
9,10,12,Horner
’s
syndrom)

PARAPHARYNGEAL SPACE INFECTION
Treatment
1. Evaluate and maintain airway & fluid hydration
2. Parenteral antibiotic high dose 24-48 hrs.
3. If not improve, consider surgical drainage

RETROPHARYNGEAL SPACE INFECTION
Types: Acute (children)
Chronic (adults)
• In children: follows
retropharyngeal lymphadenitis from
upper respiratory tract infections
• In adult: follows
regional trauma and TB of the cervical
spines
Clinical feature
irritability,neck rigidity,
torticollis,
fever,drolling,muffle cry,
airway compromise
sore throat, odynophagia,
Investigation
Radiological:
Lateral neck film and CT
scan: might show
widening of the
retropharyngeal space
soft tissue shadow
air-fluid level
spine destruction (TB)

Treatment:
Hospital admission
Maintain the airway (intubation or tracheostomy)
Iv fluids and antibiotics
If abscess develop: drainage
1- Airway obstruction.
2- Septicemia.
3- neurological: cranial nerves palsy (9
th
and 10
th
)
and Horner’s syndrome.
4- Carotid artery rupture.
5- Internal jugular vein thrombosis.



