Dr. Rzan
CONNECTIVE TISSUE DISEASESObjectives:
1- define CT. diseases.2-Identify the common CT. diseases.
The connective tissue diseases are a group of chronic inflammatory disorders that involve multiple body systems and exhibit a wide spectrum of clinical manifestations.Aetiology
Their aetiology is multifactorial and involves:• Genetic,
• Immunological (especially autoantibody production)
• Environmental factors
SYSTEMIC LUPUS ERYTHEMATOSUS
SLE is the most common multisystem connective tissue disease.
It is characterised by a diverse spectrum of autoantibody production.wide variety of clinical features.
The prevalence varies according to geographical and racial background.
Around 90% of affected are women.with peak onset in the second and third decades.
Aetiology andpathogenesis
Autoantibodies production.At least 50 antigen targets for autoantibody production.
polyclonal B- and T-cell activation.
Many autoantigens in SLE are components of the intracellular and intranuclear machinery.
one mechanism may be exposure of intracellular antigens on the cell surface during apoptosis..
Environmental factors that associate with flares of lupus:
1-sunlight and artificial ultraviolet (UV) light.• 2-Pregnancy.
• 3-Infection.
• -increase oxidative stress and subsequent apoptosis
REVISED AMERICAN RHEUMATISM ASSOCIATION CRITERIA FOR S L E
Features
Characteristics
• Malar rash• Discoid rash
• Photosensitivity
• Oral ulcers
Fixed erythema, flat or raised, sparing the nasolabial folds
Erythematous plaques with adherent keratoticscales, scarring and follicular plugging
Rash as a result of unusual reaction to sunlight
Oral or nasopharyngeal ulceration, which may be painless
• 5-Arthritis• 6-Serositis
• 7--Renal disorder
• 8--Neurological disorder
• 9-Haematological disorder
• 10-Immunological disorder
• 11-Antinuclear antibody (ANA)
Non-erosive, two or more peripheral joints.
Pleuritis or Pericarditis
Persistent proteinuria > 0.5 g/day or
Cellular casts
Seizures or psychosis.
Haemolytic anaemia or
Leucopenia2 (< 4 ××109/l), orLymphopenia2 (< 1 ××109/l), or
Thrombocytopenia2 (< 100 ××109/l) in the
Anti-DNA antibodies or antibody to Sm antigen or antiphospholipid antibodies.
Abnormal titre of ANA by immunofluorescence
SLE is diagnosed by presence of 4out of these 11 criteriaMucocutaneous features
It is obvious that 4 of the 11 criteria were mucocutaneous.
20% of all SLE cases present with initial skin manifestations.
50–70% of all SLE patients will eventually show skin symptoms during the course of their disease.
There are three main types OF LE
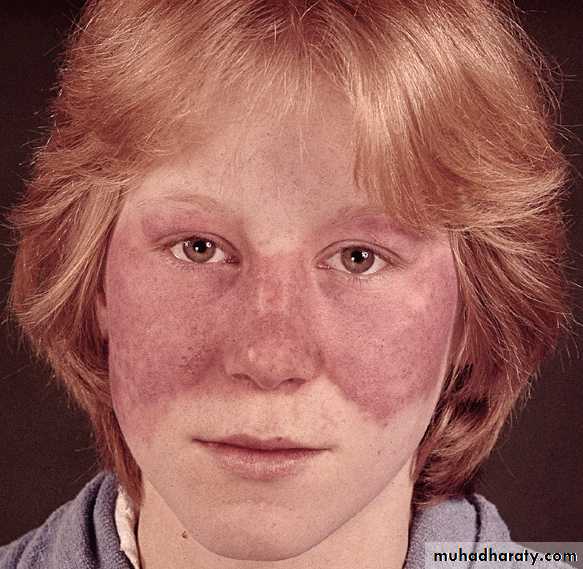
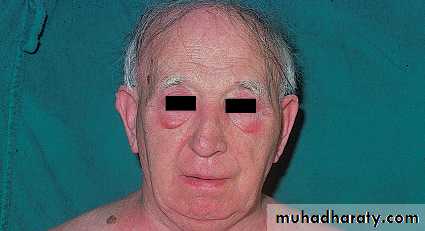
• SLE. (The classic butterfly facial rash)
• Subacute cutaneous lupus erythematosus (SCLE).
• Discoid lupus erythematosus (DLE).
The classic butterfly facial rash of SLE.
(20-30% of patients) is painful or pruritic erythematous plaques and occurs in a photosensitive distribution that involves the cheecks ,nasal bridge and spares the nasolabial folds.• Subacute cutaneous lupus erythematosus (SCLE):
• rashes are migratory nonscarring and either• (psoriasiform)
• or annular
• with characteristic shawl distribution..
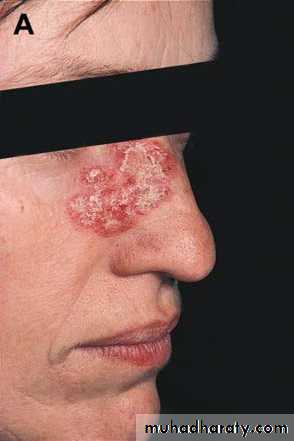
Discoid lupus erythematosus (DLE)
lesions are long-lasting for up to decades.discoid erythymatous scaly plaques with follicular plugging.
the scales are adherent and there removal may leave pits (carpet-tack sign).
healing in an area and continuing in another.
healing occurs with scarring and hypopigmentation.
Scarring alopecia may result if DLE present on the scalp.
The external ear is a predilection sites of DLE.
When DLE lesions are present below the neck line it is concedered as generalised.
Involvement of the scalp leads to cicatricial alopecia
Painful oral ulcers are common in SLE.
Diffuse, non-scarring, alopecia may occur with active diseaseRaynaud's phenomenon.
Vasculitis.
livedo reticularis
periungual erythema.
Examination of nail-fold capillary loops using a dermtoscope may show loss of the normal loop pattern and capillary 'fallout' with haemorrhage and dots.
Differential diagnosis of butterfly rash:
1-SLE.2- rosacea .
3-Polymorphic light eruption.PLE.
4-Seborrhoic dermatitis.
Differential diagnosis of discoid lesion:
1-DLE.
2-DISCOID ECZEMA
3-Tinea.
4-psoriasis (silvery scale).
5-lupus vulgaris (diascopy
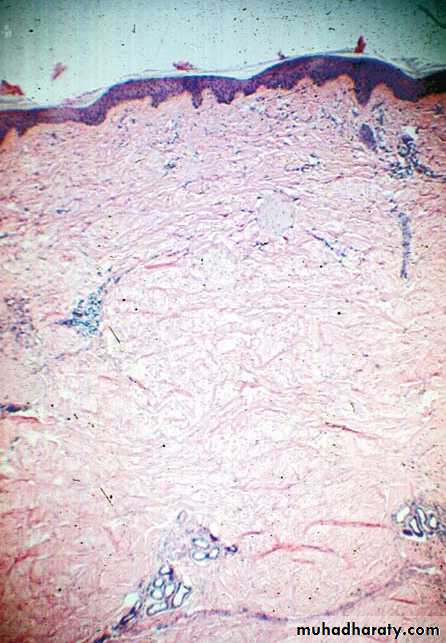
Histological findings
• epidermal hyperkeratosis.• basal cell liquefaction degeneration.
• thickening of the basement membrane.
• mononuclear cell infiltrateat the dermo-epidermal junction ,around blood vessels and adnexial structures.
• Direct Immunofluorescence examination shows granular deposits of mostly IgG, IgM and complement C3 in a continuous line along the dermo-epidermal junction (so-called lupus band ) .
Management
General; avoiding sun and UV light exposure.Topical: potent steroids for skin leasions.
Systemic:
1- Intermittent NSAIDs.
2-Hydroxychloroquine (200-400 mg daily).
3-Short courses of oral corticosteroids for mild to moderate disease activity.
4-Acute or life-threatening disease requires high-dose corticosteroids ( prednisolone 40-60 mg daily or i.v. methylprednisolone 500 mg-1 g) in combination with pulse i.v. cyclophosphamide .
5- immunosuppressive drugs (azathioprine, methotrexate, ciclosporin, tacrolimus, mycophenolate mofetil) are useful either alone or in combination with corticosteroids.
Prognosis
Overall 5-year survival is greater than 90%.Early mortality within 5 years of diagnosis is usually due to organ failure or sepsis.
the late mortality mainly results from premature cardiovascular disease to which chronic corticosteroid therapy contributes.
To reduce this, steroids should be used at the lowest effective dose and for the shortest period possible; combination therapy with immunosuppressive drugs may help to achieve this.
DERMATOMYOSITIS
connective tissue disorders defined by the presence of muscle weakness and inflammation with dermatological manifistations.
The aetiology is unknown and genetic associations differ amongst ethnic groups.
2 peaks of incidance juvenile and adulthood type (between 40 and 60 years of age).
There is an increased risk of malignancy (about a threefold increase).
Malignancy may be apparent at the time of diagnosis or later.
The typical presentation
symmetrical proximal muscle weakness, usually affecting the lower extremities first. sometimes with muscle pain.The onset is usually gradual.
Other systemic manifestations include arthralgia, weight loss and fever.
Characteristic cutaneous manifestations
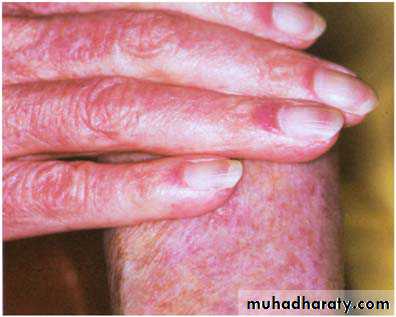
The heliotrope rash is oedema with a violaceous discoloration of the eyelid .Gottron's papules are erythematous scaly papules or plaques occurring over the knuckles.
Periungual nail-fold capillaries are often abnormal.
Investigations
Creatine kinase (CK) is usually raised and is a guide to disease activity.Electromyography (EMG) mayconfirm the presence of myopathy and exclude neuropathy.
muscle biopsy: fibre necrosis, regeneration and inflammatory cell infiltrate.
MRI identifying areas of abnormal muscle that are amenable to biopsy.
When underlying malignancy is suspected screening investigations should include chest/abdomen/pelvis CT, gastrointestinal tract imaging and mammography.
Management:
Rest.
Topical: potent steroid to the skin lesions.
Oral corticosteroids (e.g. prednisolone 40-60 mg daily) are the mainstay of initial treatment. Patients with severe weakness or evidence of respiratory or pharyngeal weakness may need methylprednisolone 1 g daily for 3 days. If there is a good response, the prednisolone dose should be reduced by approximately 25% per month to a maintenance dose of 5-7.5 mg.
immunosuppressive therapy, Azathioprine and methotrexate are the initial agents of choice. ciclosporin, cyclophosphamide, tacrolimus and intravenous immunoglobulin are alternatives.
Scleroderma
Localized Scleroderma (Morphea).Scleroderma derived from the Greek terms skleros, hard, and derma, skin and means hard skin.
Localized scleroderma (LS) or morphea encompasses a group of disorders characterized inflammatory sclerosis (thickening) and fibrosis of the skin± subcutaneous tissue, fascia and/or adjacent muscle
The cause of morphea
is unknown.Genetic
Environmental factors:
trauma ,Radiation,infectious ,vaccination .
ischemic injury
Such triggers may have a role in in the activate the of immune system and initiate fibrosis.
Morphea is commoner in women, 6 and 2.6:1.
Biopsy specimen
normal epidermis.sclerosis of the dermis.
periadnexal inflammation .
sweat glands are entrapped by higher in the dermis.
Clinical presentation
Localised morphea may be divided into 5 subtypes:Plaque.
Guttate.
Linear.
En Coup de Sabre
. Deep.
Diagnosis and Measurement of Disease Activity
The diagnosis is based on:clinical findings
histology Characteristic.
clinical features suggestive of active disease
include extension of lesions,
appearance of new lesions
presence of a violaceous halo.
Therapy
Topical Corticosteroids: (high potency ) “first-line” treatment for patient with plaque morphea.
Ultraviolet A.
(PUVA).
UVA1 with topical calcipotriol ointment.
Antimalarials.
Methotrexate.
Interferon-_ .