Lumbar Spinal Canal Stenosis & Lumbar Disc Disease
Dr. Moneer K. FarajConsultant Neurosurgeon
College of Medicine, Baghdad Uni.
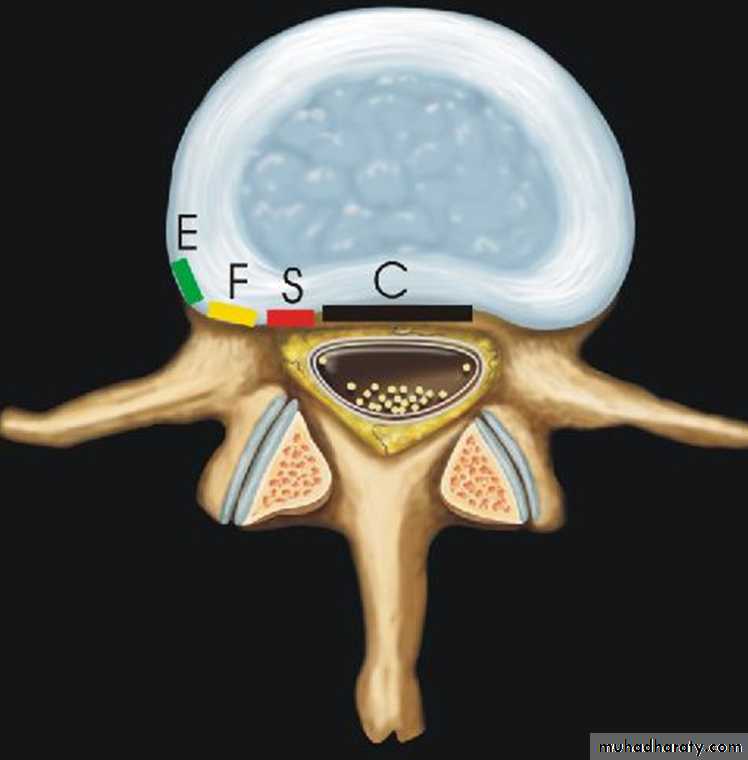
Lumbar spinal canal stenosis :Reduction in the diameter of the spinal canal which results from either congenital stenosis & / or degenerative changes.
Definition
Degenerative changes may result in:
Lumbar disc protrusionFacet joint osteoarthritis
Ligamentum flavum hypertrophy
End plate changes ( modic changes)
Pathogenesis
Neurogenic Claudication
Dermatomal: pain/sensory changes/weakness of buttock, hip, thigh, or leg initiated by standing or walkingslow relief with postural changes (sitting >30 min), NOT simply exertion cessation
elicited with lumbar extension, but may not have any other neurological findings, no signs of vascular compromise (e.g. ulcers, poor capillary refill, etc.)
Clinical Features: History
Facet Joint Syndrome
comprises clinical symptoms related to the facet joints such as dysfunction and osteoarthritis.The cardinal symptoms of facet joint pain are:
predominant low-back pain
osteoarthritis pain type (improvement during motion) However, in late stages of OA this alleviation will disappear
pain aggravation in extension and rotation (standing, walking downhill)
The pain is often located in the buttocks and groin and infrequently radiates into the posterior thigh. However, it is non-radicular in origin.
Patients often feel stiff in the morning sometimes of such intensity that they have difficulty to get out of bed.
Instability Syndrome
The cardinal symptom of a segmental instability is:mechanical low-back pain
Instability pain worsens during motion and improves during rest
Vibration (e.g. driving a car, riding in a train) may aggravate the pain.
Pain is also felt when sudden movements are made. The resulting muscle spasm can be so severe that the patients experience a lumbar catch (“blockade”). Pain usually does not radiate below the buttocks.
Some patients benefit from wearing a brace.
In patients with facet syndrome, physical findings are:
pain provocation on repetitive backward bendingpain provocation on repetitive side rotation
hyperextension in the prone position
In patients with instability syndrome, physical findings are:
abnormal spinal rhythm (when straightening from a forward bent position). The patient needs the support with hands on thighs when straightening out of the forward bent position by supporting the back.
Clinical Features: Signs
Standard radiographs are rarely diagnostic
disc space narrowing with endplate sclerosis
severe facet joint osteoarthritis
Flexion/Extension Films
Functional views : excessive segmental motion (>4mm) or subluxation of the facet joint that is rare in asymptomatic individuals
Diagnostic workup
Computed Tomography
The current role of CT is for patients with contraindications for MRI (e.g. pacemaker). In the latter case, CT is often combined with myelography (myelo-CT) to provide conclusions on potential neural compression.in the evaluation of patients postoperatively to assess lumbar fusion status.
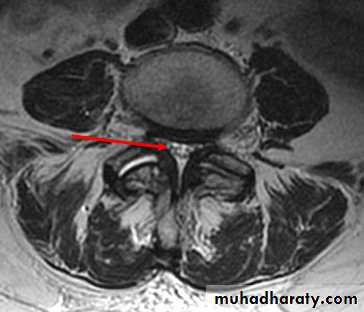
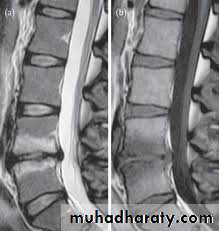
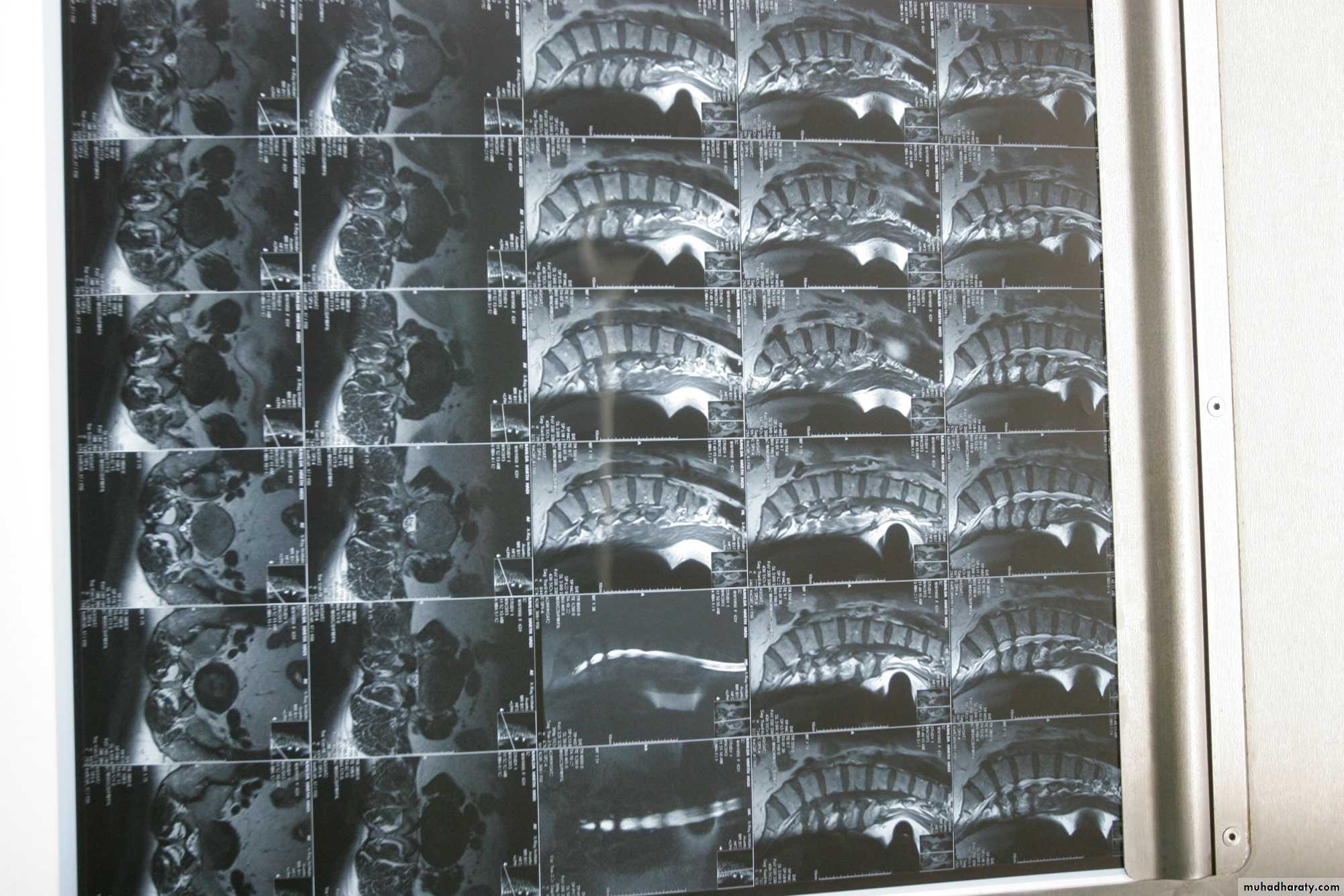
MRI
It is superior to computed tomography (CT) because of its tissue contrast and multi planar capabilities.General objectives of treatment
pain reliefimprovement of health-related quality of life
improvement of work capacity
Treatment
Patient Selection for Treatment
Various domains must be considered,medical factors
psychological factors
sociological factors
work-related factors
Favorable indications for non-operative treatment
minor to moderate structural alterations
short duration of persistent symptoms <6months
Pain of variable intensity and location
absence of risk factor ( early neurological deficit)
intermittent symptoms
The non-operative management composed of
:pain management (medication)
functional restoration (physical exercises)
cognitive-behavioral therapy (psychological intervention)
Favorable indications for operative treatment
severe structural alterations and instabilityfailure to relief the pain more than 6 months of medical therapy.
Progressive neurological deficit
Psychologically stable patient.
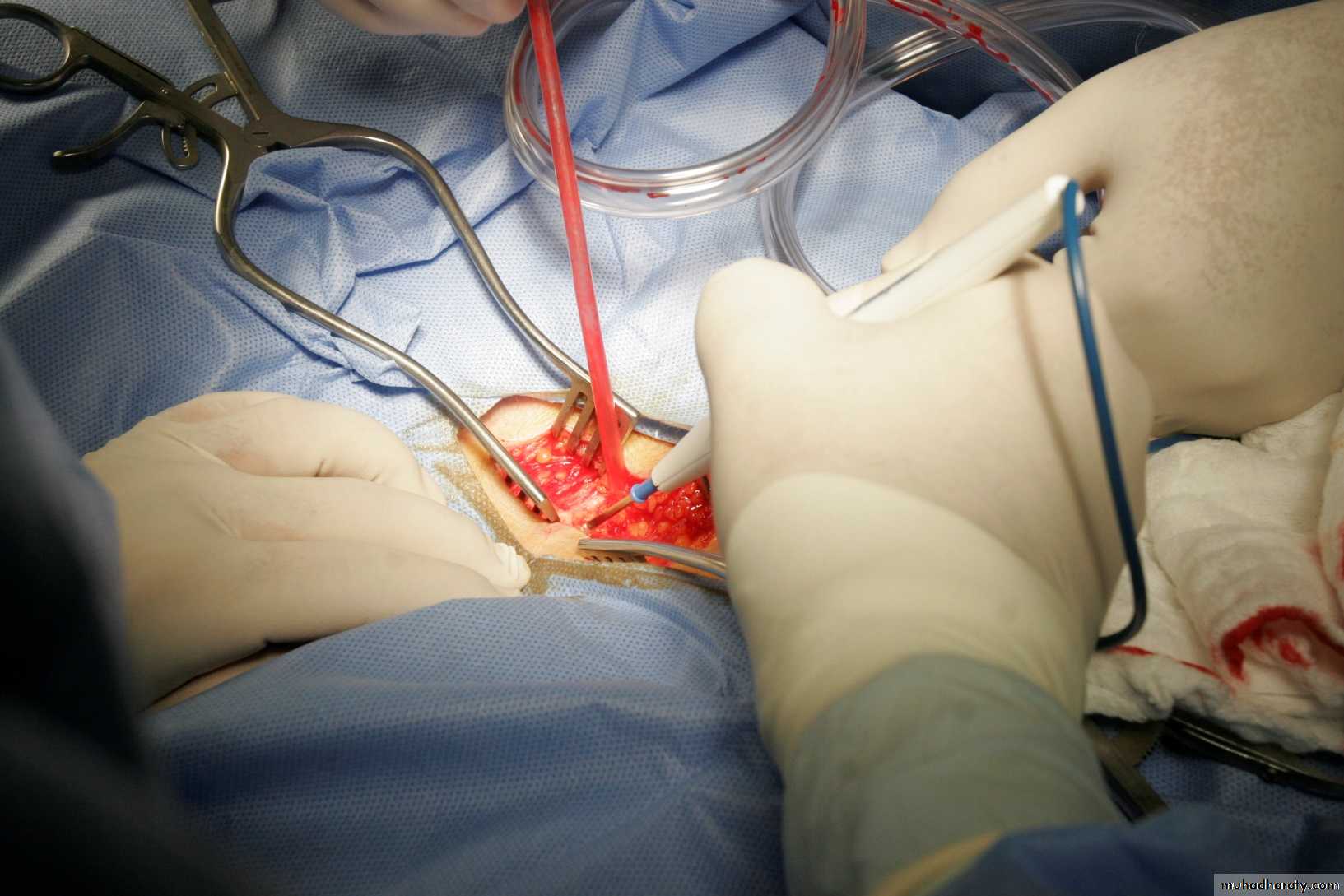
Operative Management
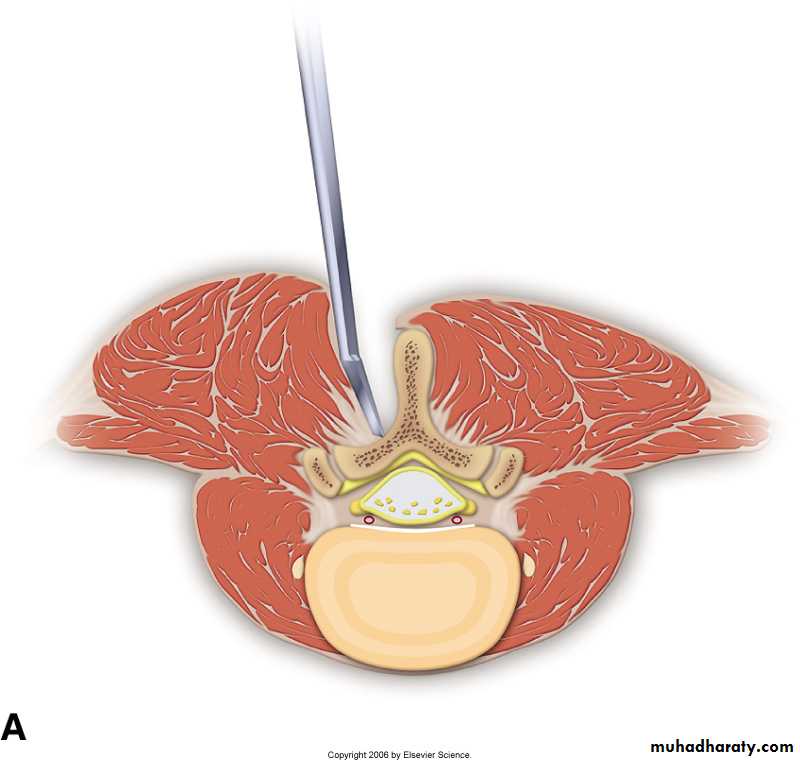
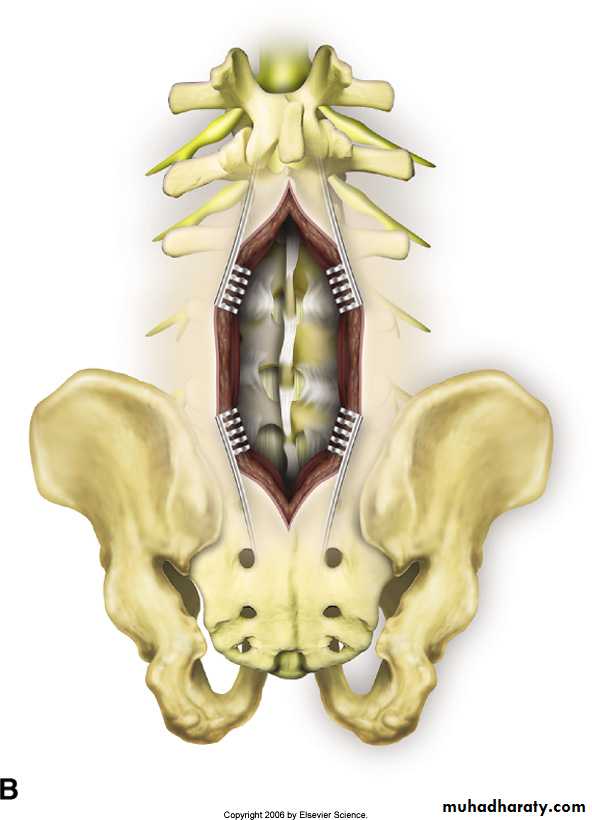
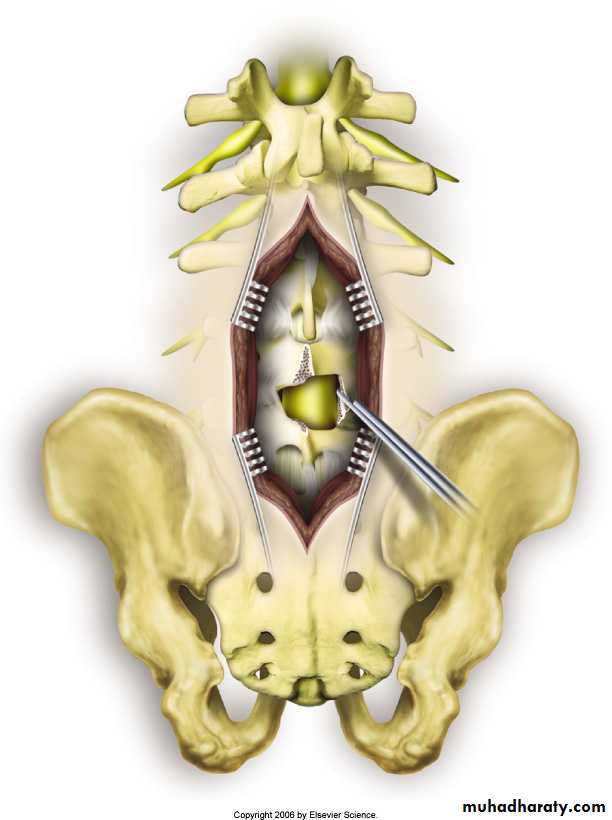
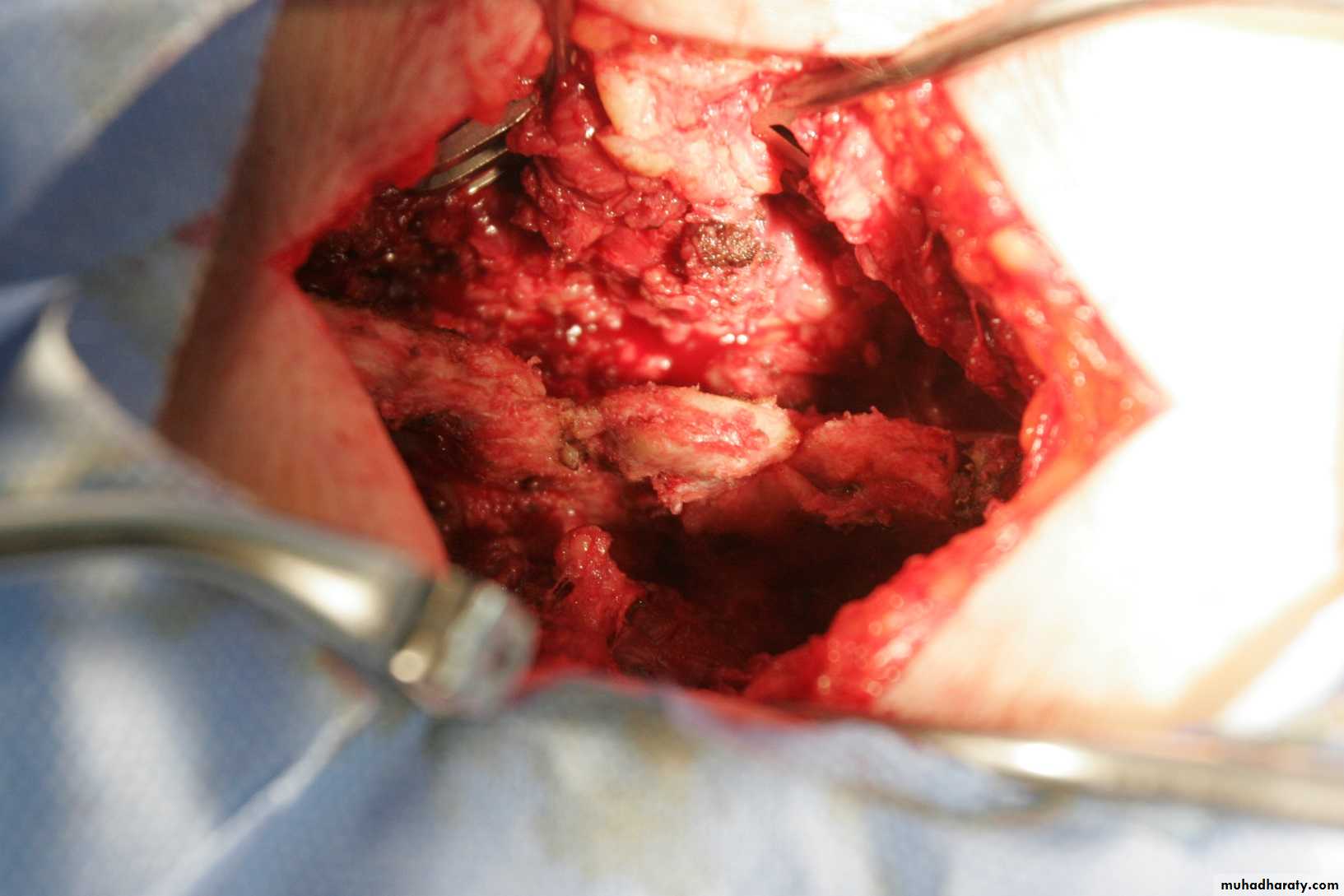
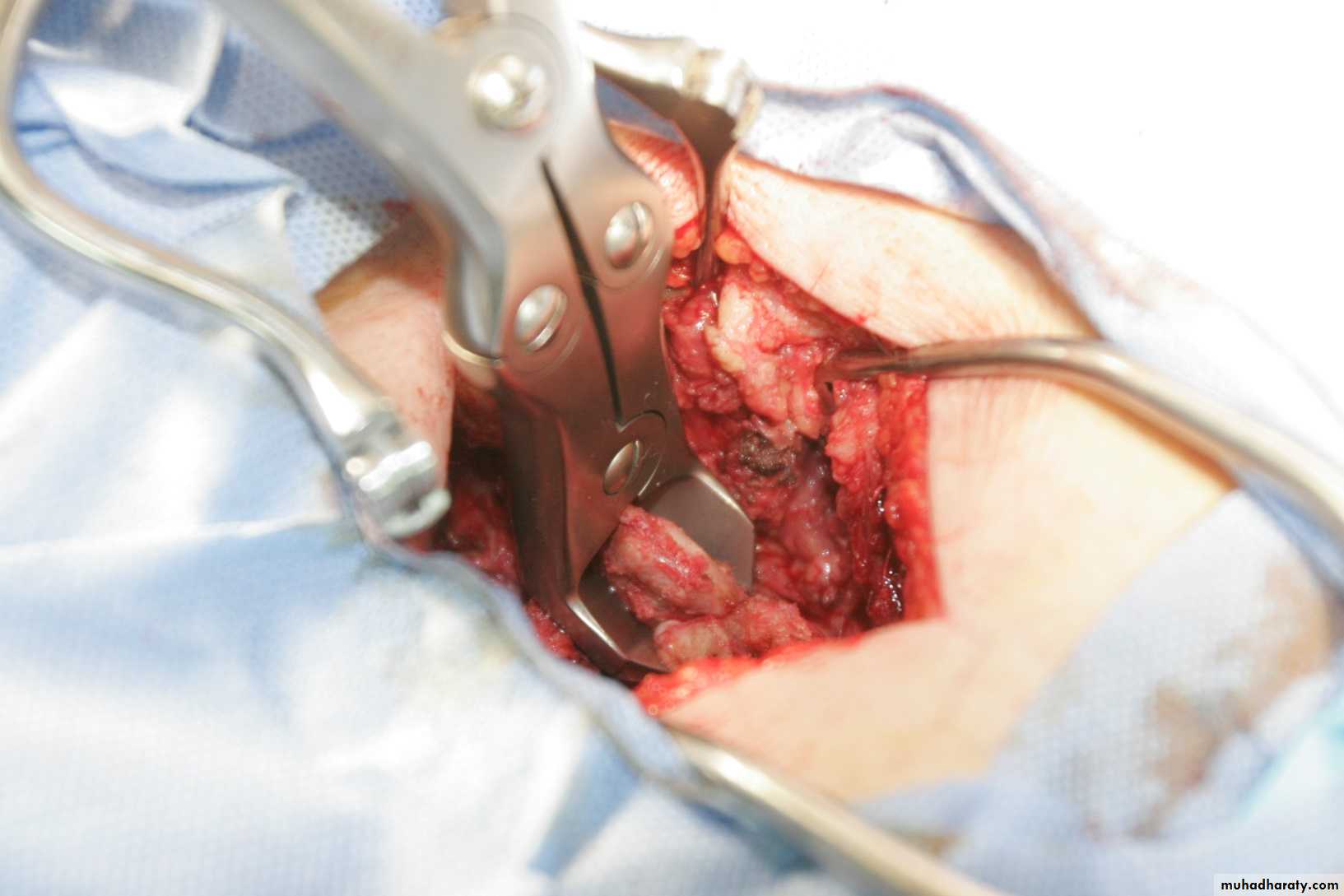
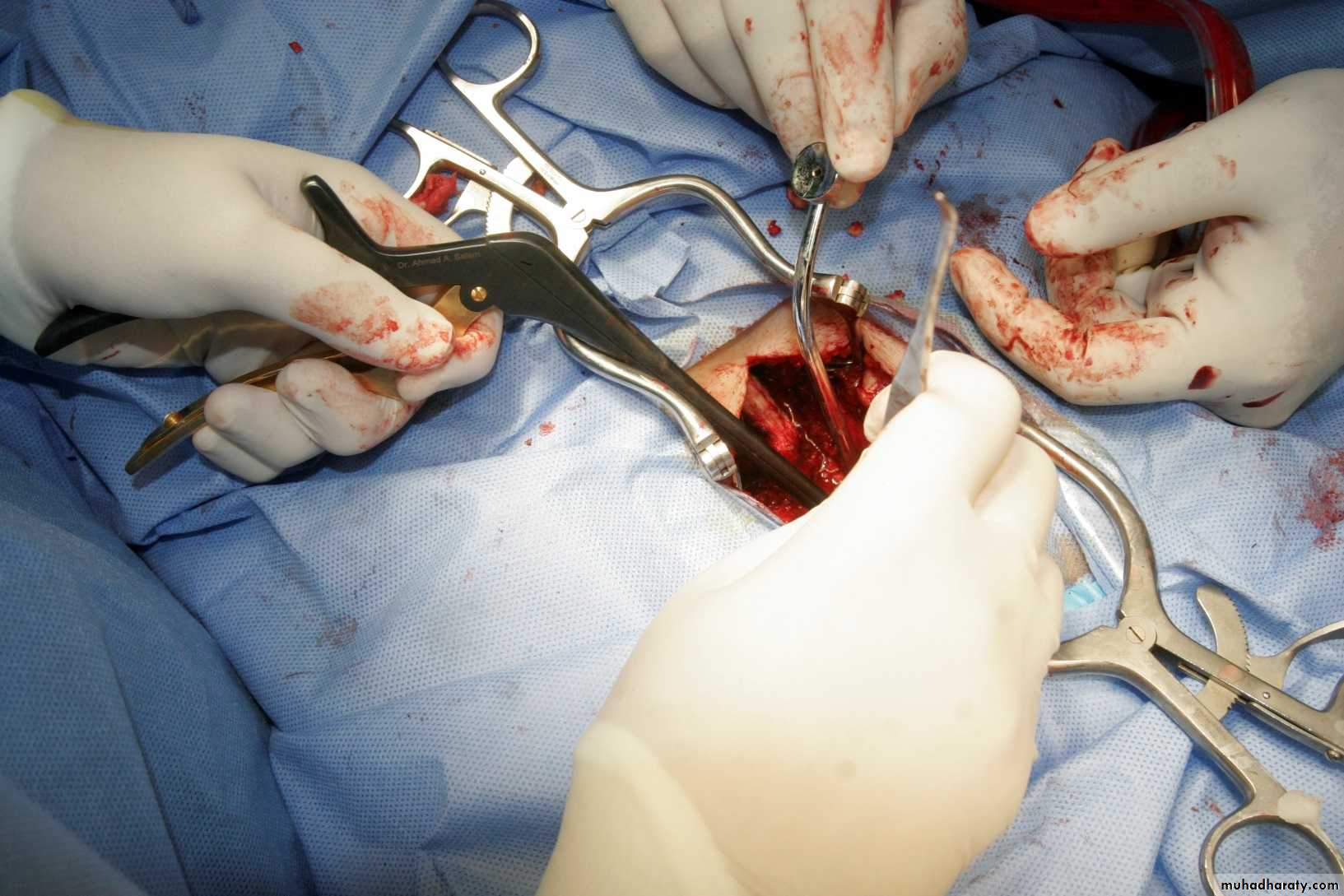
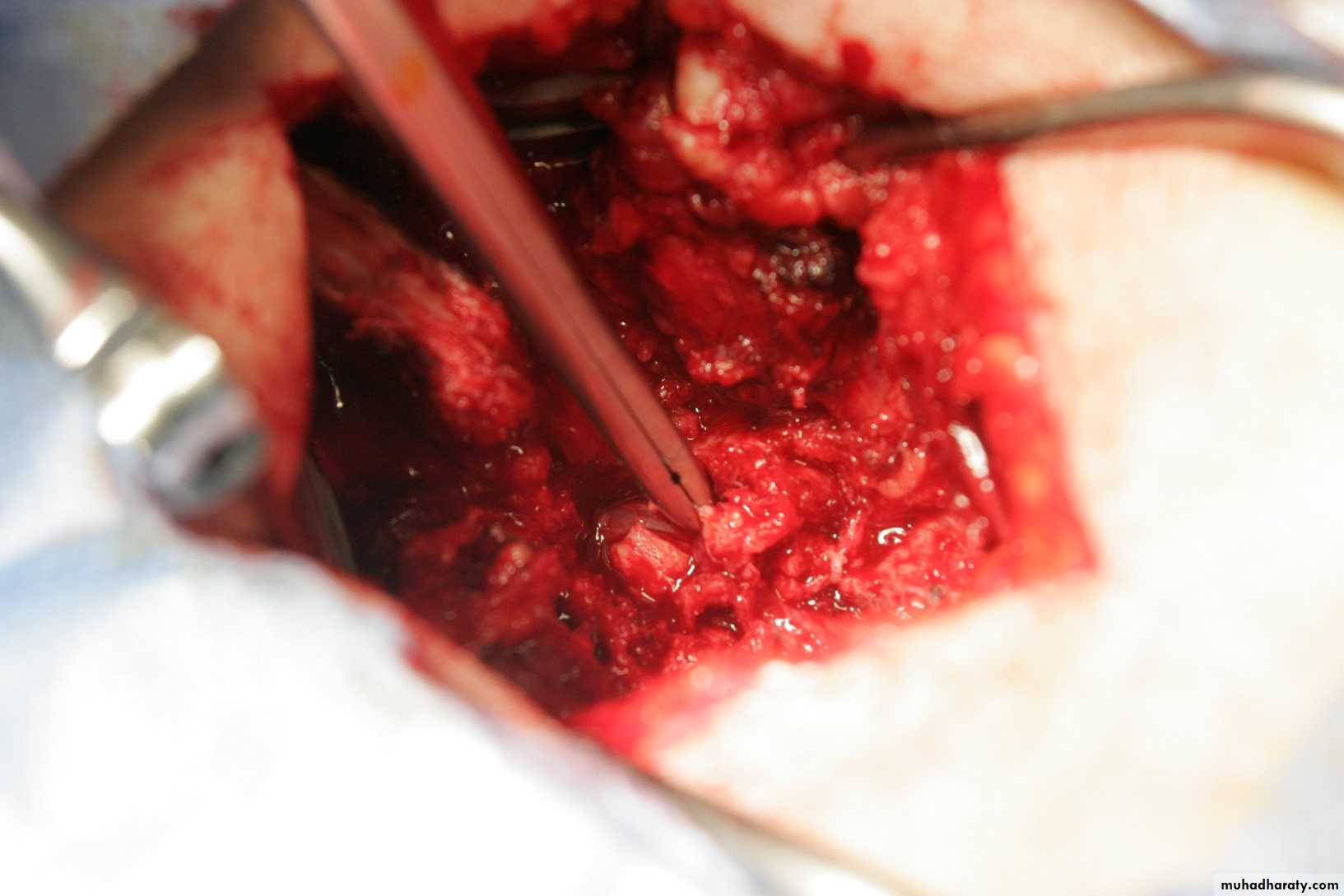
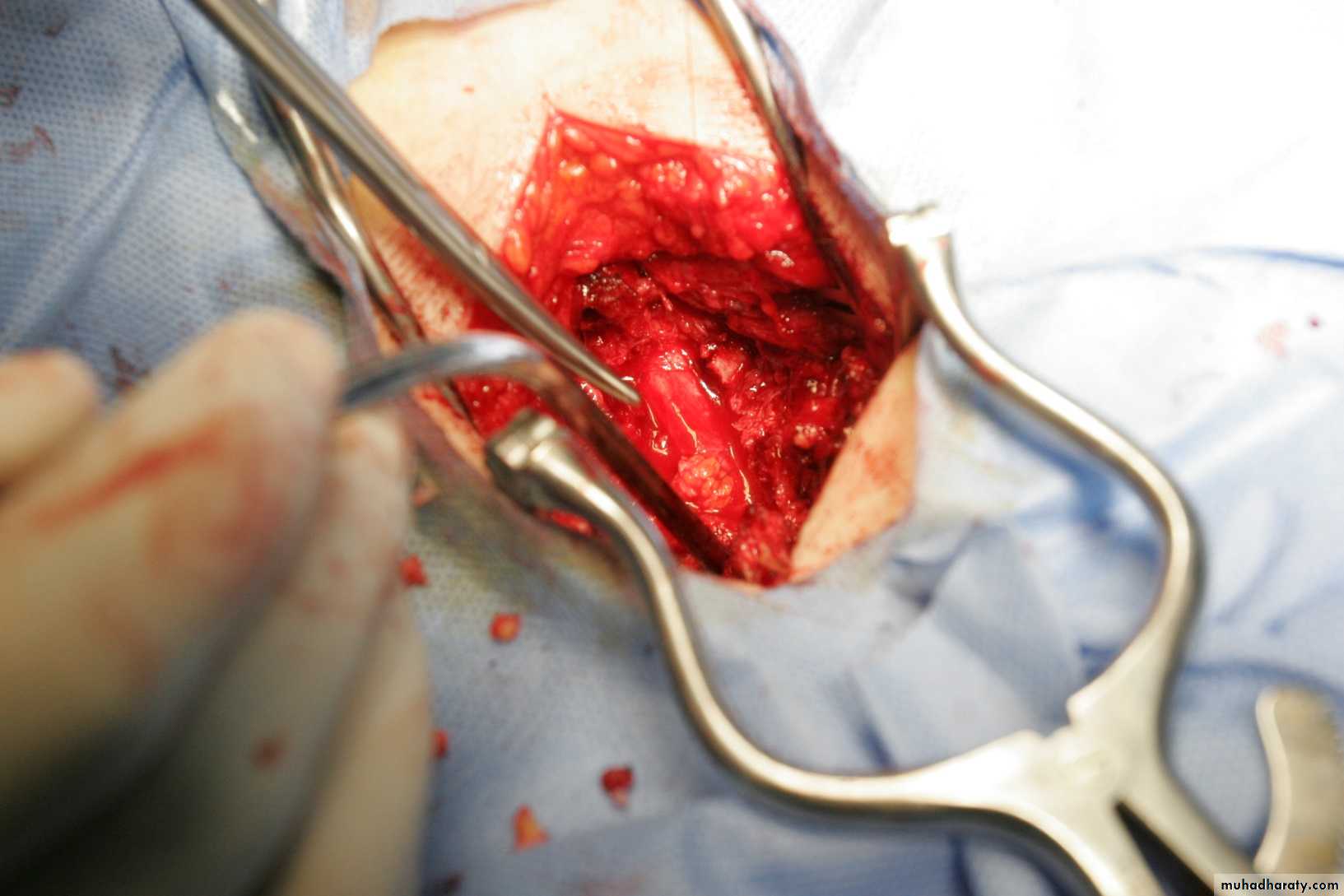
Decompression Laminectomy
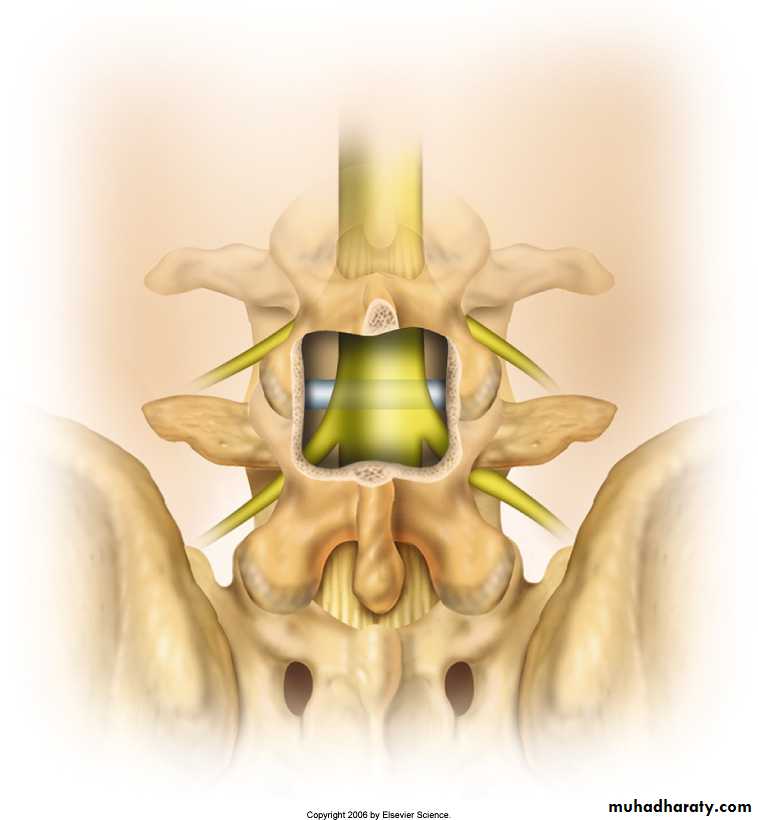
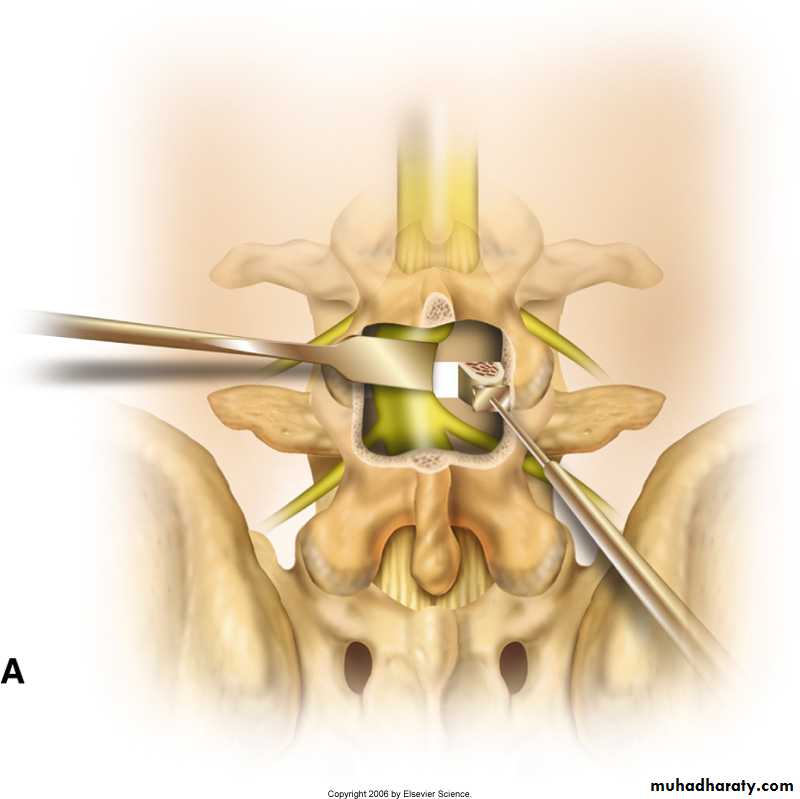
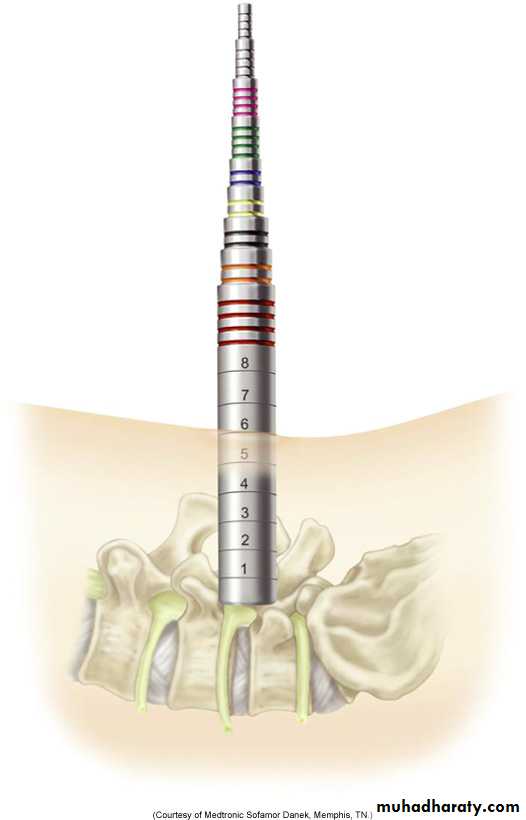
Non instrumented spinal fusionInstrumented spinal fusion
Spinal fusion with fixation
A combination of previous surgeries
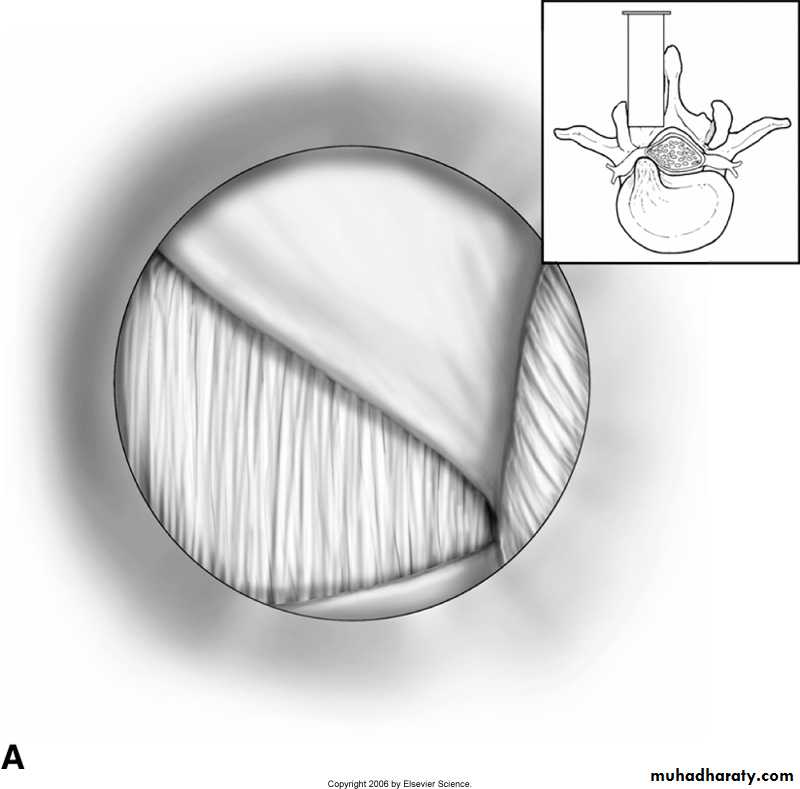
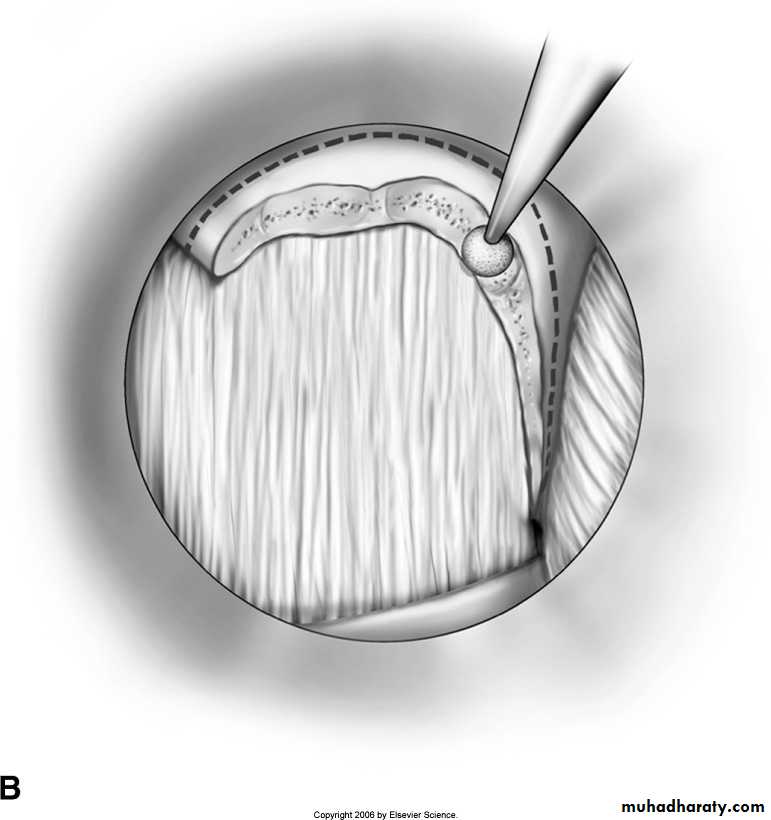
Surgical Procedures
Etiology
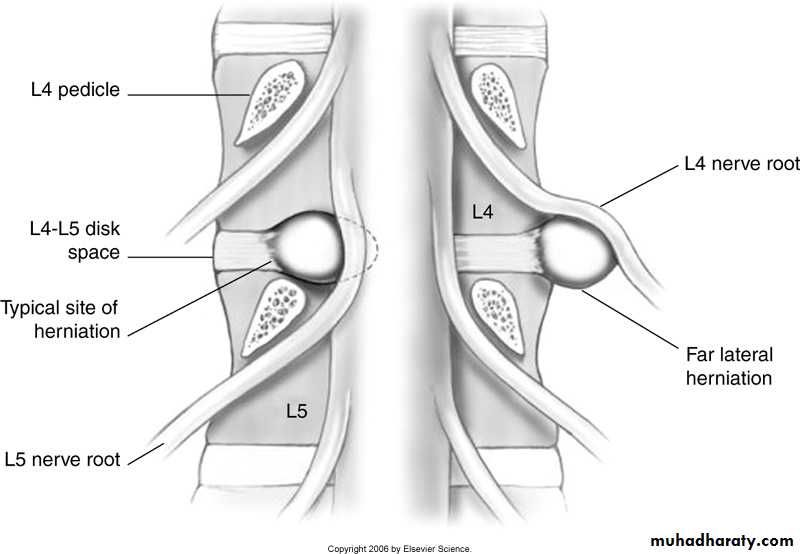
Tear in the annulus with herniation of the nucleus outside either laterally compressing nerve root, or centrally causing cauda equina or lumbar stenosis (neurogenic claudication)Lumbar Disc Syndrome
leg pain > back pain
limited back movement (especially forward flexion) due to pain
dermatomal sensory changes, motor weakness, reflex changes
exacerbation with coughing, sneezing or straining. Patients often report that sitting is the worst position (caused by disc compression).
Relief with flexing the knee or thigh
nerve root tension signs
straight leg raise (SLR test) or crossed SLR (pain should occur at less than 60 degrees) suggest LS, Sl root involvement
femoral stretch suggest L2, L3 or L4 root involvement
Clinical Features
Central , sub articular, foramenal, extreme lateral
• L5-S1
• L4-5• L3-4
• Sl
• L5
• L4
• Root Involved
• 45%
• 45%
• <10%
• Incidence
• Sciatic pattern
• Sciatic pattern
• Femoral pattern
• Pain
• Lateralfoot
• Lateral leg
• Dorsal foot to hallux
• Medial leg
• Sensory
Gastronemius, Soleus ( plantar flexion)
• Extensor hallusis
• longus ( hallux
• extension)
• Tibialis anterior
• (dorsiflexion)
Motor
• Ankle jerk
• Knee jerk
• Reflexes
x -ray spine (only to rule out other lesions)
CT, CT- Myelography
MRl
consider EMG, nerve conduction studies if diagnosis uncertain
Investigationsconservative
bed restactivity modification, patient education (reduce sitting, lifting)
physiotherapy, exercise programs
analgesics may help
Treatment
surgical indications
intractable pain despite adequate conservative treatment for >3 months
progressive neurological deficit
Types:
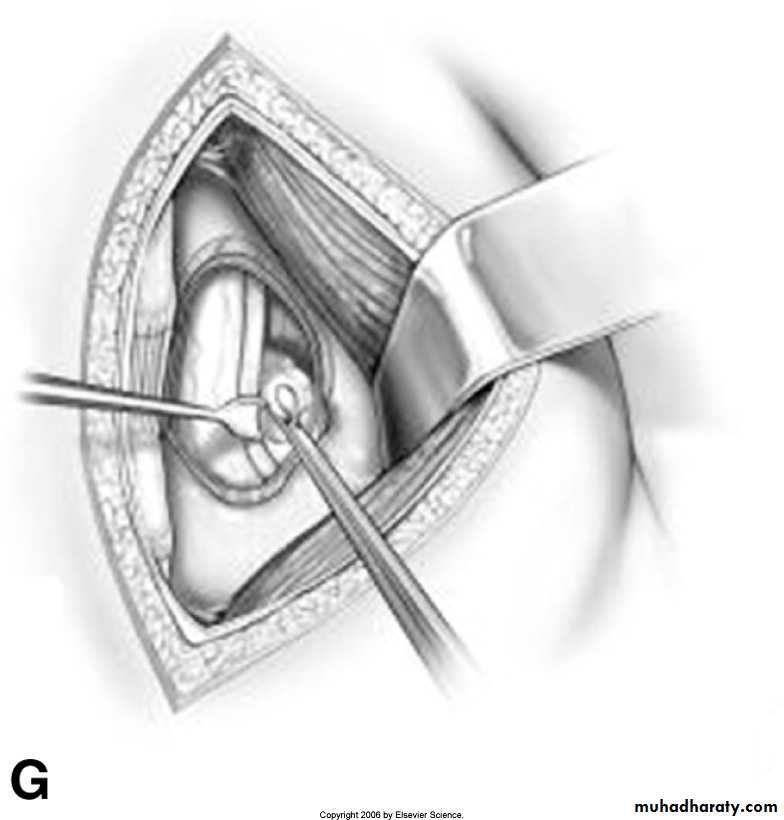
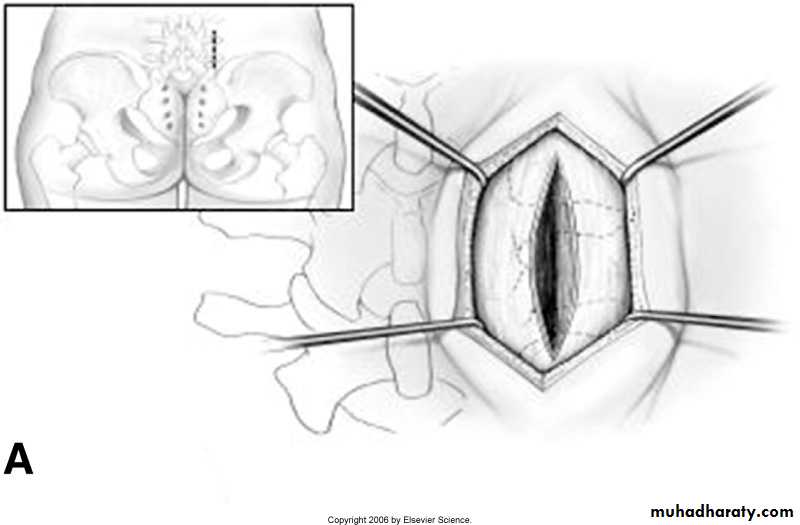
- open laminectomy with discectomy
- micro discectomy
Surgery
Etiology
compression or irritation of lumbosacral nerve roots below conus medullaris due to decreased space in the vertebral canal below L2.Common causes include herniated disk, spinal stenosis, vertebral fracture and tumors.
Cauda Equina Syndrome
usually acute (develops in less than 24 hours); rarely subacute or chronicmotor (LMN signs)
weakness/paraparesis in multiple root distribution
reduced deep tendon reflexes (knee or ankle)
autonomic
urinary retention (or over flow incontinence) and/or fecal incontinence due to loss of anal sphincter tone
sensory
low back pain radiating to legs (sciatica) aggravated by Valsalva maneuver and by sitting; relieved by lying down
bilateral sensory loss or pain: depends on the level of cauda equina affected
saddle area (S2-S3) anesthesia (most common sensory deficit)
sexual dysfunction (late finding)
Clinical Features
Treatment:
requires urgent investigation and decompression (<48 hrs) to preserve bowel and bladder function and/ or to prevent progression to paraplegiaPrognosis:
markedly improves with surgical decompression.
Recovery correlates with function at the initial consult: if patient is ambulatory, likely to continue to be ambulatory; if unable to walk, unlikely to walk after surgery