1
Fifth stage
Plastic Surgery
Lec-1
.د
اسامة
13/12/2015
Principles of plastic surgery
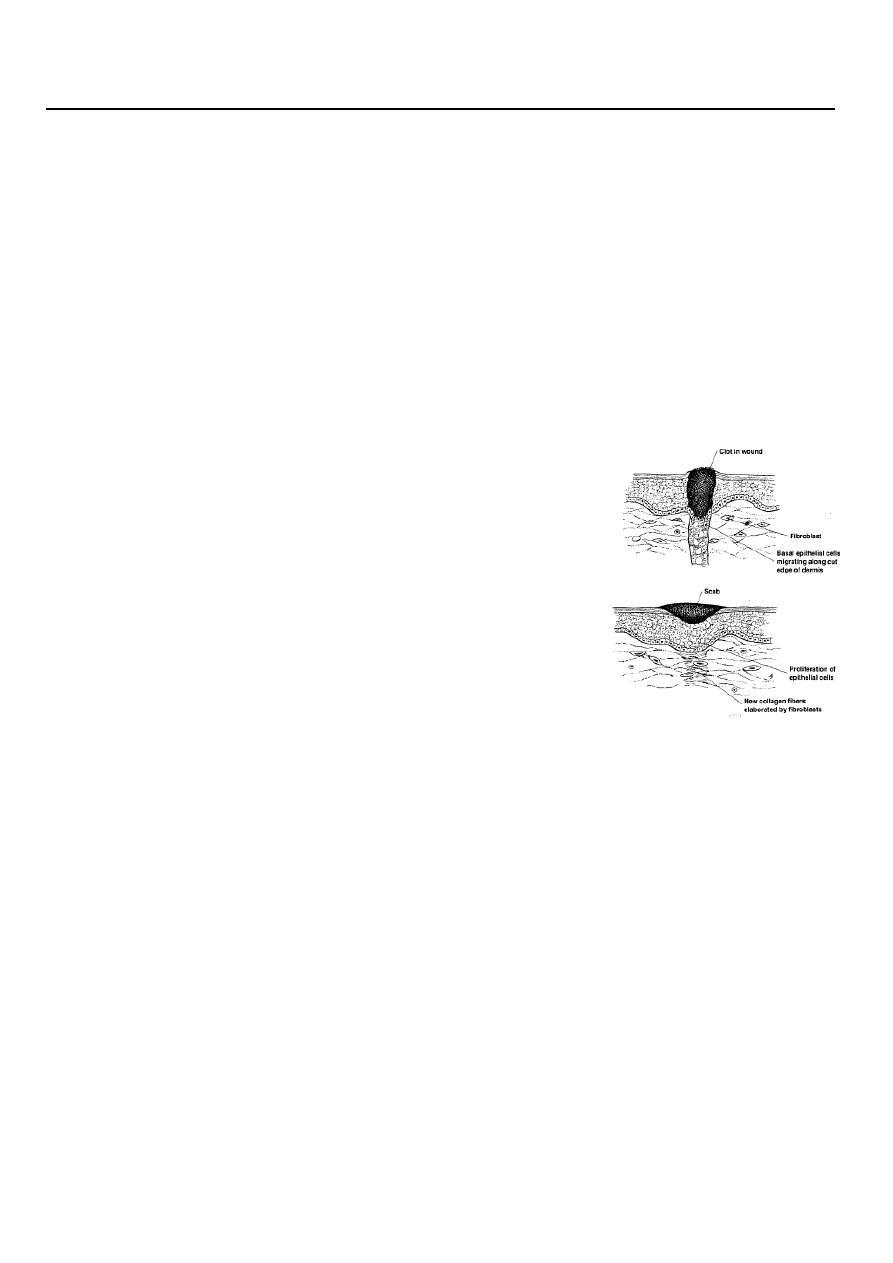
Wound Healing:
Body attempt to restore tissue to its structural and functional pre injury state.
Wound healing either by regeneration or repair
All tissues repair except?
Liver and bone
Wound Healing Normally Proceeds in an Organized Process:
Four Phases of Wound Healing
1-Hemostasis
2-Inflammation
3-Proliferation
4-Remodeling (maturation)
Classification of wound closure and healing:
1. By primary intention
2. By secondary intention
3. By tertiary intention
Features of good scar
1- Fine line scar
2- Absence of contour irregularities
3- No pigmentary irregularities
4- No contracture or distortion
Obtaining A Fine-Line Scar(good scar)
The final appearance of a scar is dependent on many factors:
2
(1) the age of the patient, type of skin and location on the body.
(2) the tension on the closure.
(3) the direction of the wound.
(4) co-morbid conditions.
(5) the technique used for skin closure.
Age:
Who will have better scar a child or elderly patient?
Loss of elasticity combined with changes in the subcutaneous tissue, produce
wrinkling, which makes scars in older individuals less obvious and less prone to
stretching.
o Child: raised red scar.
o Old age : flat white scar.
Type of skin:
Type of skin should also be taken into account. Skin that is oily or pigmented, or both,
produces more unsightly scars..
Certain anatomic areas produce unfavorable scars that tend to become hypertrophic
or widened. The shoulder and sternal area are notable examples. On the other hand,
eyelid scars almost always heal with a fine-line scar
Nutritional status can affect wound healing:
1. Wounds gain strength less rapidly in the face of protein depletion.
2. Vitamin A reverses the healing retardation caused by steroids.
3. Vitamin C deficiency has long been known to cause scurvy, characterized by a failure
of collagen synthesis.
4. Zinc is required for epitheliazation and fibroblast proliferation.
5. Ferrous iron and copper are necessary for normal collagen metabolism.
Co-morbid conditions such as anemia,ureamia and Diapedus can retard wound
healing. .
3
Atraumatic technique by:
Minimizing damage to the skin edges with atraumatic technique
Debridement of necrotic or foreign material
Good irrigation of traumatic or contaminated wounds.
o Careful handling of tissue.
o No crushing or dryness.
o No strangulation or tension.
o Hemostasis.
o Sharp knife.
o No hot sponges.
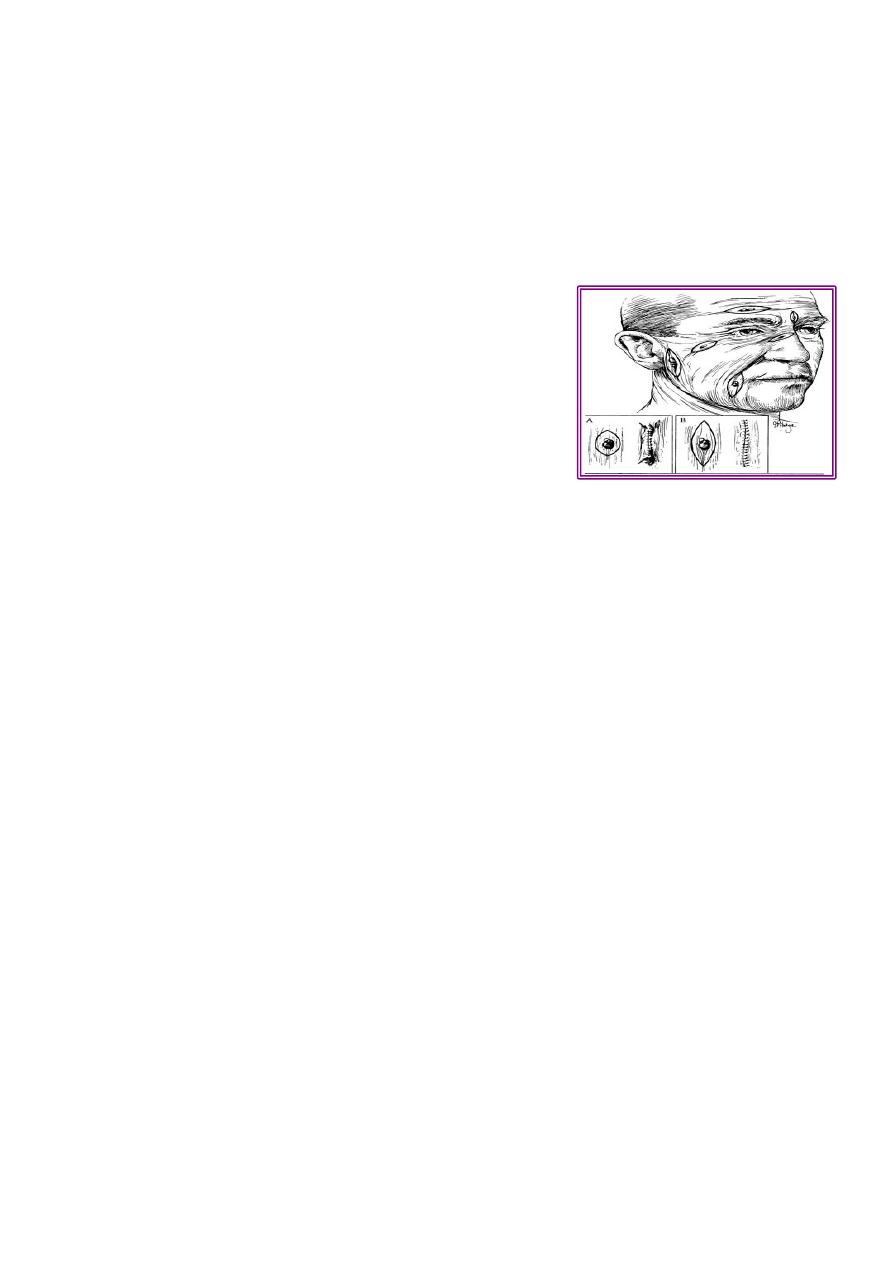
Skin lines:
The lines of tension in the skin were first noted byLanger(1861) who described the normal
tension lines of the skin, called “Langer’s lines”. Or called “relaxed skin tension lines”
Excision of lesions is planned when possible so that the final scar will be parallel to the
relaxed skin tension lines. Maximal contraction occurs when a scar crosses the lines of
minimal tension at a right angle. Wrinkle lines are generally the same as the relaxed skin
tension lines.
Method of homeostasis:
Electro-cautery.
Ligature.
Pressure and time.
Clamping and twisting.
Vasoconstrictor.
Fibrin foam.
Methods of suturing:
A. interrupted.
B. Vertical mattress.
C. Transvers mattress.
D. Subcuticular .
E. Continous.

4
Factors determine the severity of suture markers:
1.Time of removal of stitches .
2.Diameter of the suture .
3. Relation to wound edges.
4. Region of the body.
5.Absence of infection.
6. Propensity for keloid.
When to remove the Stitches from different body sites?
Sutures:
Are the most common materials used to close a wound.
They are 2 types:
1. Absorbable:
a. Natural :
o Catgut (plain , chromic) from submucosa of sheep intestine.
o Collagen suture from flexors of beeves.
b. Synthetic:
o Polyglycolic A.(Dexon ).
o Polyglactin 910 (Vicryl ).
o PDS (polydiaoxonon suture).
2. Non-absorbable:
1. Natural : silk, cotton. stainless steel.
2. Synthetic:
1. Polyamide (nylon): degrade 20 % / year.
2. Polyester (Dacron, Ethibond)
3. Polypropylene ( Prolene).
5
Skin graft:
Definition: is a segment of epidermis and dermis that is removed without its blood
supply from donor site transferred into a recipient site
Types: according to:
o Origin:
Autograft , allo-(homo), xeno(hetero)-, iso-graft (identical twins)
o Thickness:
Split-thickness graft(Thiersch graft): thin ,intermediate, thick.
Full thickness graft (Wolfe graft).
Flaps:
“ part of tissue which retains its vascular attachment to body, transplanted to
reconstruct a defect.”
The flap donor site closed by suture or SSG.
Skin tumors
Basal cell carcinoma (BCC):
Most common, 75% of skin tumors.
Arise from basal layer of epidermis.
Affects white skin, Male: Female=3:2 .
Occurs on exposed parts: face, neck, scalp.
No metastasis.
Commonly Caucasian male older than 60 years
Diagnosis: by biopsy (FNA, incisional biopsy , excisional biopsy)
Treatment:
Surgery: excision with 2-5 mm. healthy margin, & repair defect by skin graft or flap.
Radiotherapy: in large lesion, oldman, refusing operation.
Cryotherapy: for primary lesion < 2 cm., but hypopigmentation, scarring are
disadvantages.
Squamous Cell Carcinoma:
(SCC) is second most common skin cancer.
arises from the malignant transformation of keratinocytes in the epidermis.

6
arise either in normal skin or in preexisting lesion as (actinic keratosis, leukoplakia,
radiation keratosis, scars( where called Marjolin ulcer).
Clinically: present as irregular ulcer, everted edge, indurated base,attached deeply,
blood-stained discharge,frequent lymph n. positive.
Treatment: biopsy done.
1- Excision
Surgical excision with 10-mm margin
If lymph n. positive: excise lesion with lymph n. dissection.
2-Radiation therapy is best used in older patients,
Cleft lip and palate
One of the most frequently encountered congenital facial defects
Embryology: result of breakdown in the normal lines of fusion during the early stage
of fetal development
Etiology of the clefts
The cause of the cleft lip and palate is multifactorial involving both genetic and
environmental factors
15% of the cleft cases are syndromatic with more than 170 syndrome have it as a
feature
Smoking is now well known to increase the incidence of clefting
Multivitamine and folic acid in the 1st four months of pregnancy is protective
Common questions asked by the family:
1-How to feed the baby
2-Timing of surgery
3-How many operation needed
Feedings:
It is important to keep the cleft clean
Breastfeeding is extremely challenging.
Repair :lip at 3 months or rule of 10 (10 pounds weight, 10 gm Hb, 10 weeks old).
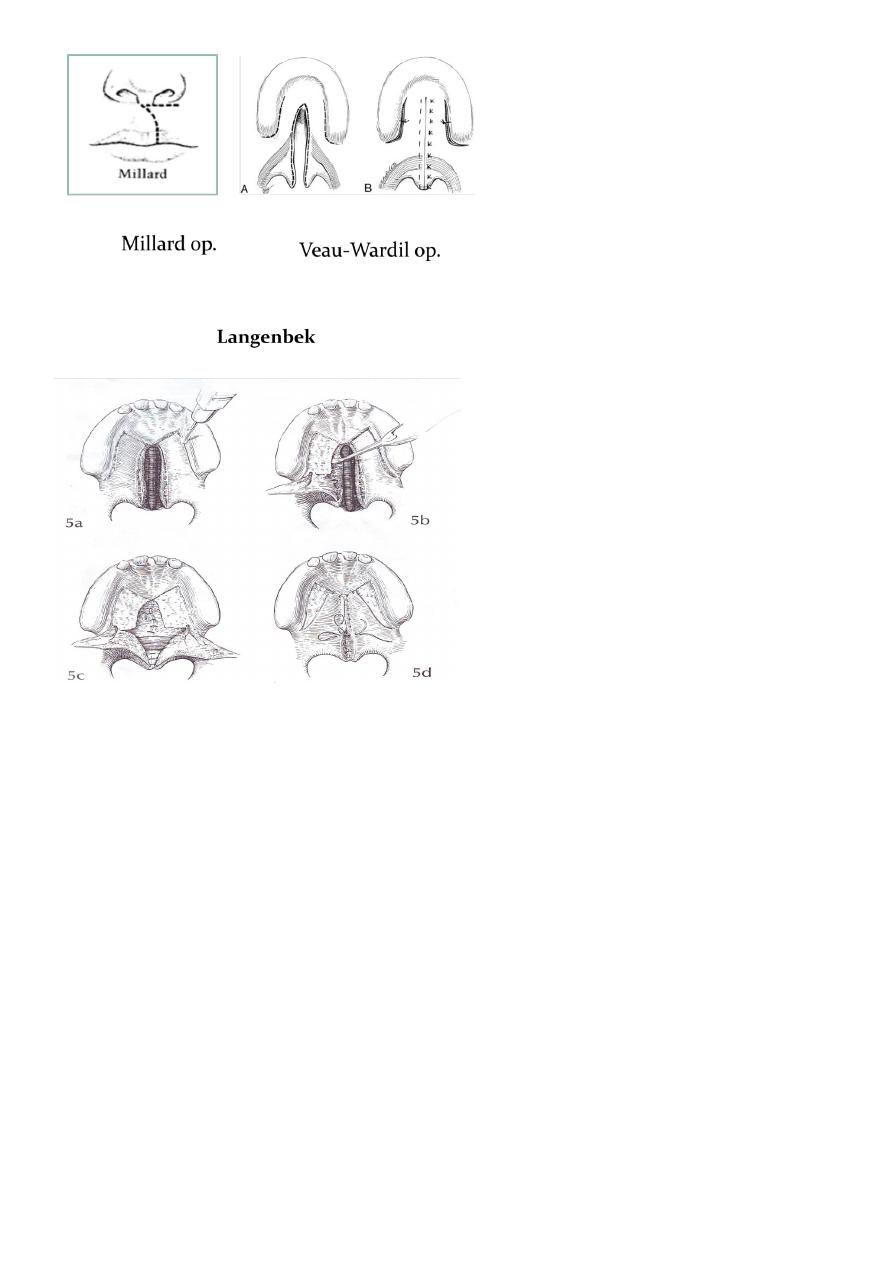
o Palate : at 12-18 months, by Veau-Wardil, 4 flaps, Langenbek.
Aim of repair:
o lip: to improve appearance
o Palate: to achieve normal speech and prevent regurgitation .
7
Effects on child:
o Inability to suck.
o Speech –nasal.
o Dentition deformity
o Nose deformity.
o Hearing defects.
