
د.منى
\
radiology L3
GIT IMAGING TECHNIQUE
Imaging techniques: general principles
Contrast examinations
1. Barium sulphate is the best contrast medium for demonstrating the GI tract on conventional
radiographic studies, e.g. fluoroscopy (screening). It produces excellent opacification, good
coating of the mucosa and is completely inert.
Its disadvantages are that the barium may solidify and impact proximal to a colonic or rectal stricture,
and it may cause a severe inflammatory peritonitis if there is a barium leak from the bowel. In
addition, patients must be reasonably mobile in order to undertake a complete barium study.
2. A water-soluble contrast medium, such as Gastrografin, is predominantly used when
perforations or anastomotic leaks are suspected (as it does not cause inflammatory
peritonitis), in cases where small bowel obstruction is suspected and in specific circumstances
in pediatric patients.
it is an irritant should it inadvertently enter the lungs; and it is less radio-opaque than barium.
Computed tomography
1. CT can show the full width of the wall of the structures in question as well as the surrounding
fat.
2. the lumen of the gastrointestinal tract may be evaluated using either Gastrografin as the
contrast agent (e.g. standard abdominal CT),
3. CT is therefore useful for diagnosing and staging GI tumours
4. assessing the complications of treatment such as surgery and chemotherapy.
5. CT can be used to diagnose appendicitis and is useful in patients with intestinal obstruction and
suspected damage to the bowel wall following trauma.
Ultrasound examinations
1. detect intra-abdominal fluid and assess the bowel wall in certain situations, but gives
limited information about the bowel mucosa.
2. diagnosis of infantile pyloric stenosis, intussusception and appendicitis when the diagnosis
is not obvious clinically.
3. The use of endoscopic ultrasound assessing the depth of invasion of tumours in the
oesophagus, gastric or rectal wall and diagnosing small tumours in the pancreas and wall of
the duodenum
.
Magnetic resonance imaging
1. be limited use, due to artefacts caused by peristalsis of the bowel.
2. assessing the local spread of rectal carcinoma prior to surgical resection,
3. assessing perianal fistula and abscess formation
4. The role in the assessment of oesophageal cancer is currently under development
د.منى
\
radiology L3
OESOPHAGUS
Imaging techniques
Plain films
1. do not show the oesophagus unless it is very dilated (e.g. achalasia),
2. but they are of use in demonstrating an opaque foreign body such as a bone lodgedin the
oesophagus
3. Plain films are also used to check the position of a nasogastric tube,
The barium swallow is the standard contrast examination employed to visualize the
oesophagus. The use of CT and endoscopic ultrasound is limited to the assessment of
oesophageal carcinoma.
Endoscopy :its primary investigation used in patient with dysplasia
Barium swallow examination
The patient swallows a gas-producing agent to distend the oesophagus, followed by barium, and its
passage down the oesophagus is observed on a television monitor. Films are taken with the
oesophagus both full of barium to show the outline, and following the passage of the barium to show
the mucosal pattern. The oesophagus has a smooth outline when full of barium. When empty and
contracted, barium normally lies in between the folds of mucosa, which appear as three or four long,
straight, parallel lines. Peristaltic waves can be observed during fluoroscopy.
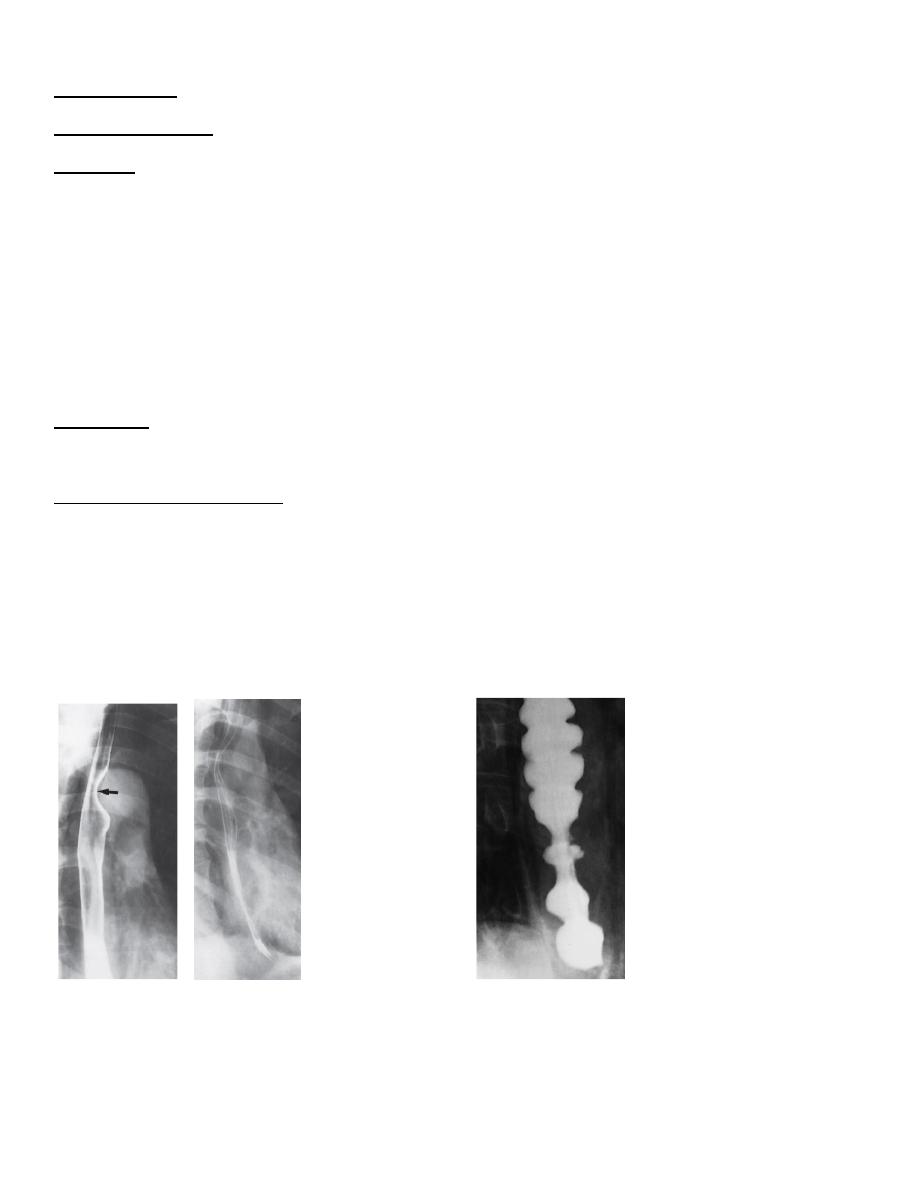
these are normal one
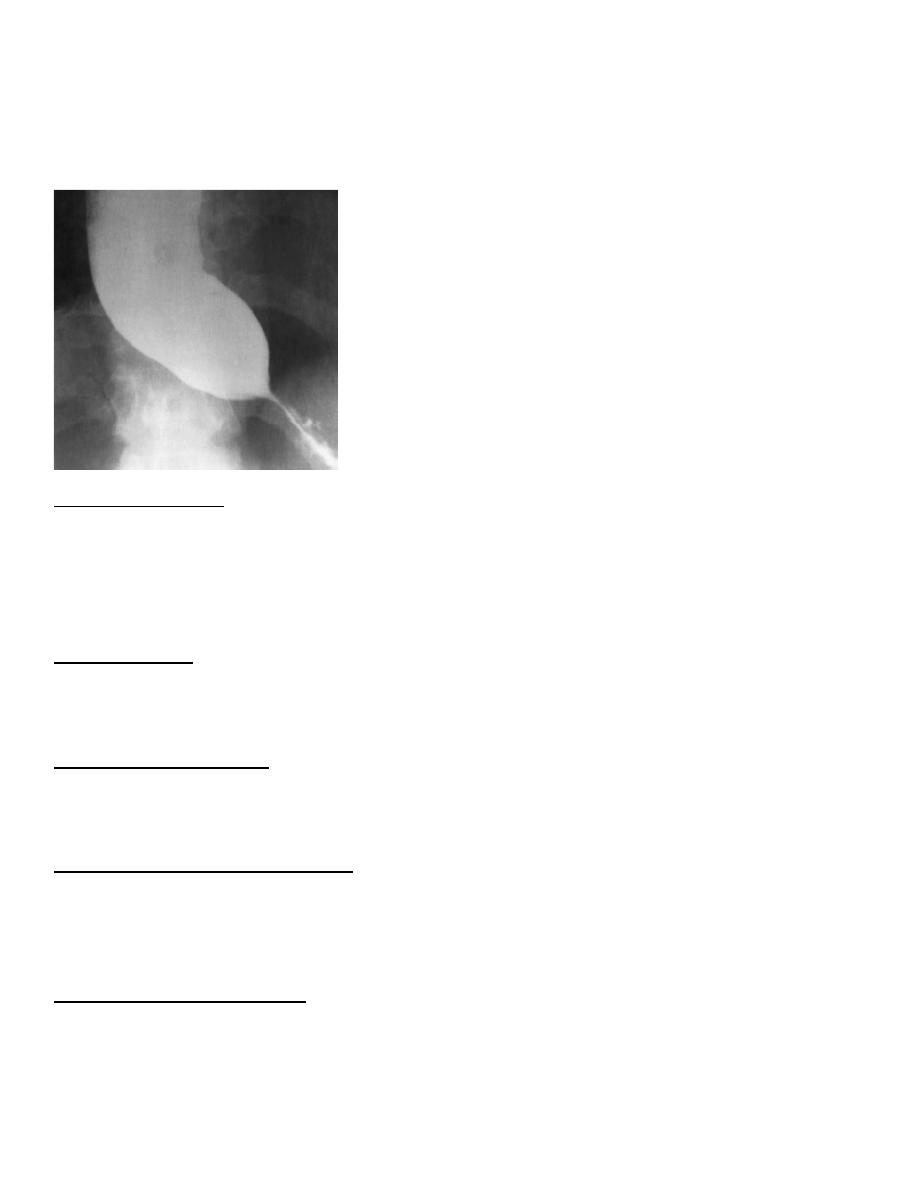
this tertiary contraction
It is important not to confuse a contraction wave with a true narrowing: a narrowing is constant
whereas a contraction wave is transitory. Sometimes the contraction waves do not occur in an orderly
fashion but are pronounced and prolonged, giving the oesophagus an undulated appearance . These
so called tertiary contractions usually occur in the elderly, and in most instances they do not give rise
to symptoms. Occasionally, tertiary contractions cause dysphagia.
د.منى
\
radiology L3
Indications for contrast studies of the oesophagus
1. Swallowing disorders, including confirming or excluding a pharyngeal pouch
2. Determining the length of oesophageal strictures
3. Assessing possible mild gastro-oesophageal reflu. (although usually done by manometry)
4. Assessing the integrity of an oesophageal anastomosis
5. Following obesity reduction surgery and anti-reflux surgery
6. Demonstrating an oesophagobronchial or pleural fistula
Computed tomograpphy
Computed tomography is used in the staging of carcinoma of the oesophagus. The primary function of
CT is to detect distant disease (e.g. lung, liver or bone metastases), and although it does give
information on local staging, this is more accurately performed by endoscopic ultrasound
Fluorodeoxyglucose positron emission tomography/computed tomography
In patients with oesophageal carcinoma who have potentially curable disease, an FDG-PET/CT study is
performed to identify any occult metastases prior to undertaking either surgery or definitive
chemoradiotherapy.
Oesophageal abnormalities
Strictures of the oesophagus
Causes of strictures of the oesophagus are :
1. Oesophageal cancer
2. Peptic strictures
3. Achalasia
4. Corrosive strictures
5. Benign tumours (leiomyomas)
6. Other mediastinal masses
7. Anomalous right subclavian artery
د.منى
\
radiology L3
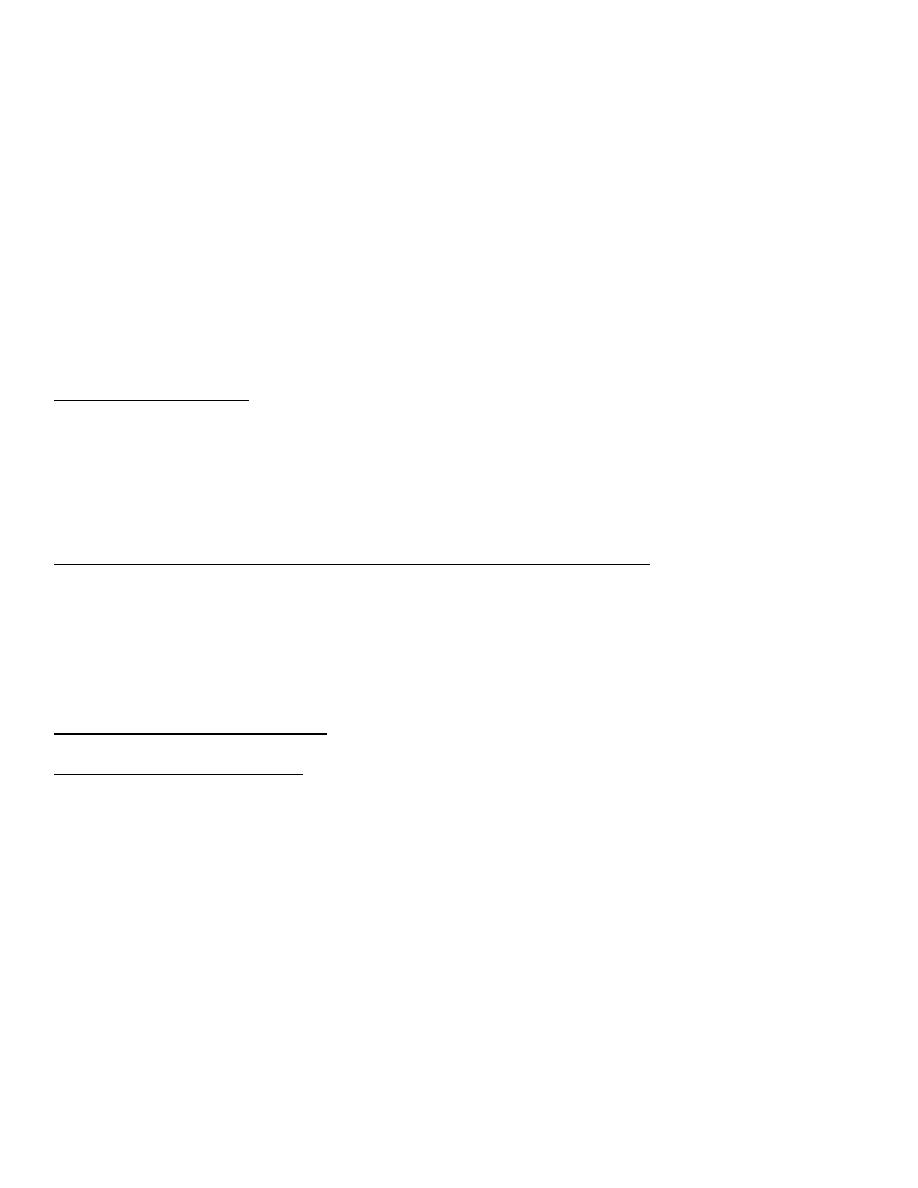
Oesophageal carcinoma
It may occur anywhere in the oesophagus, shows an irregular lumen with shouldered
edges and is often several centimetres in length
A soft tissue mass may be visible.
Assessing the extent of the tumour is carried out by endoscopic ultrasound and CT
examination. Endoscopic ultrasound (EUS) is able to demonstrate the layers of the
oesophageal wall and the surrounding lymph nodes.
Oesophageal cancer is seen as a hypoechoic mass and the depth of invasion of the tumour into
the oesophageal wall may be assessed .EUS is also used to assess and, if necessary, biopsy,
regional lymph nodes to detect potential metastatic disease that might place the patient in a
palliative rather than curative pathway.
د.منى
\
radiology L3
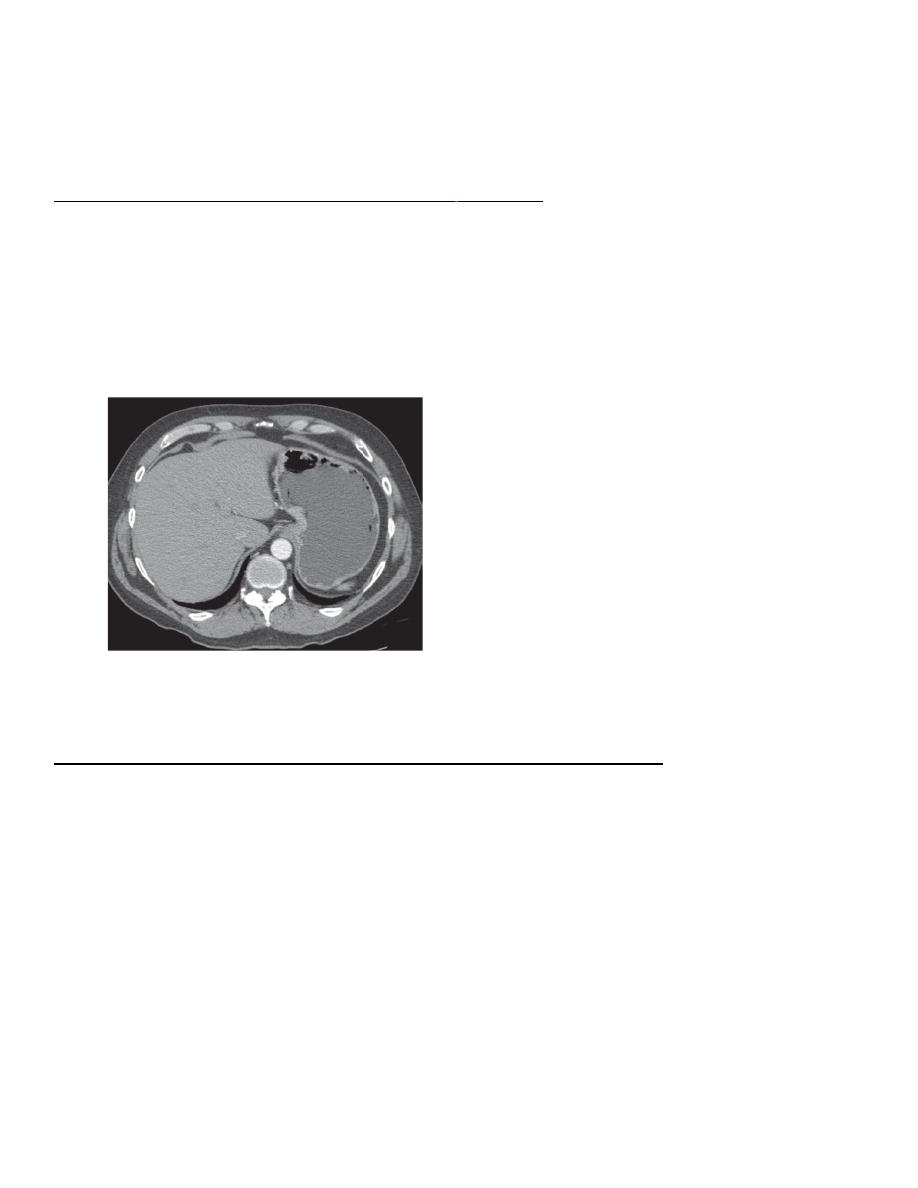
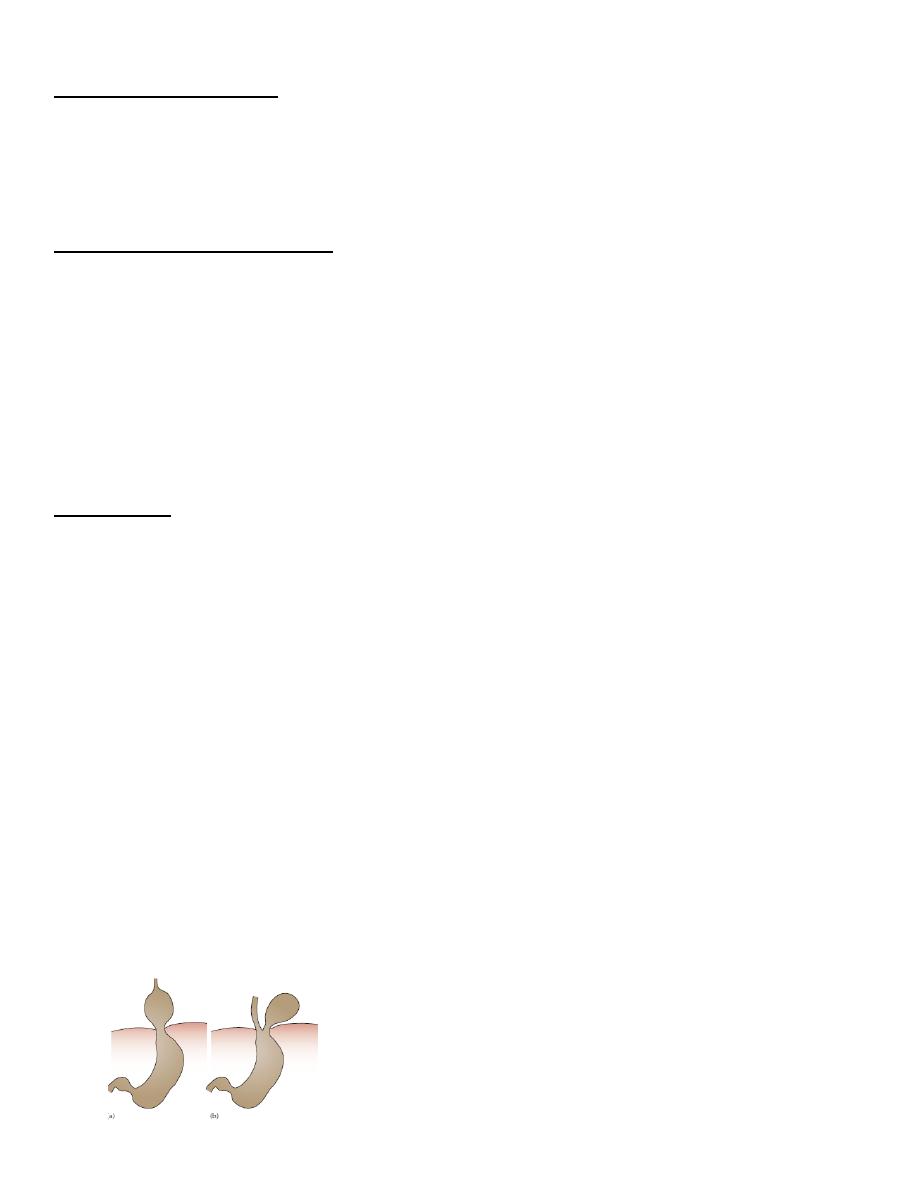
On CT the tumour is seen as a thickening of the oesophageal wall and the length of the tumour
can usually be assessed. CT may also show invasion of the mediastinum or adjacent structures,
evidence of metastatic spread to lymph nodes, liver or lungs .
FDG-PET/CT is used to exclude the presence of occult metastatic disease in patients who are
considered potentially curable (either by surgery or radical chemoradiotherapy) after initial
evaluation with CT and EUS . Assessment of response to treatment and follow-up of patients
with carcinoma of the oesophagus is usually done with CT and endoscopy.increasingly being
used to assess the response of the tumour to chemotherapy or radiotherapy, allowing an early
change in therapy in patients who are non-responders.
Peptic strictures
Peptic strictures can be demonstrated at barium swallow.
They are found at the lower end of the oesophagus and are almost invariably associated with a
hiatus hernia and gastro-oesophageal reflux and, therefore, the stricture may be some distance
above the diaphragm.
Peptic strictures are characteristically short and have smooth outlines with tapering ends
Achalasia
Achalasia is a neuromuscular abnormality resulting in failure of relaxation at the cardiac
sphincter, which presents at barium swallow examination as a smooth, tapered narrowing,
always at the lower end of the oesophagus .
There is associated dilatation of the oesophagus, which often shows absent peristalsis. The
dilated oesophagus usually contains food residue and may be visible on the plain chest
radiograph.
The lungs may show consolidation and bronchiectasis from aspiration of the oesophageal
د.منى
\
radiology L3
contents.
The stomach gas bubble is usually absent because the oesophageal contents act as a water
seal, but this sign is not diagnostic of achalasia as it is seen in other causes of oesophageal
obstruction and can occasionally be observed in healthy people.
Corrosive strictures
Corrosive strictures are the result of swallowing corrosives such as acids or alkalis. They are
long strictures that begin at the level of the aortic arch.
As with other benign strictures, they are usually smooth with tapered ends on barium swallow
examinations, but may be irregular
Benign tumours
Leiomyomas cause a smooth, rounded indentation into the lumen of the oesophagus.
A soft tissue mass may be seen in the mediastinum indicating extraluminal extension.
Other medistinal masses
Mediastinal masses (e.g. lymphadenopathy secondary to lymphoma or lung cancer) can cause
extrinsic compression and narrowing of the oesophagus.
Anomalous right subclavian artery
An anomalous right subclavian artery, which, instead of coming from the innominate artery,
arises as the last major branch from the aortic arch, gives rise to a characteristic short, smooth
narrowing as it crosses behind the upper oesophagus .
Dilatation of the oesophagus
There are two main types of oesophageal dilatation –
obstructive and non-obstructive:
د.منى
\
radiology L3
• Dilatation due to obstruction is associated with a visible stricture. The patient with a carcinoma
usually presents with dysphagia before the oesophagus becomes very dilated. On the other hand,
a markedly dilated oesophagus indicates a very longstanding condition, usually achalasia or
occasionally a benign stricture.
• Dilatation without obstruction occurs in scleroderma. The disease involves the oesophageal
muscle, resulting in dilatation of the oesophagus, which resembles an inert tube with no peristaltic
movement so that barium does not flow from the oesophagus into the stomach unless the patient
stands upright.
Other abnormalities of the oesophagus
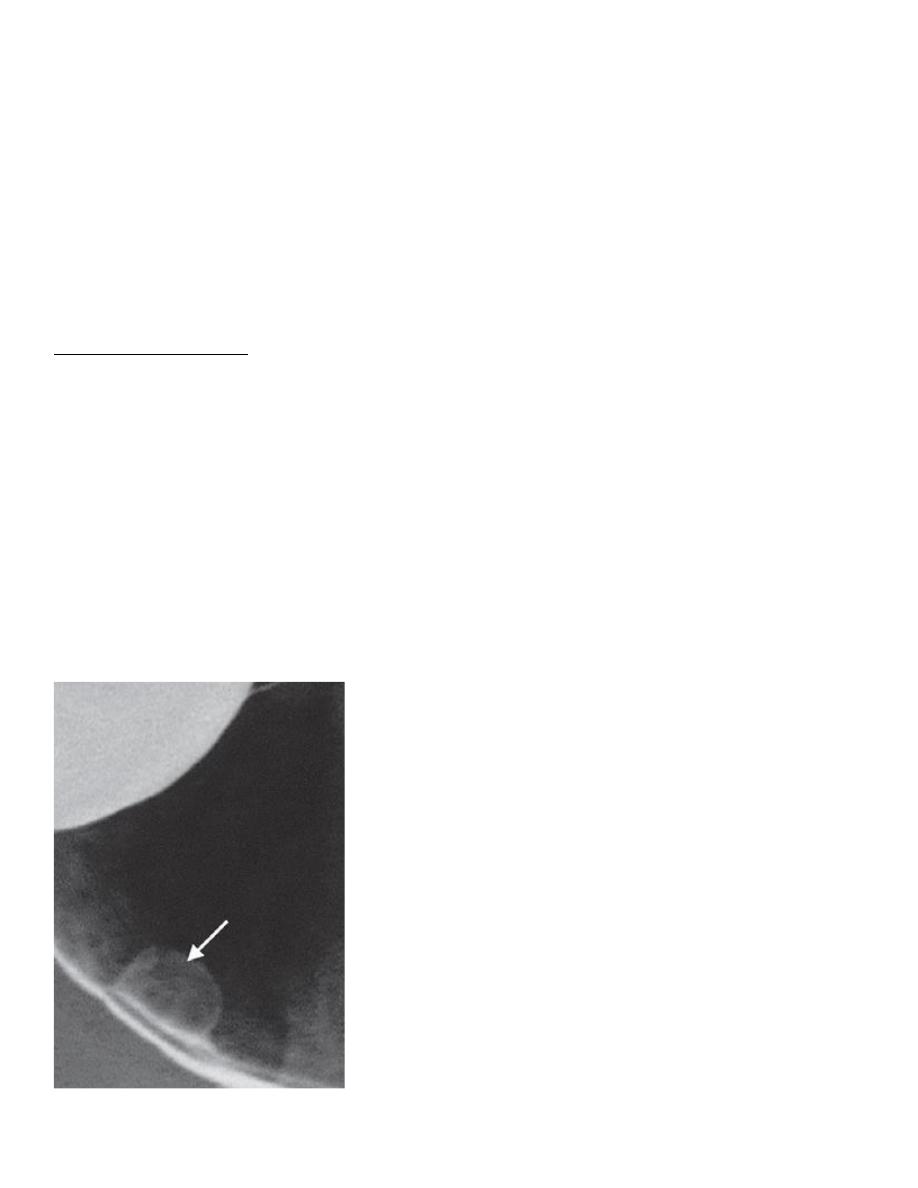
1. An oesophageal web is a thin, shelf-like projection arising from the anterior wall of the cervical
portion of the oesophagus and can only be seen when the oesophagus is full of barium . A web
may be an isolated finding, but the combination of a web, dysphagia and iron deficiency
anaemia is known as Plummer–Vinson syndrome.
2. Oesophageal diverticula are saccular outpouchings, which are often seen as chance findings, in
the intrathoracic portion of the oesophagus. One type of diverticulum, the pharyngeal pouch
or Zenker’s diverticulum is important as it may give rise to symptoms caused by retention of
food and pressure upon the oesophagus. A pharyngeal pouch arises through a congenital
weakness in the inferior constrictor muscle of the pharynx and comes to lie behind the
oesophagus near the midline. It may reach a very large size and can cause displacement and
compression of the oesophagus.
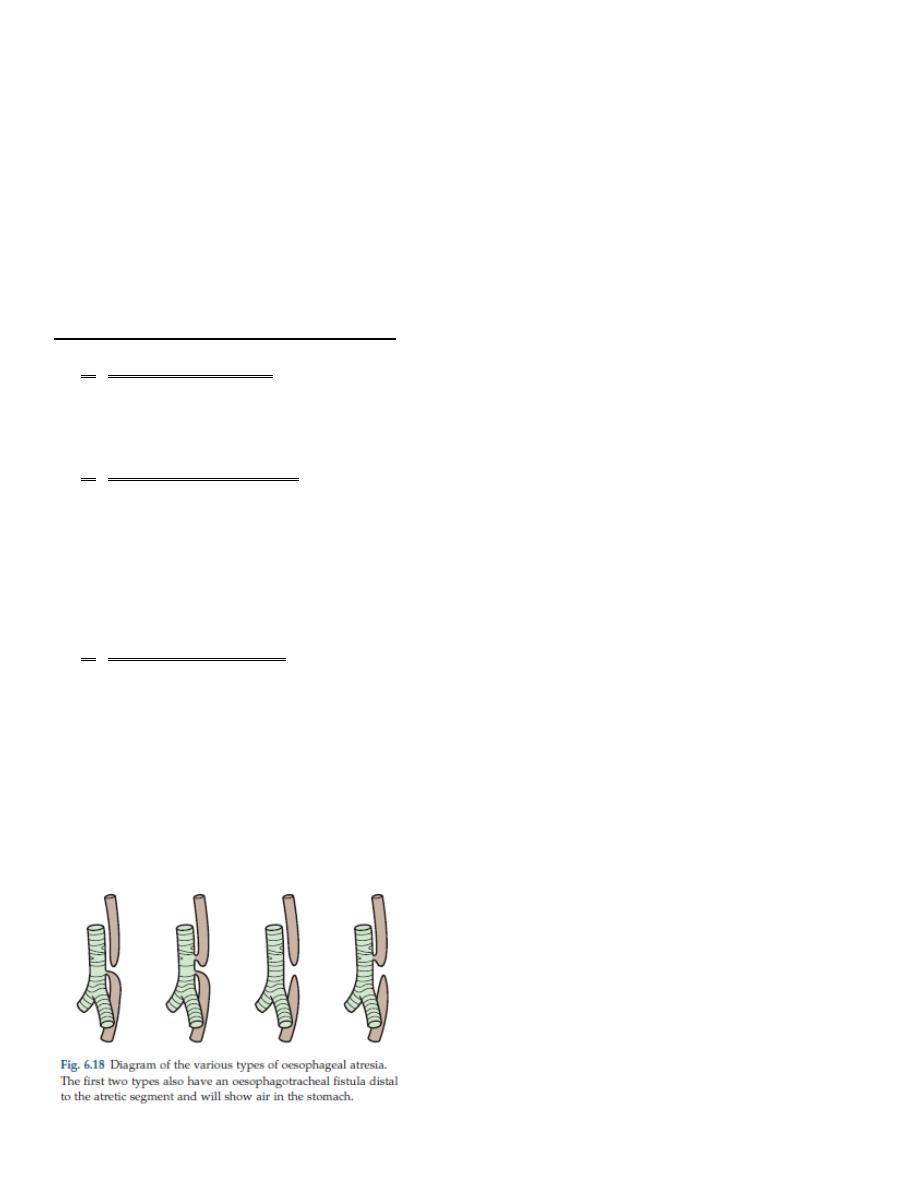
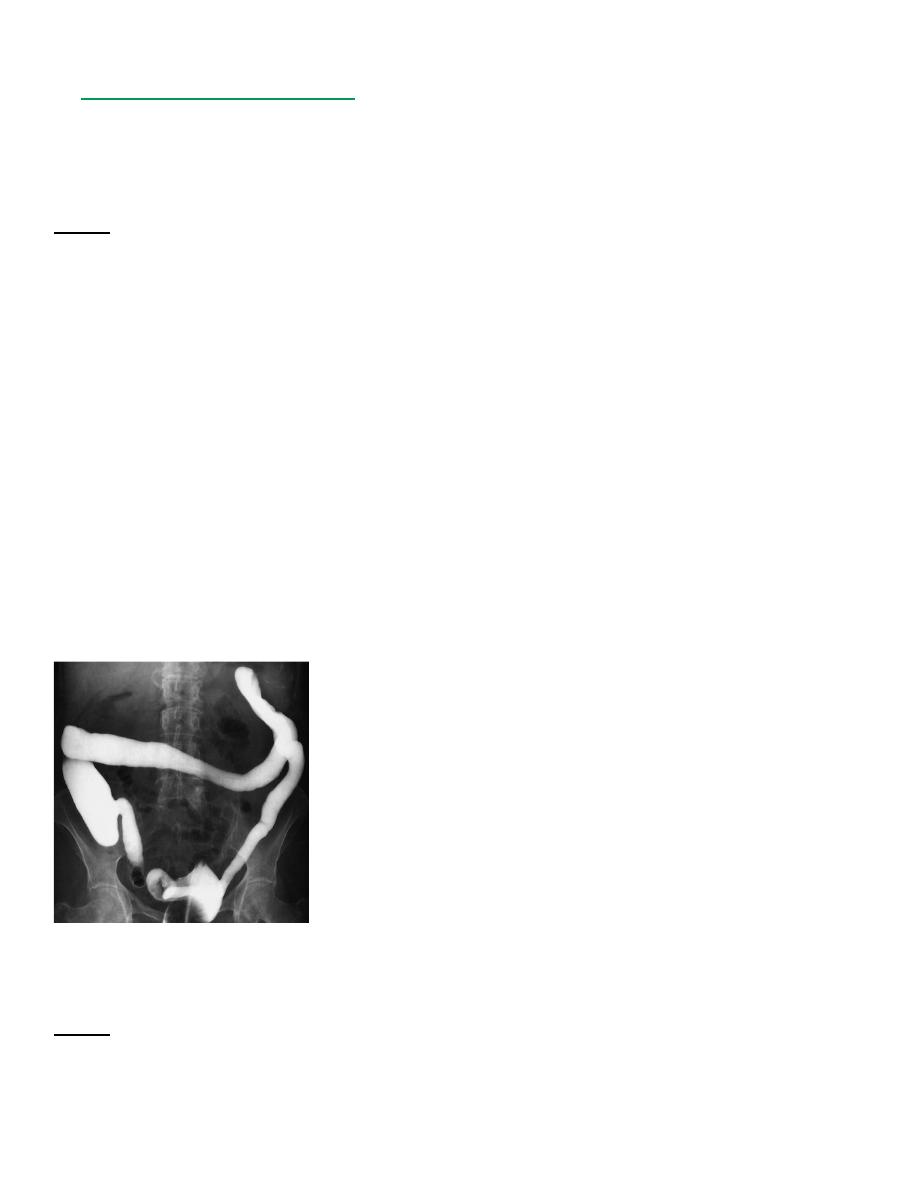
3. In oesophageal atresia, the oesophagus ends as a blind pouch in the upper mediastinum.
Several different types exist , but the most frequent is for the upper part of the oesophagus to
be a blind sac with a fistula between the lower segment of the oesophagus and the
tracheobronchial tree. A plain abdominal film will show air in the bowel if a fistula is present
between the tracheobronchial tree and the oesophagus distal to the atretic segment. The
diagnosis of oesophageal atresia is made by passing a soft tube into the oesophagus and
showing that the tube holds up or coils in the blind-ending pouch. The use of contrast agents is
potentially dangerous because the contrast may cause respiratory problems if it spills over into
the trachea.
د.منى
\
radiology L3
STOMACH AND DUODENUM
Imaging techniques
Barium meal examination
Barium meal examination is now rarely performed as it has been superseded by endoscopy.
The stomach is distended with a gas-producing agent, and an intravenous injection of a short-
acting smooth muscle relaxant is often given. The patient drinks about 200 mL of barium. Films
are taken in various positions with the patient both erect and lying flat, so that each part of the
stomach and duodenum is shown distended by barium and also distended with air but coated
with barium to show the mucosal pattern
The duodenal cap or bulb arises just beyond the short pyloric canal, and the duodenum forms a
loop around the head of the pancreas to reach the duodenojejunal flexure.
Diverticula arising beyond the first part of duodenum are a common finding and are usually
without clinical significance
have an important role in functional studies of the upper GI tract or to evaluate any potential
anastomotic leak For this reason it is usually water-soluble contrast agents that are used, which
are more rapidly resorbed than barium and importantly will allow timely subsequent imaging
with CT.
Computed tomography
Firstly, the patient must not eat for 6 hours prior to the CT to ensure that no food residues
remain in the stomach, which could obscure or mimic disease.
The patient is usually given about 100 mL of tap water to drink (acting as a negative contrast)
as well as a smooth muscle relaxant, in order to distend the stomach and duodenum. If the
stomach is not distended during the scan, any thickening of the gastric wall could be
misinterpreted as being a mass. During the scan, intravenous iodinated contrast medium is
injected to demonstrate enhancement of both the normal structures as well as to distinguish
the enhancement characteristics of any abnormality.
د.منى
\
radiology L3
Upper GI endoscopy is widely used as the initial investigation in patients with possible disease
of the stomach and duodenum.
It enables the mucosa of the stomach and duodenum to be directly inspected and biopsied.
Indications for contrast studies of the stomach and
duodenum
1. Failed gastroscopy
2. Assessment of duodenal strictures that cannot be characterized or navigated on endoscopy
3. Assessment of functional patency/gastric emptying following gastroenterostomy or anti-
obesity surgery
4. To confirm or rule out anastomotic leak following gastric surgery (a water-soluble contrast
agent)
5. Staging tumors discovered by endoscopy
Upper GI endoscopy is widely used as the initial investigation in patients with possible disease
of the stomach and duodenum.
It enables the mucosa of the stomach and duodenum to be directly inspected and biopsied.
Indications for upper gastrointestinal (GI) endoscopyDiagnosis and follow-up
1. Peptic ulcer disease
2. Haematemesis and melaena
3. Dyspepsia and dysphagia
4. Barrett’s oesophagus
5. Biopsies
6. Coeliac disease
7. Confirmation and follow-up of malignant tumours
8. Therapeutic
9. Injection/clipping/banding to stop bleeding from ulcers or
10. oesophageal varices
11. Removal of ingested foreign bodies
12. Stenting of upper GI strictures
13. Feeding tube placement
د.منى
\
radiology L3
Specific diseases of the stomach and duodenum
Peptic ulcer
Gastric ulcers may be benign or malignant so confirmation at gastroscopy is routinely
undertaken, whereas duodenal ulcers are almost invariably benign.
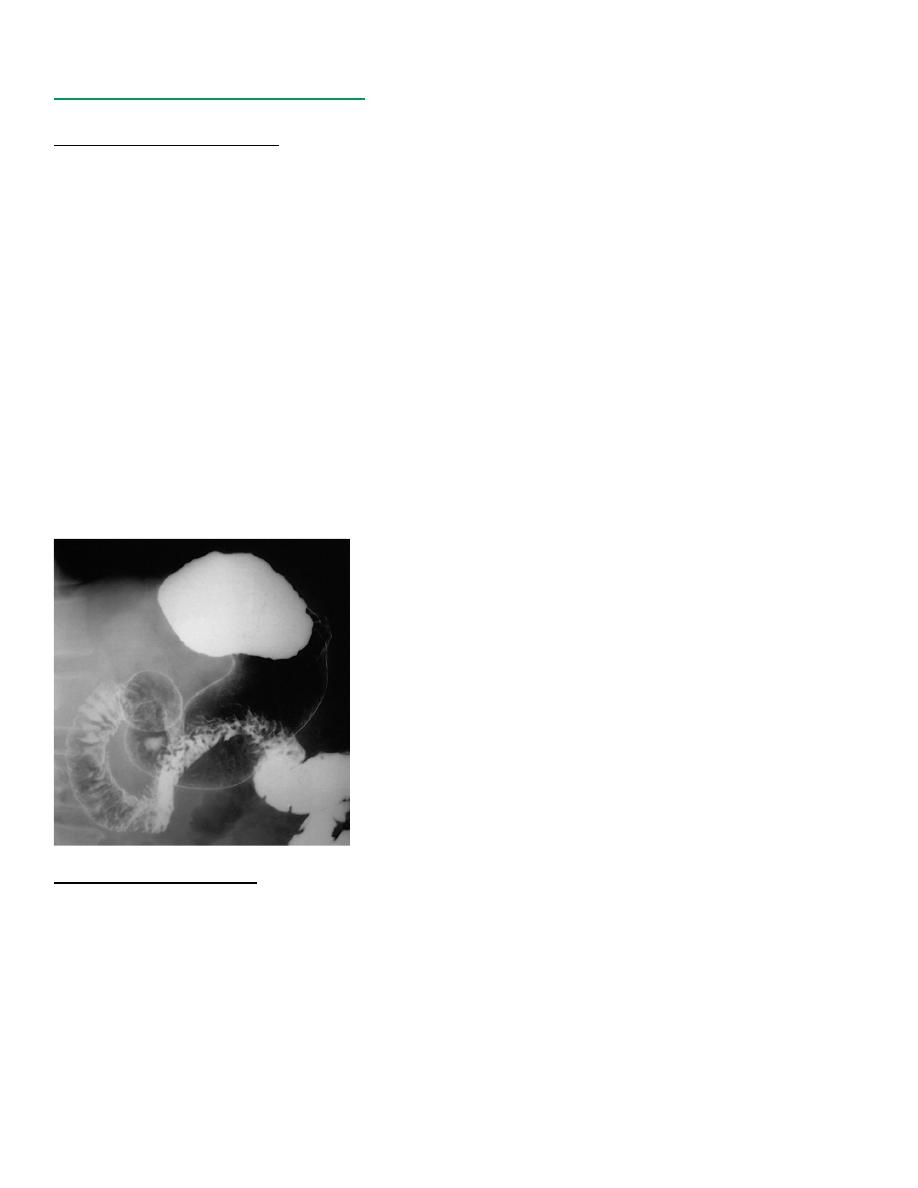
Ulcers are identified as projections of barium beyond the mucosal profile. With duodenal
ulceration, the duodenal cap (bulb) may be very deformed by scarring
Gastric carcinoma
However, gastroscopy has now almost completely taken over the diagnosis of Ca.
At barium examination, gastric carcinoma typically produces an irregular filling defect with
alteration of the normal mucosal pattern
Computed tomography is the main imaging modality for the preoperative staging of patients
with gastric cancer as it can show the extent of the primary tumour but also any distant disease
EUS may be used in some cases for local staging and patients will undergo staging laparoscopy
prior to curative surgery.
FDG-PET/CT does not have a clear role in the primary staging of gastric cancer due to the
normal uptake of FDG by the gastric mucosa.
Gastrointestinal stromal tumours (GISTs)
arise from the wall of the stomach resulting in a smooth, round, submucosal filling defect,
which may ulcerate as the tumour enlarges
GISTs are a group of tumours that are usually benign and well differentiated; they may occur
anywhere in the GI tract but 60–70% occur in the stomach.
د.منى
\
radiology L3
A leiomyoma is a submucosal tumour which, as well as projecting into the lumen of the
stomach, may have a large extraluminal extension that can be easily recognized at CT.
Neuroendocrine tumours of the stomach and duodenum include gastric carcinoid tumours and
gastrinomas.
Gastrointestinal carcinoid tumours can be found anywhere in the GI tract, particularly the
appendix, but can be found incidentally in the stomach often as multiple small (<1 cm)tumours
on a background of pernicious anaemia/chronic atrophic gastritis. Occasionally they are seen in
association with MEN (multiple endocrine neoplasia) type 1 in association with other endocrine
tumours, or as a solitary larger tumour (>3 cm) where they can cause local symptoms of
abdominal pain and bleeding as well as the carcinoid syndrome.
Gastrinomas usually secrete gastrin, resulting in increased gastric acidity and peptic ulceration.
Gastrinomas are often very small and typically enhance brightly in the arterial phase
Gastric polyps
Gastric polyps may be single or multiple.
They may be sessile or have a stalk.
Even with high quality radiographs it is often impossible to distinguish benign from malignant
polyps.
For this reason, gastroscopy with biopsy or operative removal is invariably carried out on all
suspected polyps.
Other intraluminal defects within the stomach include food or blood following a
haematemesis. Sometimes ingested fibrous material, such as hair, may intertwine forming a
ball or bezoar
Lymphoma
The stomach is the most frequent site of lymphoma involving the GI tract, either as primary
disease or by infiltration from adjacent nodes.
The appearance of primary gastric lymphoma is typically of an extensive area of diffuse
thickening of the gastric wall
There may be extensive, bulky lymphadenopathy adjacent to the tumour.
The appearance may mimic gastric carcinoma.
د.منى
\
radiology L3
Gastric outlet obstruction
In infants, pyloric stenosis is by far the commonest cause of gastric outlet obstruction. Often,
the diagnosis is made clinically and can be confirmed with ultrasound, which has superseded
barium meal.
Ultrasound shows a thickened, elongated pyloric canal
Causes of gastric outlet obstruction
Chronic duodenal ulceration: the diagnosis depends on demonstrating a very deformed,
stenosed duodenal cap. It
may or may not be possible to identify an actual ulcer crater
Carcinoma of the antrum
Duodenal, ampullary and pancreatic carcinoma
Acute or chronic pancreatitis, including pseudo cyst formation
Poor functional patency of a gastroenterostomy
Pyloric stenosis in infants
Hiatus hernia
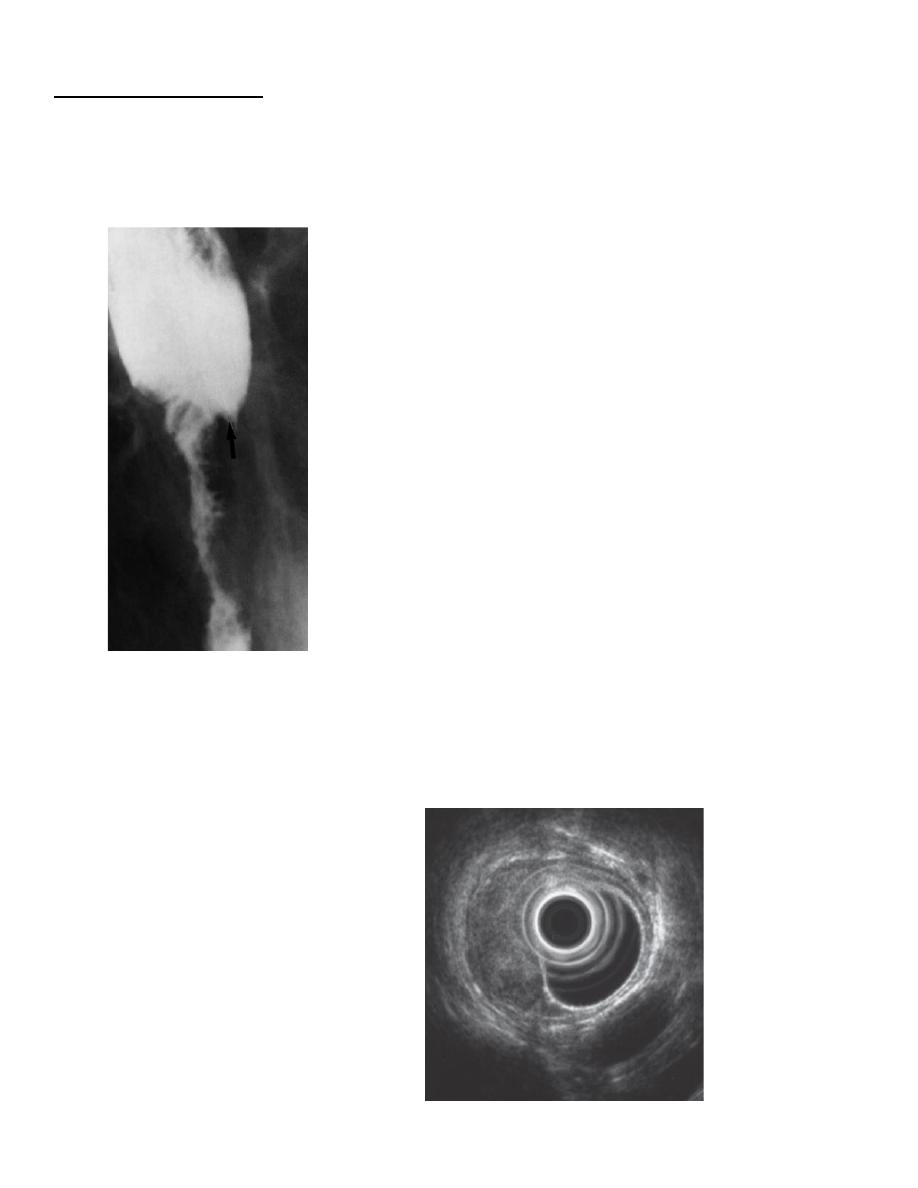
A hiatus hernia is a herniation of the stomach into the mediastinum through the oesophageal
hiatus in the diaphragm.
It is a common finding.
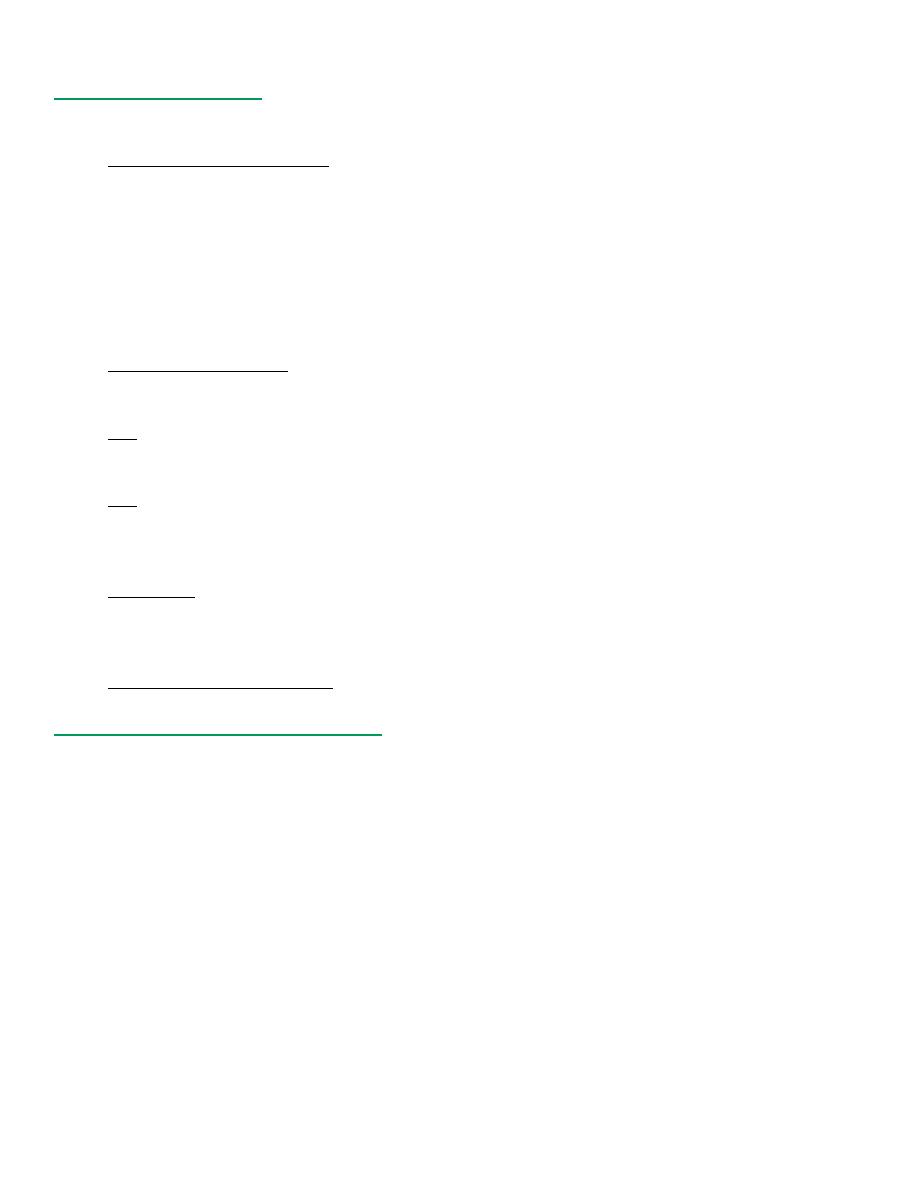
Two main types of hiatus hernia exist: sliding and rolling.
An alternative name for a rolling hernia is ‘para-oesophageal’
The commoner type is the sliding hiatus hernia, where the gastro-oesophageal junction and a
portion of the stomach are situated above the diaphragm The cardiac sphincter is usually
incompetent, so reflux from the stomach to the oesophagus occurs readily and this may cause
oesophagitis, ulceration or peptic stricture. A small sliding hernia may be demonstrated in
most people during a barium meal examination, provided that enough manoeuvres have been
undertaken to increase intra-abdominal pressure. It is, therefore, difficult to assess the
significance of a small hernia with little or no reflux.
In a rolling or para-oesophageal hernia, the fundus of the stomach herniates through the
diaphragm, but the oesophagogastric junction often remains competent below the diaphragm.
A large hernia, particularly one of the para-oesophageal type, may not be reduced when the
patient is in the erect position. In these instances the hiatus hernia will be seen on chest films
and on CT
د.منى
\
radiology L3
SMALL INTESTINE
Imaging techniques
Standard imaging techniques and their indications are:
Small bowel follow-through (small bowel meal)
Indications for small bowel follow-through
1. Inflammatory bowel disease (Crohn
’s disease)
2. Suspected stricture
3. Malabsorption
4. Enterocutaneous fistulae
5. Post small bowel resection, to assess small bowel length, in short bowel syndrome
6. Malrotation
Computed tomography
has a role in the assessment of small bowel disease as it can show
thickening of the bowel wall, an important sign of inflammatory bowel disease and lymphoma,
and occasionally mucosal irregularity and small bowel neoplasms.
***
The patient fasts for 4
–6 hours prior to the procedure and then may be given oral
Gastrografin or water to delineate the small bowel. In some cases, an intravenous bowel relaxant
is injected.
***
CT enteroclysis may also be performed with contrast being infused into the small bowel via
a nasoduodenal tube, followed by CT. Intravenous iodinated contrast medium is injected to
demonstrate vessels and enhancing structures.
Ultrasound
Demonstrate small bowel thickening and free fluid associated with inflammatory conditions, and can
demonstrate a thickened appendix suggestive of appendicitis and occasionally the presence of an
intussusception.
Magnetic resonance imaging
for assessment
Normal appearances of the small bowel
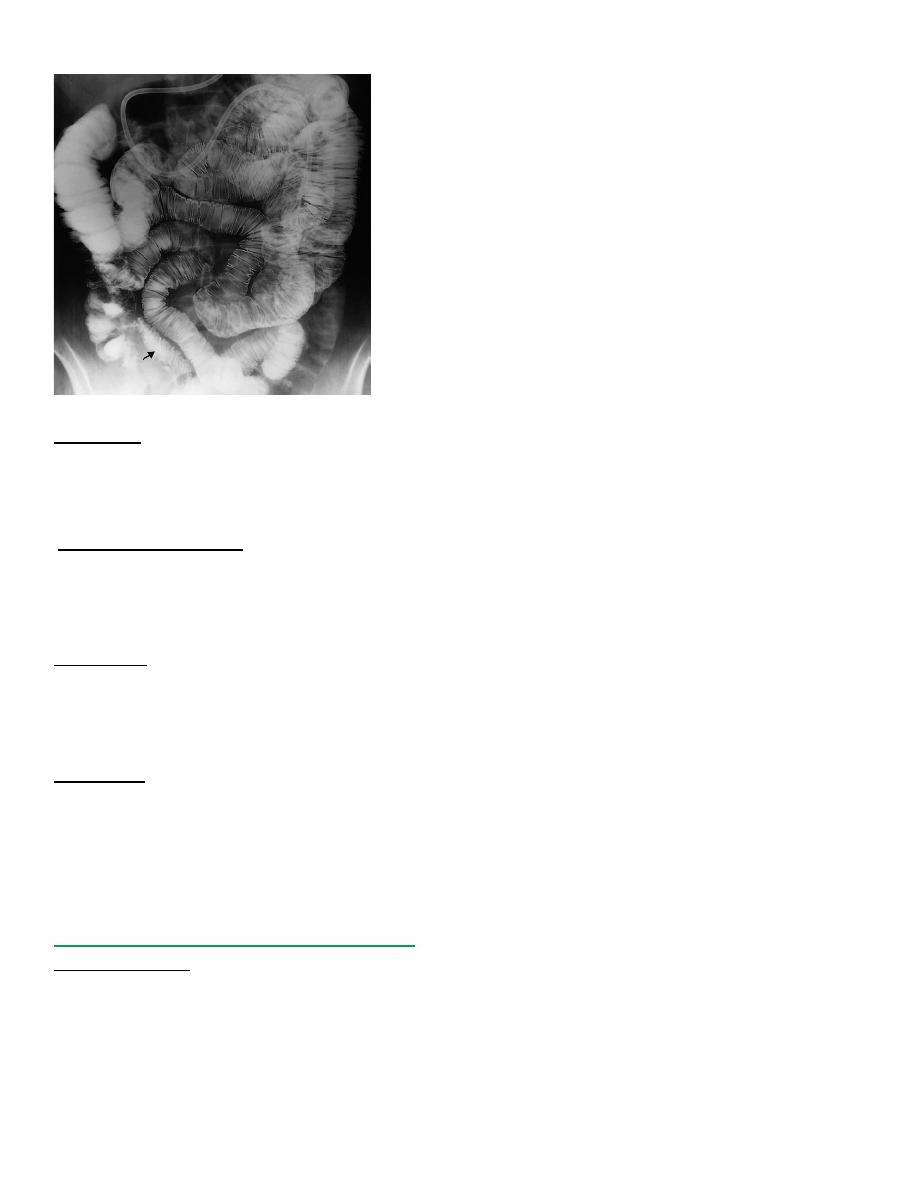
The normal small intestine occupies the central and lower abdomen, usually framed by the
colon.
The terminal portion of the ileum enters the medial aspect of the caecum through the ileocaecal
valve. As the terminal ileum may be the first site of disease
The barium forms a continuous column defining the diameter of the small bowel, which is
normally not more than 25 mm ( 3 cm)
Transverse folds of mucous membrane project into the lumen of the bowel and barium lies
between these folds, which appear as lucent filling defects of about 2
–3 mm in width.
The mucosal folds are largest and most numerous in the jejunum and tend to disappear in the
lower part of the ileum On CT, the small bowel is seen as multiple loops usually containing oral
water or contrast medium.
The lumen of each loop should not exceed 25 mm.
The wall of the small bowel may not be properly assessed unless the small bowel is
distendedplanes.
د.منى
\
radiology L3
Imaging signs of disease of the small intestine
Dilatation
Dilatation usually indicates malabsorption, paralytic ileus or small bowel obstruction . A diameter over
30 mm is definitely abnormal, but it is important to make sure that two overlapping loops are not being
measured
Mucosal abnormality
The mucosal folds become thickened in many conditions (e.g. malabsorption states, oedema or
haemorrhage in the bowel wall) and when inflamed or infiltrated
As mucosal fold thickening occurs in many diseases, it is not possible to make a particular diagnosis
unless other more specific features are present.
Narrowing
The only normal narrowings are those caused by peristaltic waves. They are smooth, concentric and
transient, with normal mucosal folds traversing them and normal bowel proximally. The common
causes of strictures are Crohn
’s disease , tuberculosis and lymphoma. Strictures do not contain normal
mucosal folds and usually result in dilatation of the bowel proximally.
Ulceration
The outline of the small bowel should be smooth apart from the indentation caused by normal mucosal
folds.
Ulcers appear as spikes projecting outwards, which may be shallow or deep .
Ulceration is seen in Crohn
’s disease, tuberculosis and lymphoma.
When there is a combination of fine ulceration and mucosal oedema, a
‘cobblestone’ ppearance may be
seen.
Specific diseases of the small intestine
Crohn’s disease
a disease of unknown aetiology of non-specific chronic granulomatous inflammation, which nearly
always affects the terminal ileum. In addition, it may cause disease in several different parts of the
small and large intestine, often leaving normal intervening bowel, the affected parts being known
as skip lesions.
د.منى
\
radiology L3
The major signs on barium examinations and crosssectional
Imagin
g
1. Strictures, which are extremely variable in length. Sometimes a loop of bowel is so narrow,
either from spasm or oedema and fibrosis in the bowel wall, that its appearance has been called
the
‘string sign’.
2. Contraction of the caecum, which may be seen particularly when there is visible disease in the
terminal ileum.
3. Dilatation of the bowel, which may be seen proximal to narrowed areas.
4. Ulcers; these are sometimes quite deep. Fine ulceration combined with mucosal oedema gives
rise to the so-called
‘cobblestone’ appearance.
5. Thickening, distortion or effacement of mucosal folds.
6. Separation of loops of bowel, due to bowel wall thickening or an inflammatory mass.
7. Fistulae to other small bowel loops, colon, bladder or vagina . When the fistula is between
adjacent loops of small intestine it can be difficult to detect.
8. Signs of malabsorption
Imaging :
1. Ultrasound may identify thickened loops of bowel, abscess collections in the lower
abdomen
2. CT, have a thick-walled appearance with streaky, high density of the surrounding mesenteric fat
due to surrounding oedema and inflammatory change.
When Crohn
’s disease affects the anal canal, a perianal fistula often results.
3. MRI is often used to demonstrate the position and extent of the fistula.
Small bowel ischaemia
Intestinal infarction, a serious life-threatening condition, is caused by occlusion of the superior
mesenteric artery, either due to a thrombosis or an embolus .
There may be thickening and oedema of the wall of the small bowel, and gas may be seen within the
bowel wall.
Perforation may occur, with free gas seen within the peritoneal cavity. There may be air within the
superior mesenteric vein or portal vein system in severe cases. These features are best demonstrated on
a post contrast CT, performed in the arterial and portal venous phase, which will also demonstrate the
arterial anatomy.
Tuberculosis
Tuberculosis of the small bowel is indistinguishable from Crohn
’s disease on barium examination.
It commonly affects the ileocaecal region and also causes contraction of
the caecum.
On CT, there may be signs of diffuse peritoneal involvement, with ascites, thickening of the omentum,
peritoneal and serosal nodules, and lymph node enlargement.
These appearances may be indistinguishable from a disseminated intraperitoneal malignancy and
ultrasound
or CT-guided biopsy is usually required to establish the
diagnosis.
Lymphoma
The infiltration in the wall of the bowel with lymphoma ,extremely difficult to distinguish
from Crohn
’s disease. Features that may help differentiate the two conditions on barium examinations
are
د.منى
\
radiology L3
small mucosal filling defects due to tumour nodules and displacement of loops caused by enlarged
mesenteric lymph nodes. Enlargement of the liver and spleen may also be present.
CT and ultrasound can show very marked thickening of the bowel wall, which can help differentiate
between Crohn
’s disease and lymphoma.
CT can also demonstrate mesenteric and para aortic lymphadenopathy and lymphomatous deposits in
the liver and spleen.
Malabsorption
A number of disorders result in defective absorption of Foodstuffs, minerals or vitamins. The definitive
test for malabsorption is jejunal biopsy.
The following imaging signs may occur with any of the causes of malabsorption
• Small bowel dilatation, the jejunum being affected more than the ileum.
• Thickening of mucosal folds.
• The barium may be diluted by the excessive fluid in the small bowel and so appears less dense.
The use of barium follow-through in malabsorption is mainly confined to demonstrating a structural
abnormality causing the malabsorption, notably:
• Crohn’s disease.
• Lymphoma.
• Anatomical abnormalities, e.g. decreased length of small bowel available for absorption, such as
surgical resection or a fistula short-circuiting a length of small bowel.
• Stagnation of bowel contents, allowing bacterial overgrowth, which utilizes nutrients from the bowel
lumen, caused by:
– multiple small bowel diverticula (Fig. 6.48)
– a dilated loop cut off from the main stream of the
bowel in which there is delayed filling and emptying
(blind loop)
– a dilated loop proximal to a stricture (stagnant loop).
Acute small bowel obstruction
1. peritoneal adhesions (usually postoperatively or following previous peritoneal inflammation),
2. obstruction in hernial orifices, Crohn
’s disease, at the site of twisting in volvulus,
3. occasionally due to metastatic carcinoma, lymphoma or even primary small bowel tumours.
A barium examination is not carried out in most cases of obstruction as the diagnosis is usually made
on clinical history and examination with the help of plain abdominal films.
Water-soluble contrast is used in preference to barium
LARGE INTESTINE
Imaging techniques
Colonoscopy
Colonoscopy is now the gold standard for examining the colonic mucosa and may be used for
diagnostic or therapeutic biopsy or resection of mucosal lesions.
Barium enema
Firstly, the bowel is prepared by means of aperients or washout to rid the colon of faecal
material, which might otherwise mask small lesions and cause confusion by simulating polyps.
Although diverticular disease and colonic carcinoma are well demonstrated at barium enema,
CT pneumocolon is increasingly being used following failed colonoscopy.
د.منى
\
radiology L3
Instant enemas (water-soluble contrast) are still used in suspected large bowel obstruction to
confirm the diagnosis and also to delineate the level of obstruction in a patient who may be
considered for bowel decompression with a colonic stent, prior to surgery
Computed tomography pneumocolon
the method of choice for identifying malignant tumours of the colon when colonoscopy has
failed as it has the advantage of allowing not only the diagnosis of the tumour but also the
demonstration of metastatic disease.
Neither barium nor Gastrografin is used.
three-dimensional display and viewed as
virtual colonoscopy
.
Sigmoidoscopy
is performed in almost every patient in whom a barium enema or CT
pneumocolon is requested, because lesions in the rectum, especially mucosal abnormalities, may
be missed.
Magnetic resonance imaging
Magnetic resonance imaging of the colon is challenging due to movement artefacts from bowel
peristalsis.
MRI is mainly used to evaluate the rectum and anal canal, where movement artefacts are
minimal. No specific patient preparation is required.
Nuclear medicine studies
in patients with chronic constipation.
The presence of inflammation (Ulcerative colitis.)
Normal appearance of the colon
The calibre decreases from the caecum to the sigmoid colon.
The caecum is usually situated in the right iliac fossa, but it may be seen under the right lobe of
the liver or even in the centre of the abdomen if it possesses a long mesentery.
The lips of the ileocaecal valve may project into the caecum and cause a filling defect, which
must not be mistaken for a tumour.
Filling of the terminal ileum and appendix with rectal contrast may occur, but if they do not fill
no significance can be attached to this.
Haustra can usually be recognized in the whole of the colon, although they may be absent in the
descending and sigmoid regions. The outline of the descending colon, apart from the haustra, is
smooth.
Imaging signs of disease of the large intestine
Narrowing of the lumen
Narrowing of the colon may be due pathology:
• inside the lumen of the bowel (e.g. impacted faeces)
• inside the bowel wall (may be due to physiological spasm)
• outside the bowel wall due to compression by an extrinsic mass.
Causes of narrowing of the colonic lumen
1. Carcinoma
2. Diverticular disease
3. Crohn
’s disease
4. Ischaemic colitis
5. Rarer causes:
- Tuberculosis: --lymphogranuloma venereum
—amoebiasis---radiation fibrosis

د.منى
\
radiology L3
Neoplastic strictures
have shouldered edges, an irregular lumen and are rarely more than 6 cm in
length
whereas benign strictures
classically have tapered ends, a relatively smooth outline and may be
of any length.
Ulceration
may be seen in strictures due to Crohn
’s disease, and sacculation of the colon is a
feature of ischaemic strictures.
Narrowing due to diverticular disease
It is sometimes impossible to distinguish a stricture due
to a carcinoma in an area of diverticular disease from a stricture due to diverticular disease.
• The site of the stricture can help in limiting the differential diagnosis. Strictures due to diverticular
disease are almost always confined to the sigmoid colon. Ischaemic strictures are usually centred
somewhere between the splenic flexure and the sigmoid colon. Crohn
’s disease and tuberculosis have a
predilection for the caecum.
Extrinsic compression
by a mass arising outside the wall of the bowel causes a smooth
narrowing of the colon at barium enema examination, frequently from one side only, and often
displaces the colon, e.g. ovarian and uterine masses. Extrinsic compression causing a smooth
indentation on the caecum may be seen with a mucocele of the appendix, appendix abscess or an
inflammatory mass in Crohn
’s disease.
Dilatation
Double-contrast barium enema and CT pneumocolon examinations both involve distending the
colon
The causes of dilatation of the colon are:
1.
Obstruction.
2.
Paralytic ileus.
3.
Volvulus
.
4.
Ulcerative colitis
with toxic dilatation
5.
Hirschsprung
’
s disease
and
megacolon
.
Filling defects
1. Filling defects in the colon, as elsewhere in the GI tract, may be intraluminal, arise from the wal
or be due to pressure from an extrinsic mass.
2. A localized filling defect is likely to be a polyp or a neoplasm.
3. Faeces cause a filling defect which can be very difficult to distinguish from a polyp or tumour
Faeces have no attachment to the wall of the bowel, are completely surrounded by barium or air,
and move according to the position of the patient
4. Intramural haemorrhage, oedema or air in the wall of the colon (pneumatosis coli) all cause
multiple, smooth filling defects arising from the wall of the bowel.
5. A unique type of filling defect is seen in intussusceptions.
Ulceration
Ulcers of the colonic mucosa can be recognized on barium enema as small projections from the
lumen into the wall of the bowel, causing the normally smooth outline of the colon to have a
fuzzy or shaggy appearance
The two major causes of ulceration are ulcerative colitis and Crohn
’s disease. Rarer causes
include tuberculosis and amoebic and bacillary dysentery.
د.منى
\
radiology L3
Specific diseases of the colon
Ulcerative colitis
Ulcerative colitis is a disease of unknown aetiology characterized by inflammation and ulceration of
the colon. The disease always involves the rectum. When more extensive it extends in continuity
around the colon, sometimes affecting the whole colon.
Signs :
1. The cardinal radiological sign is widespread ulceration The ulcers are usually shallow, but in
severe cases may be quite deep.
2. In all but the milder cases, there is loss of the normal colonic haustra in the affected portions of
the colon.
3. Oedema of the perirectal tissues causes widening of the space between the sacrum and the
rectum.
4. Narrowing and shortening of the colon, giving the appearance of a rigid tube,
5. in advanced disease Pseudopolyps are small filling defects projecting into the lumen of the
bowel, formed by swollen mucosa in between the areas of ulceration.
6. Strictures are rare, and, when present, are likely to be due to carcinoma; the incidence of colonic
carcinoma in longstanding ulcerative colitis is significantly increased.
7. On CT, the bowel wall may be thickened.
8. In chronic ulcerative colitis there is visible fatty infiltration in the submucosa, resulting in a
‘target sign’ appearance.
9. When the whole colon is involved, the terminal ileum may become dilated. As the ileocaecal
valve in this situation is incompetent,
10. Toxic dilatation (toxic megacolon) is a serious complication
11. Barium enema and CT pneumocolon should be avoided in the presence of toxic dilatation
owing to the risk of perforating the colon, a contraindication that also applies to colonoscopy.
Crohn
’
s disease
chronic granulomatous condition of unknown aetiology, which may affect any part of the GI tract, but
most frequently involves the lower ileum and the colon. The colon may be the only part of the
alimentary tract to be involved, but usually the disease affects the small bowel if the colon is involved.
Signs :
1. At an early stage in the disease, the findings at barium enema are loss of haustration,
2. narrowing of the lumen of the bowel
3. shallow ulceration.

د.منى
\
radiology L3
4. This criss-crossing ulceration combined with mucosal oedema may give rise to a
‘cobblestone’
appearance of the mucosa
Later,the ulcers become deeper and may track in the submucosa
5. The ulcers may be very deep, penetrating into the muscle layer, when they are described as
‘rose-thorn ulcers’ or deep fissures.
6. The deep ulceration in Crohn
’s disease may lead to the formation of intra- and extramural
abscesses.
7. Fistulae are an important complication.
8. The additional features visible at CT are thickening of the bowel wall, strands in the surrounding
fat, fistulae and extracolonic fluid collections.
9. Strictures are a common finding in Crohn
’s disease
10. The disease is not always circumferential; one of the features that distinguish it from ulcerative
colitis is that it may involve only one portion of the circumference of the bowel.
11. Another important diagnostic feature is the presence of the so-called
‘skip lesion’, namely areas
of disease with intervening normal bowel. Skip lesions are virtually diagnostic of Crohn
’s
disease. However, the entire colon may be involved or the disease may be limited to just one
segment.
12. There is a predilection for the caecum and terminal ileum.
13. The rectum is often spared
– another important differentiating feature from ulcerative colitis.
14. Fistulae may also occur between the colon and the small bowel, bladder or vagina, which may
be demonstrated on water-soluble contrast studies or MRI
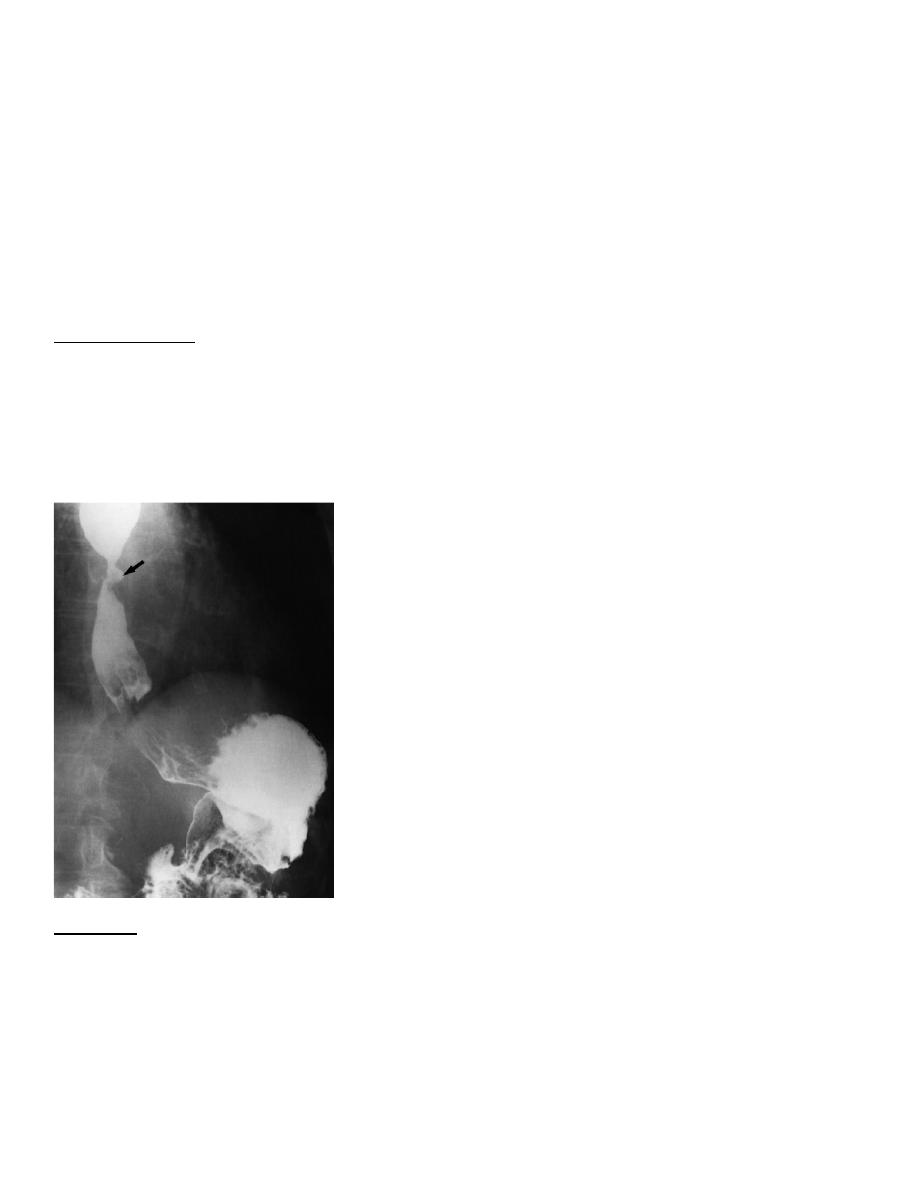
Diverticular disease
sac-like out-pouchings of mucosa through the muscular layer of the bowel wall. They are associated
with hypertrophy of the muscle layer and are probably due to herniation of mucosa through areas of
weakness where blood vessels penetrate the muscle.
Diverticula are very common, particularly in the elderly.
They are seen in all parts of the colon, but are commonest in the sigmoid colon.
The term diverticulitis is used when infection of the affected segment causes symptoms such as
sepsis, diarrhoea or obstruction.
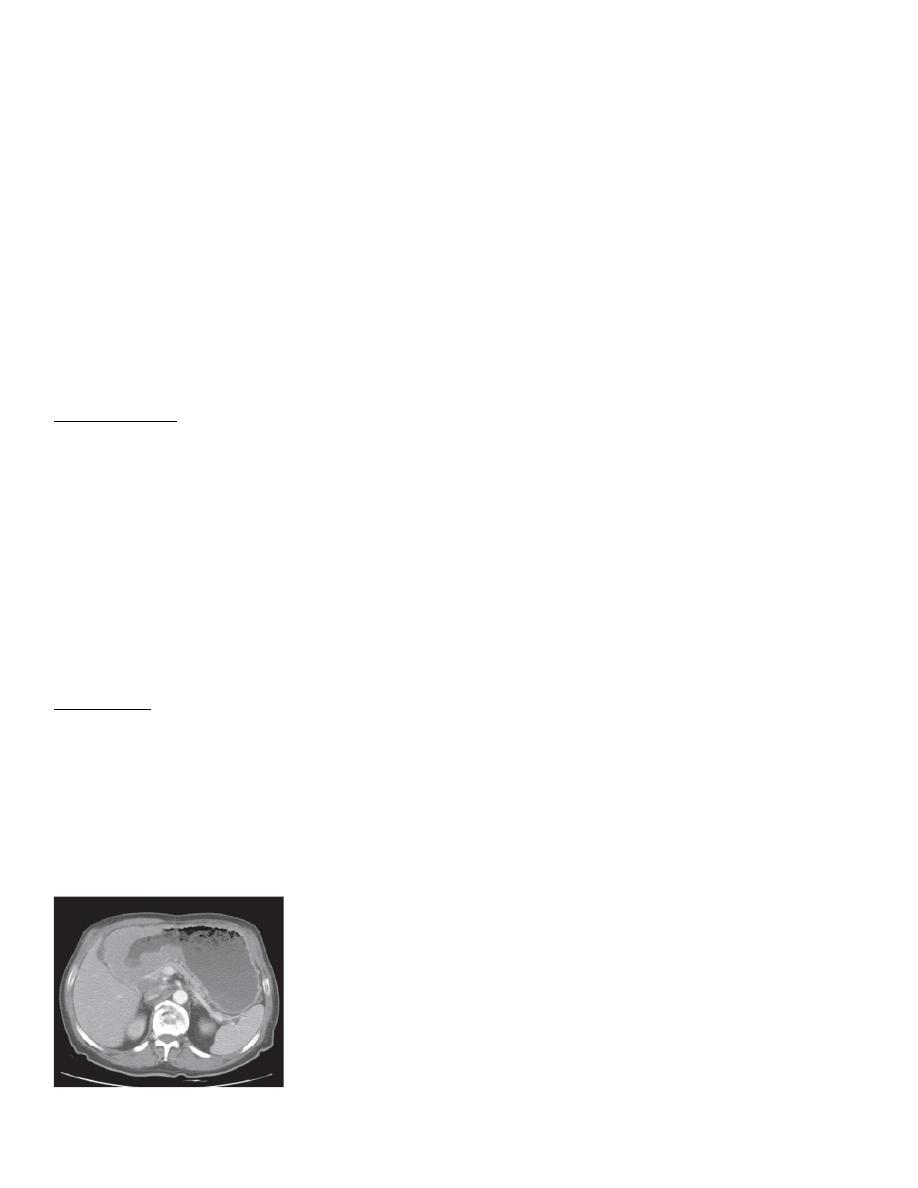
The diverticula, when filled with barium, are seen as spherical out-pouchings with a narrow
neck .

د.منى
\
radiology L3
The colon may also show a
‘saw-tooth’ serrated appearance from hypertrophy of the muscle
coats.
Some diverticula may not fill; when inflammation occludes the necks of the diverticula.
On CT, the affected loop of bowel appears thick-walled and there is stranding of the
surrounding fat due to oedema and inflammatory change .
A diverticulum may perforate, resulting in a pericolic abscess or fistula into the bladder, small
bowel or vagina. This is recognized by noting barium outside the colon, either in the pericolic
region or within the structure to which the fistula has occurred.
An abscess is most readily diagnosed with CT.
Occasionally, diverticula perforate directly into the peritoneal cavity causing peritonitis, and free
intraperitoneal air should be looked for on a plain abdominal film if necessary.
A stricture with or without local abscess formation may occur
Ischaemic colitis
Acute infarction of the large bowel is very rare.
mucosal oedema and haemorrhage, and usually resolve
If suspected, a CT arteriogram is very helpful in not only demonstrating the presence of bowel
abnormalities (e.g. strictures), but
On barium studies, mucosal haemorrhage and oedema may be recognized by observing
multiple, smooth indentations into the lumen of the bowel, resembling thumb prints
If stricture formation occurs, the stricture will be smooth and have tapered ends. The site is
usually, but not always, centred between the splenic flexure and the sigmoid colon because these
are the regions of the colon with the most vulnerable blood supply
Sacculations may be seen arising from one side of the strictured area
د.منى
\
radiology L3
Colorectal tumours
Polyps
means a small mass of tissue arising from the wall of the bowel projecting into the lumen.
They are best investigated by endoscopy, but may be found at barium enema or CT
pneumocolon.
It is often impossible on radiological grounds to exclude frank malignancy in a polyp in an
adult. However, only a tiny minority of polyps less than 1 cm in size, and very few less than 2
cm, are cancers.
The features that suggest malignancy are a diameter of more than 2 cm, a short thick stalk or an
irregular surface.
Polyps may be sessile or on a stalk, single or multiple.
The common polyps are:
Adenomatous polyps
are benign neoplasms but have a predisposition to malignant change.
They are, therefore, removed endoscopically when discovered, regardless of whether or not an
individual polyp is believed to be responsible for symptoms.
found most frequently in the rectosigmoid region.( single or multiple )
In
familial polyposis
they are numerous and one or more will, in time, undergo malignant
change
Villous adenomas
are benign sessile tumours showing a sponge-like appearance owing to
barium trapped between the villous strands. common sites are the rectum and caecum. There is a
high incidence of malignant change.
Polypoid adenocarcinomas
.
Juvenile polyps
. Almost all isolated polyps in children are benign. They are probably
developmental in origin.
Inflammatory polyps (pseudopolyps)
are seen in ulcerative colitis.
Hyperplastic or metaplastic polyps
.
د.منى
\
radiology L3
Carcinoma
Carcinomas may arise anywhere in the colon and rectum but they are commonest in the
rectosigmoid region and caecum.
The appearance and behaviour of a carcinoma in these two sites are usually quite different. The
patient with a rectosigmoid carcinoma often has an annular stricture and presents with alteration
in bowel habit and obstruction, whereas with a caecal carcinoma the tumour can become very
large without obstructing the bowel, so anaemia and weight loss are the common presenting
features.
A barium enema shows annular carcinomas as an irregular stricture with shouldered edges (see
Such strictures are rarely more than 6 cm in length. The polypoid or fungating carcinoma causes
an irregular filling defect projecting into the lumen of the bowel.
Computed tomography particularly CT pneumocolo, recognized as thickening of the bowel
wall and an irregular narrowing of the lumen of the colon.
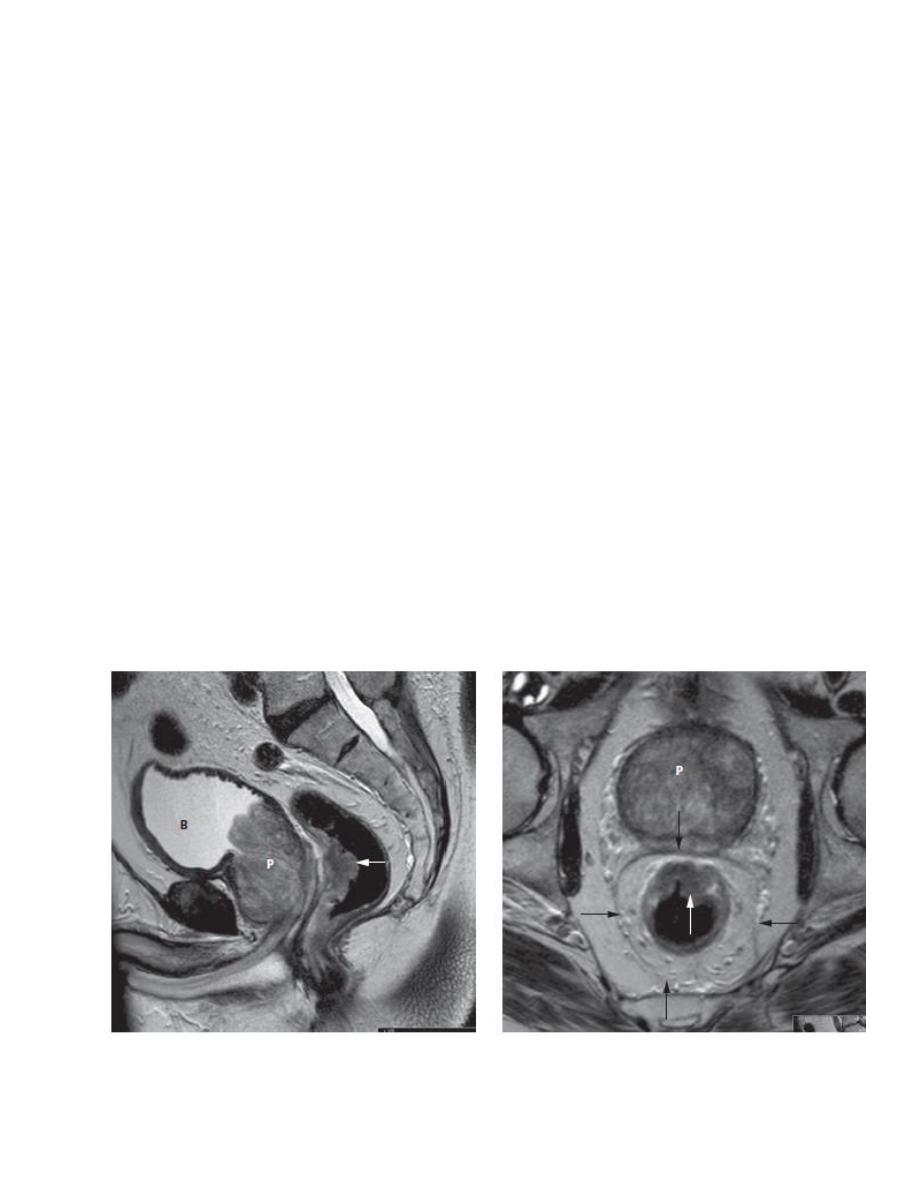
Magnetic resonance imaging is the method of choice for local extent of
rectal carcinoma
. The
mesorectal fascia is an important anatomical landmark as it represents the surgical plane of
dissection during rectal cancer surgery.
Staging colorectal carcinoma
.
CT is used to demonstrate distant metastases to the liver or lungs and to identify para-aortic
nodal disease.
CT can also inform on the local staging of a colonic tumour (e.g. infiltration into abdominal or
pelvic organs) although the definitive extent of local disease may not be known until the time of
surgery
FDG-PET/CT is not currently used routinely for initial staging of colorectal cancer, but it is
more sensitive than CT in the detection of metastatic sites of disease and is used in suspected
recurrent disease in patients who are to be considered for potential curative surgery (e.g. hepatic
resection for liver metastases) to ensure there are no other sites of recurrence.
Noor Rahman
