
1
Fifth stage
Gynecology
Lec-1
.د
اسماء
15/12/2015
Cervical cancer
Cervical cancer is cancer that starts in the cervix, the lower part of the uterus that
opens at the top of the vagina.
It is the most common form of cancer in women in developing countries (because of
lack screening programs), and the second most common form of cancer in the world as
a whole.
Incidence:
Cervical cancer accounts for 6% of all malignancies in women.
It affect women of middle age or older mainly 45-55 years, but it may be diagnosed in
any reproductive-aged woman.
Causes:
Human papillomavirus (HPV) infection with high-risk types has been shown to be a
necessary factor in the development of cervical cancer. HPV DNA may be detected in
virtually all cases of cervical cancer. Not all of the causes of cervical cancer are known.
Several other contributing factors have been implicated.
Causes for cervical cancer:
human papillomavirus (HPV) infection,
HIV infection.
stress and stress-related disorders.
dietary factors.
multiple pregnancies.
exposure to the hormonal drug diethylstilbestrol (DES) .
family history of cervical cancer.
There is a possible genetic risk associated with HLA-B7.

2
Risk groups for cervical cancer:
Young age at first coitus(20years)
Multiple sexual partners.
Young age at first pregnancy.
High parity .
Low socioeconomic state.
Smoking.
Pathology:
Squamous cell carcinoma from squamo-columnar junction comprise approximately
(80–85%) of cervical cancers.
Adenocarcinomas from the columnar cells inside the cervical canal
Cancer may appear as a fun gating, cauliflower – like growth which may completely fill
the vagina or more commonly as an ulcer on the cervix. Cancer may expand cervix into
barrel shaped.
Cervical cancers can spread by:
*Direct Spread may be to cervical stroma, corpus, vagina, bladder and parametrium.
*Lymphatic spread to pelvic and then para-aortic lymph nodes
*Hematogenous spread particularly to lungs, liver, and bone.
Clinical presentations:
Signs and symptoms
a symptomatic:the early stages of cervical cancer may be completely asymptomatic.
Vaginal bleeding, contact bleeding or (rarely)
profuse vaginal discharge .
cervical mass .
moderate pain
Symptoms of local spread :fistula formation (leak age of urine or feces.
Symptoms of distant metastases may be present as enlarged inguinal and
supraclavicular L.N. metastases in the abdomen, lungs or else where in case of
advanced disease.
Systemic manifestation of advanced malignancy as: loss of appetite, weight loss,
fatigue, pelvic pain, back pain, leg pain, single swollen leg, heavy bleeding from the
vagina, leaking of urine or feces from the vagina, and bone fractures.

3
Symptoms:
1.Abnormal vaginal bleeding:
*Post-coital bleeding.
*Inter-menstrual bleeding.
*Menorrhagia. (Some times)
*Post menopausal bleeding.
*Vaginal bleeding in pregnancy.
2. offensive vaginal discharge which may be blood stained.
3. Pain. indicates extension of the growth beyond the limits of the cervix.
4. Leg swelling.
5. Urinary frequency.
6. Incontinence of urine and some times of faeces may occur.
7. bowel changes
8. malaise and weight loss.
Signs:
In early-stage cervical cancer, physical examination findings can be relatively normal.
*As the disease progresses, the cervix may become abnormal in appearance, with
nodule, ulcer, or mass. Enlarged cervix hard and barrel shaped.
*There is free bleeding on examination and offensive watery discharge.
*Mobility of cervix varies and eventually become fixed.
Bimanual examination findings often reveal pelvic metastasis.
*Rectal examination which is essential to determine the extent of involvement.
*Pyometra occurs occasionally, causing uterine enlargement.
*There may be enlarged inguinal or supra-clavicular lymph nodes, oedema of legs,
ascitis, pleural effusion, or hepatomegally.
Differential diagnosis:
1. Cervicitis.
2. Cervical ectropion.
3. Endometrial carcinoma.
4. Pelvic inflammatory disease (PID).
5. Vaginal cancer
6. Metastatic cancer to cervix (rare).
4
7. Tuberculosis
8. Syphilitic chancre
9. Choriocarcinoma.
Investigations:
Diagnosis should be based on histology and appropriate biopsies.
After the diagnosis is established, investigation which needed are:
Complete blood cell count
Renal functions test
Hepatic functions test
Imaging Studies: for staging
Chest radiograph should be obtained to help rule out pulmonary metastasis.
CT scan of the abdomen and pelvis is performed to look for metastasis in the liver,
lymph nodes, or other organs and to help rule out hydronephrosis/ hydroureter.
Barium enema (sometimes).
Intravenous urogram.
Staging:
o Clinical Staged Disease
Physical Exam
Blood Work
Cystoscopy
Proctoscopy
IVP
Stage 0 - full-thickness involvement of the
Stage I - limited to the cervix
IA - diagnosed only by microscopy; no visible lesions
IA1 - stromal invasion less than 3 mm in depth and 7 mm or less in
horizontal spread
IA2 - stromal invasion between 3 and 5 mm with horizontal spread of
7 mm or less
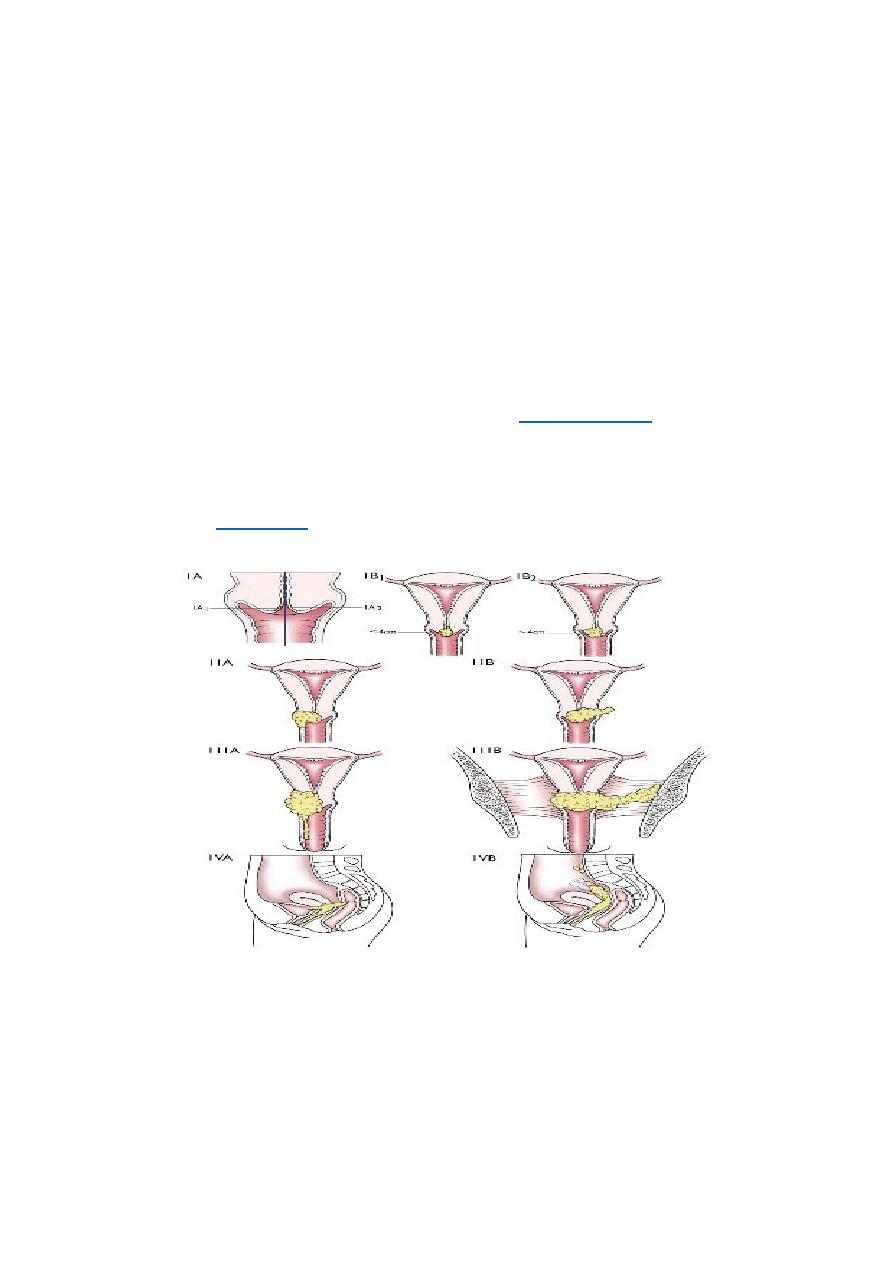
5
IB - visible lesion or a microscopic lesion with more than 5 mm of depth or
horizontal spread of more than 7 mm
IB1 - visible lesion 4 cm or less in greatest dimension
IB2 - visible lesion more than 4 cm
Stage II - invades beyond cervix
IIA - without parametrial invasion, but involve upper 2/3 of vagina
IIB - with parametrial invasion
Stage III - extends to pelvic wall or lower third of the vagina
IIIA - involves lower third of vagina
IIIB - extends to pelvic wall and/or causes
kidney
IVA - invades mucosa of bladder or rectum and/or extends beyond true pelvis
Treatment of Early Disease:
Conization or simple hysterectomy (removal of the uterus) - microinvasive cancer
Radical hysterectomy - removal of the uterus with its associated connective tissues, the
upper vagina, and pelvic lymph nodes. Ovarian preservation is possible.
Chemoradiation therapy

6
Factors that influence the mode of treatment include:
1. Stage and type of lesion.
2. Age of patient.
3. Health status.
The treatment of cervical cancer frequently requires a multidisciplinary approach.
1. Surgery
should only be considered an option for early disease (stage 1 and stage 11a).
2. Radiation
The standard treatment of cervical cancer may involve:
1. surgery
or 2. radiotherapy
or 3. a combination of both.
Early cervical cancers (stage I and IIA) may be treated by either procedure.
Radiotherapy is the treatment of choice once the disease has spread beyond the
confines of the cervix and vaginal fornices, when surgery is not effective.
Stage Ib2-IVa
1. Surgery
*The standered surgical procedure of cervical carcinoma is a Wertheim's radical
abdominal hysterectomy which involves removal of the uterus, paracervical tissue, and
upper vagina and pelvic lymph nodes.
Early microinvasive disease can be treated by cone biopsy or excisional treatment
alone .
Complications of radical hysterectomy:
The most frequent complication of radical hysterectomy is:
1. Urinary dysfunction
2. Hemorrhage
3. Infection.
4. Bowel obstruction.
5. Bladder and rectovaginal fistulas.
7
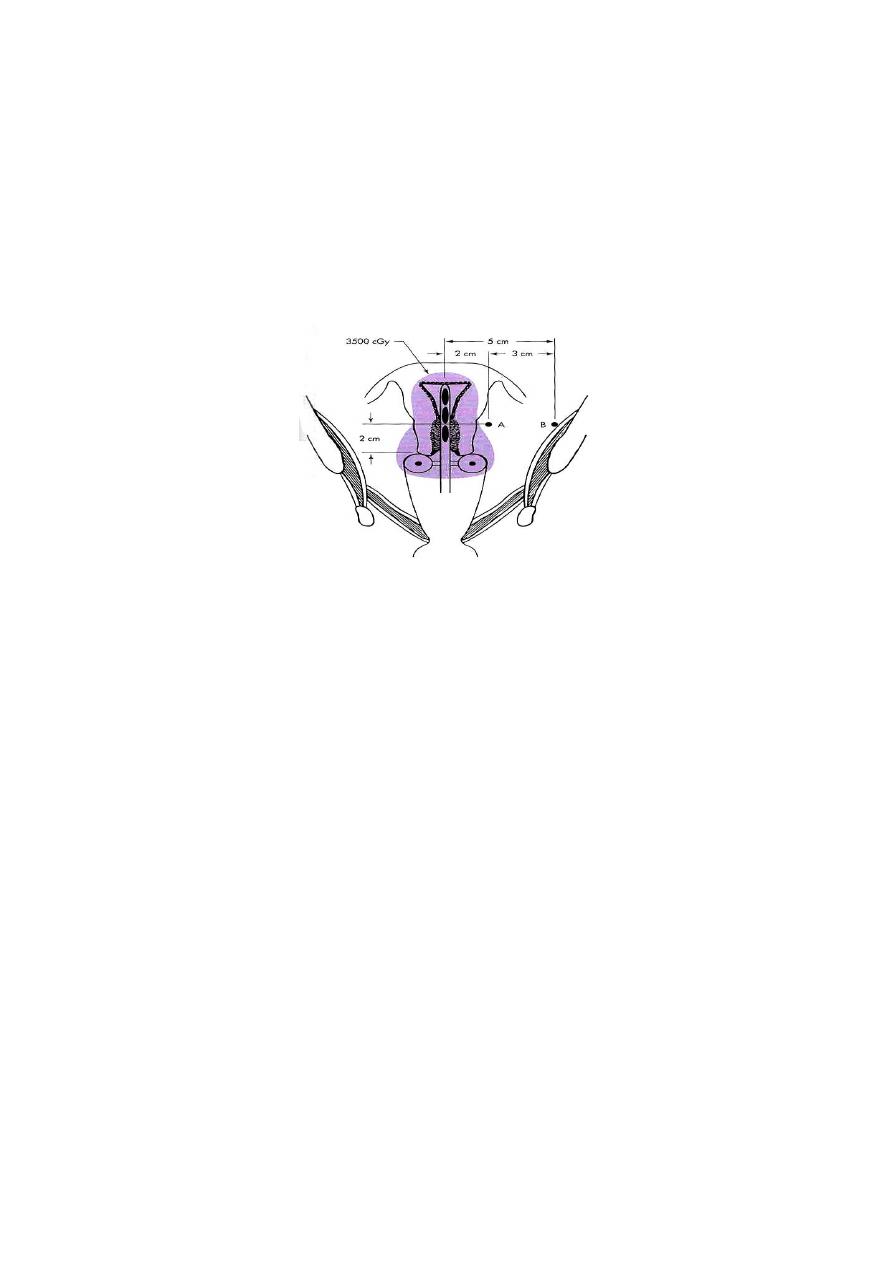
2. Radiation
Can be used for all stages. Once the disease has spread outside cervix, radiotherapy is
the mainstay of treatment.
Radiotherapy of cervical cancer may often involve a combination of:
A. external radiotherapy (for whole pelvis radiation)
B. transvaginal intracavitary irradiation (to the central part of the disease)
Palliative radiation often is used individually to control bleeding, pelvic pain, or urinary
or partial large bowel obstructions from pelvic disease.
Complications from radiation:
1. Acute adverse effect:
A. gastrointestinal effects include diarrhea, abdominal cramping, rectal discomfort, or
bleeding.
B. Cystourethritis can occur, which leads to dysuria, frequency, and nocturia.
2. Late sequelae of radiation usually appear 1-4 years after treatment. The major
sequelae include rectal or vaginal stenosis, small bowel obstruction, malabsorption,
and chronic cystitis.
Symptoms of Recurrence:
Weight loss, fatigue and anorexia
Abnormal vaginal bleeding
Pelvic pain
Unilateral leg swelling or pain
Foul discharge
Signs of distant metastases
NOTE: must distinguish radiation side effects from recurrent cancer

8
Management:
Chemoradiation may be curative or palliative, especially in women who have not
received prior radiation therapy.
Isolated soft tissue recurrence may occasionally be treated by resection with long-term
survival.
CERVICAL CANCER DURING PREGNANCY:
Prior to 24 weeks:
the treatment recommended is the same as for women who are not pregnant.
after 24 weeks:
When cancer is detected at the time of fetal viability, radical Caesarean
hysterectomy can be offered or the fetus can be delivered and therapy instituted
thereafter.
The route of delivery has traditionally been Caesarean section, though this is more
related to the possibility of increased bleeding, rather than the older concept of spread
of disease if the vaginal route is chosen.
Prognosis:
FIVE YEAR SURVIVAL RATES FOR CERVICAL CANCER
Stage I 80%
Stage II 65%
Stage III 30%
Stage IV 15%
