1
Fifth stage
ENT
ع
ملي
-
كتابة الطالب
د.سعد
7/12/2015
ENT = Ear Nose Throat
ORL = otorhinolaryngology
1- The Ear:
Symptoms of the ear:
Pain:
o Primary or secondary.
o Otogenic (caused be otitis media for example).
o Non-otogenic (cause be problems in the tooth, glossopharyngeal nerve, C2 and C3,
maxillary division of trigeminal nerve, temporomandibular joint, cervical spine).
Discharge:
o Mucus: due to perforated tympanic membrane.
o Serious: due to otitis externa or perforated tympanic membrane.
Hearing loss.
Tinnitus.
Vertigo.
Note: anything cause hearing loss could lead to tinnitus.
Examination of the ear:
Introduce yourself to the patient:
o Check hearing function, Any deafness?
o Communication
Position the patient:
o At the same level
o In chair
o Can walk around patient
Inspect the pinna
o Front and behind
o Skin condition
o Lesions
o Scars
o Pre-auricular area (common place for sinus)
o Condition of cartilage
2
Findings in inspection of the pinna
Photos
Post auricular scar
Indications:
1-Tympanoplasty
2-mastoid surgery (mastoidectomy)
3-resection of benign parotid gland tumor
Benefit: cosmetic.
Discharging ear
Causes:
1-wax
2-otitis media
3-otits externa
4-mastoiditis
5-F.B. in the ear
Preauricular sinus
Cause: congenital.
Treatment: no treatment unless infected
antibiotics or surgery.
Could convert to fistula (discharge) or
abscess (closed).
Auricular hematoma
Causes:
1-trauma
2-bleeding tendency
3-infection.
4-allergic skin diseases
Treatment: complete surgical evacuation of
the subperichondrial blood and prevent its
recurrence.
It need drainage if not deformity of
the ear.
Main complication: cauliflower ear.
Cauliflower ear
Due to repeated trauma and hematoma
Common in boxers.
Treatment: cosmetic surgery.
3
Auricular ulcer
Occur in squamous cell carcinoma
Acute mastoiditis
Causes: untreated acute otitis
media(commonest) + trauma
Medical treatment: long term antibiotics.
Surgical treatment:
1-tympanostomy tube.
2-mastoidectomy.
Complications:
1-subperiosteal abscess 2-skin fistula
3-hearing loss
4-facial palsy
5-meningitis 6-brain abscess
Right acute mastoiditis
The right pinna pushed forward and
downward.
Postauricular Hearing aid
or
behind the ear (BTE)
BAHA: Bone Anchored Hearing Aid
4
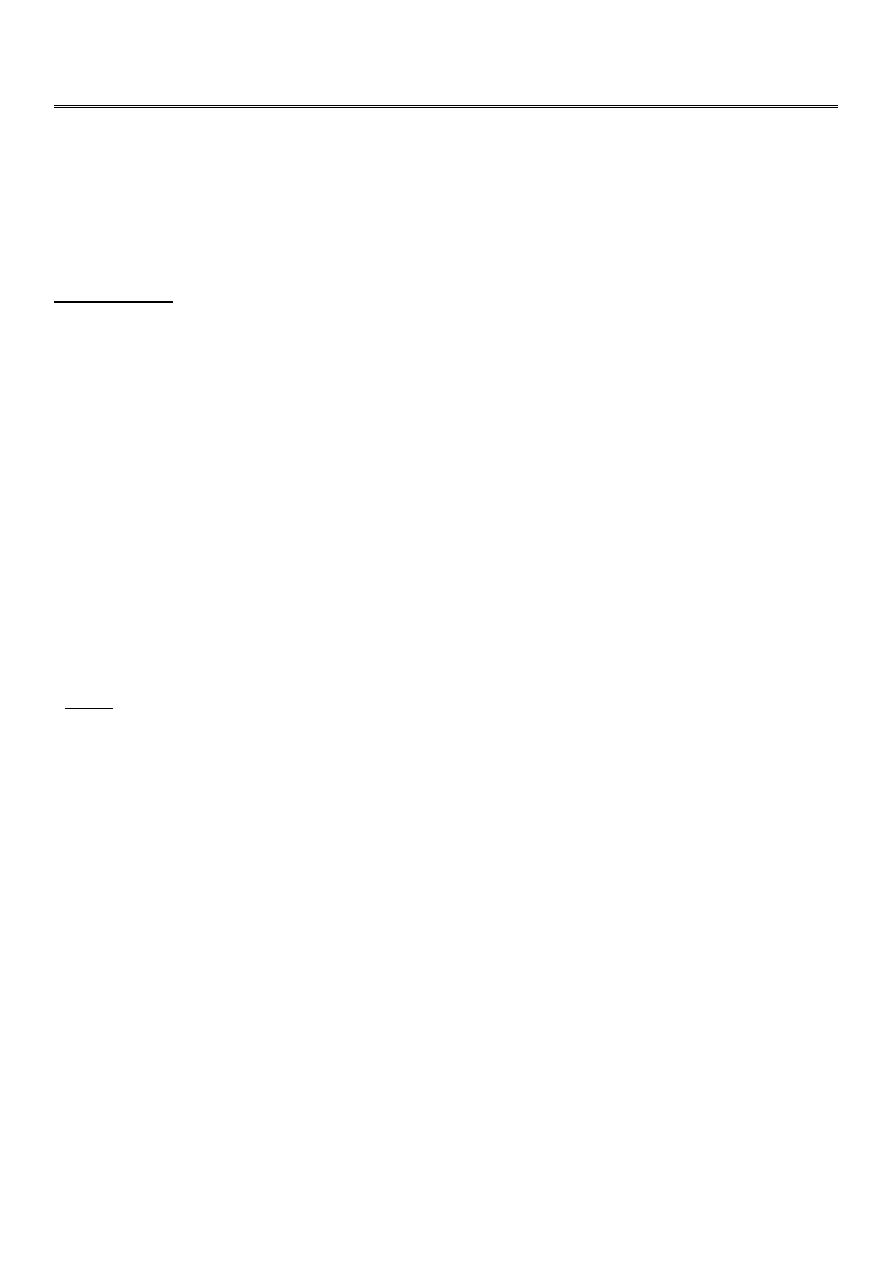
Palpation:
o Tragal tenderness: due to otitis externa.
o Tenderness on mastoid bone: due to acute
mastoiditis.
Inspect the external auditory meatus:
o Pull pinna upwards, outwards and backwards
o In infants downwards and backwards
o In children pull backwards
o See: Otorrhoea, otomycosis, Wax, Canal stenosis, Exostoses, osteomas.
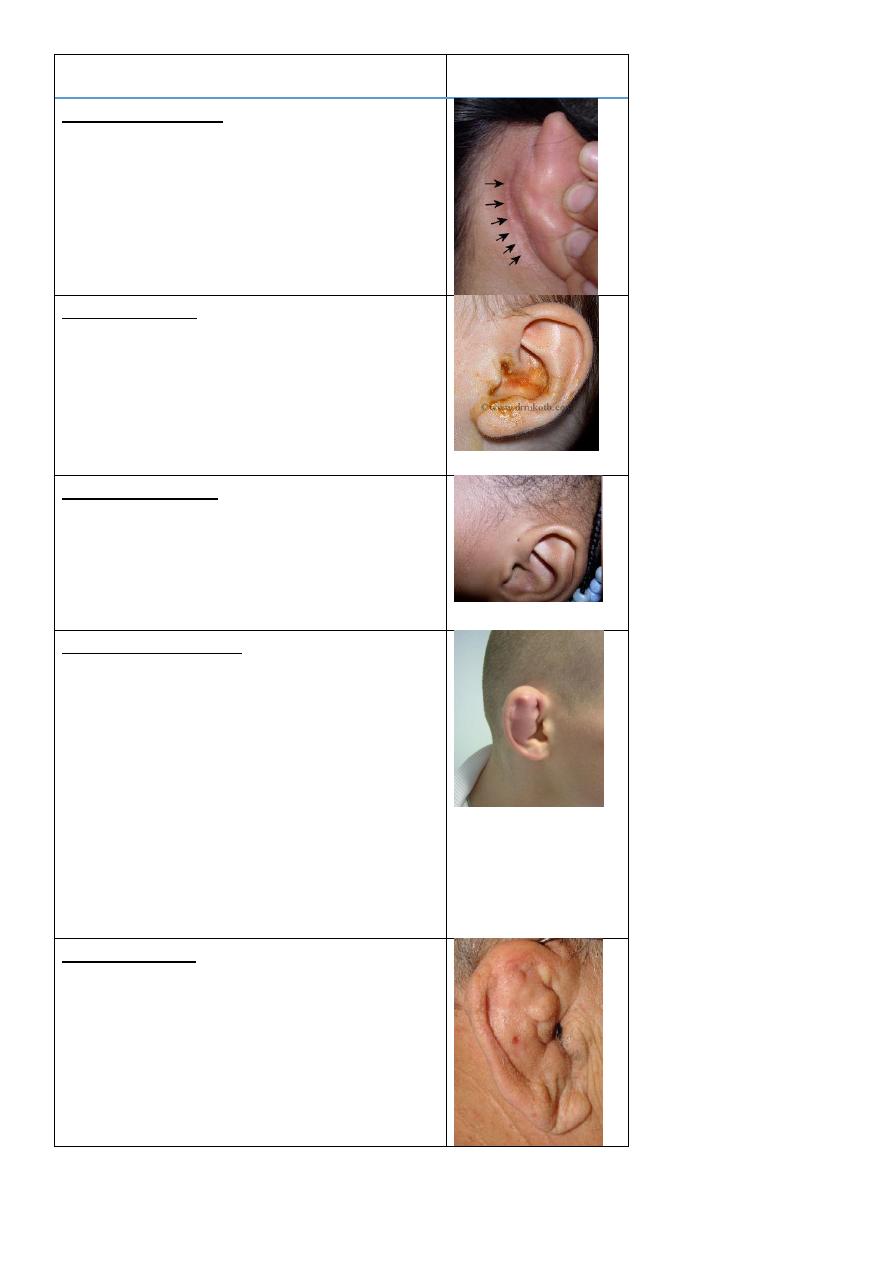
There are three methods of inspection of external auditory meatus:
1- Aural (ear) speculum:
o It is unaided eye method:
o Use head light or mirror.
o The pinna is pulled upward and backward.
Findings:
o Wax.
o Otitis externa: red, pain, pus.
o Otomycosis: due to candida albicans (white) or aspergillus niger (dots) both
called wet newspaper.
o Foreign body: very severe irritation / put light or esperto or oil.
Wax,
Conductive hearing
loss
Otomycosis
Otitis Externa
Foreign body in the ear
5
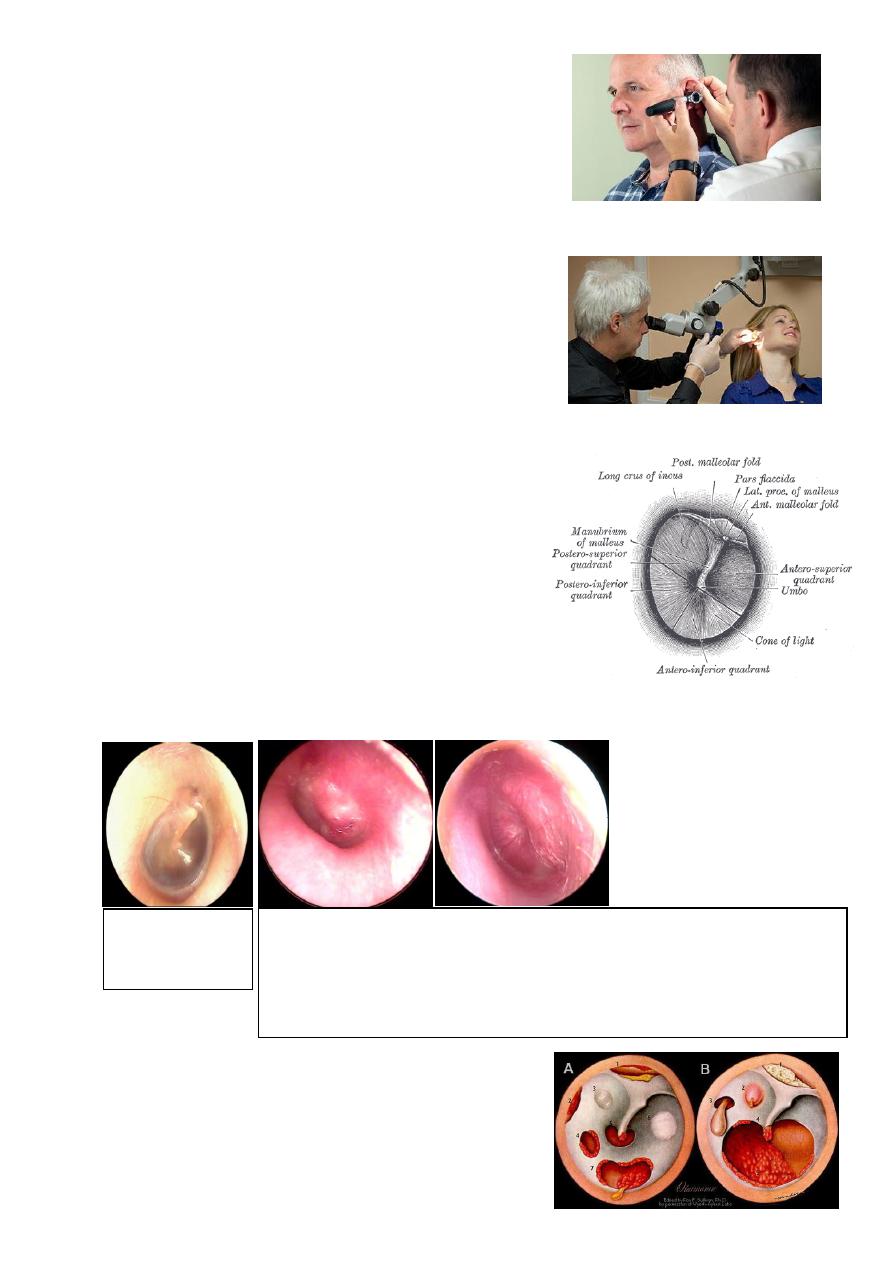
2- Otoscope:
o It is aided eye method.
o Examine right ear with right hand.
o Pull the pinna upward, outward and backward.
o The auroscope magnification is 1.5-2.0 times.
3- Microscope:
o It is aided eye method.
o Its magnification is 6-20 times.
o Uses:
o 1-detailed examination of the ear (magnified up
to 6-20 times)
o 2-certain surgical operations
o 3-biopsy
o 4-cleaning
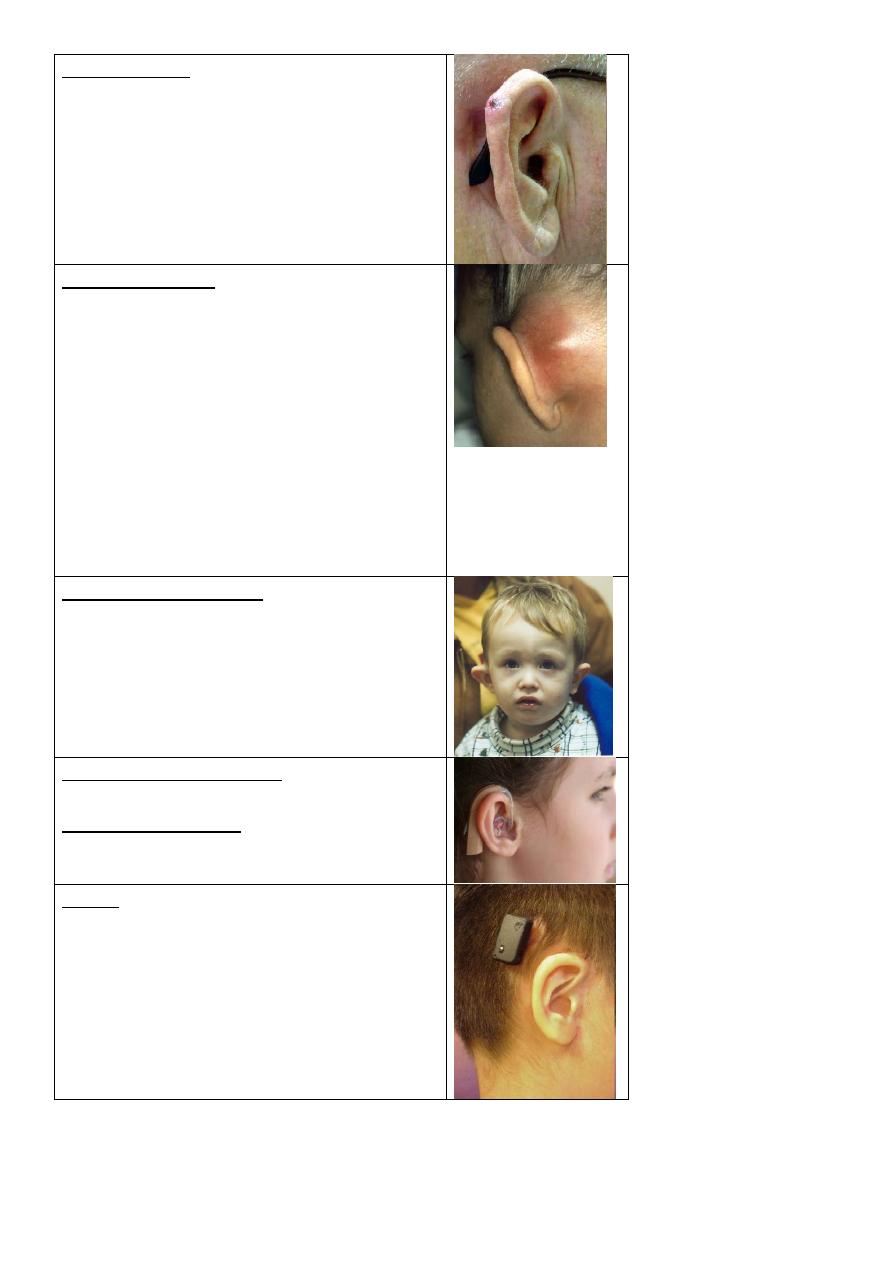
Examination of the tympanic membrane:
o Oval – pearly gray color.
o There is handle of malleus.
o There is cone of light shatter اختفاءthe cone
of light when the tympanic membrane is pulled
or pushed.
o Divided by two lines into 4 quadrants.
Tympanic membrane perforations:
o Causes :
1-trauma
2-infection
3-iatrogenic (medical mistakes)
Normal
tympanic
membrane
Congested tympanic membrane with loss of cone of light, redness and
pulging of the membrane
Dx: acute otitis media
Pain occur at night because there is no swallowing (eustachian tube is open)
6
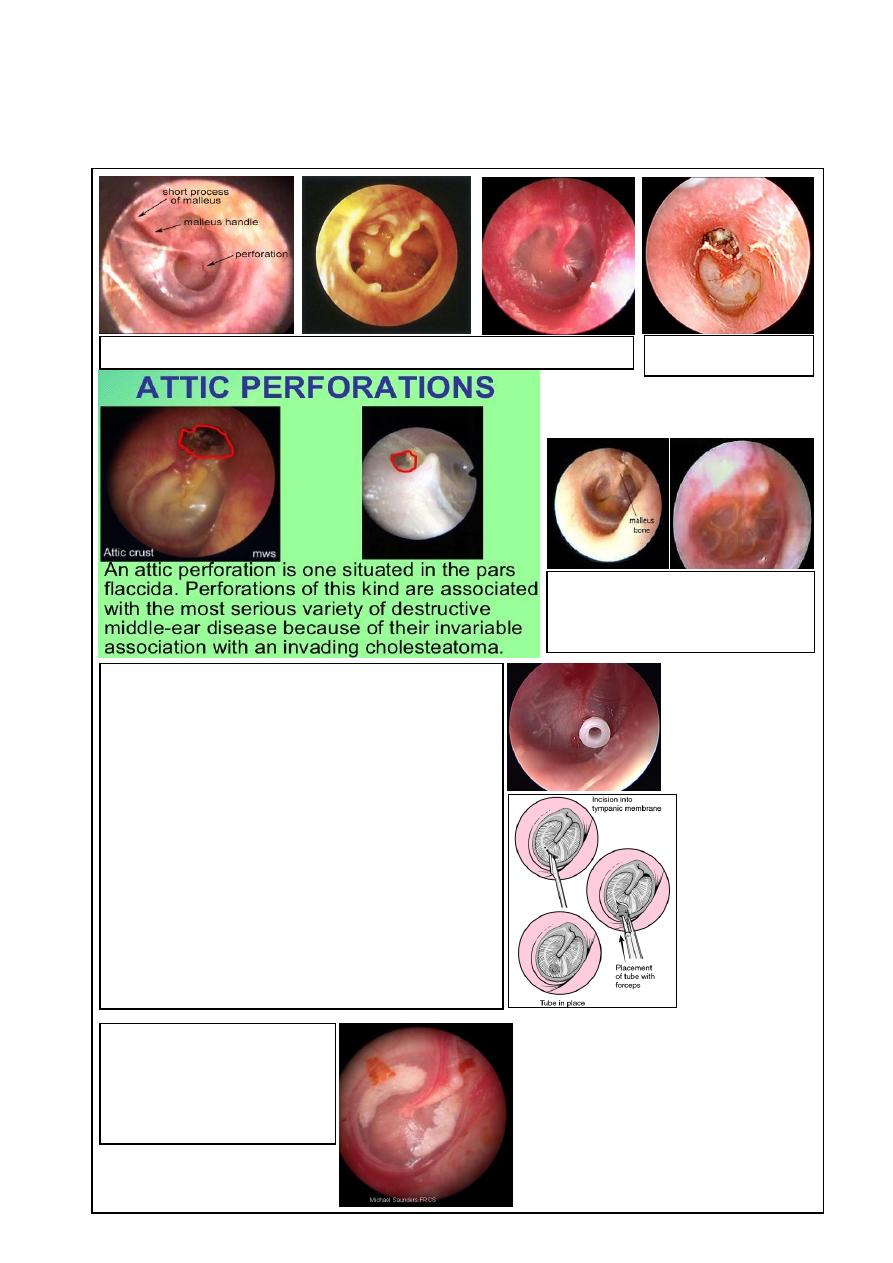
o Types of perforation:
1- Safe (Central) the perforation is surrounded by part of the tympanic
membrane.
2- Unsafe (Marginal and Attic perforations).
cholesteatoma
Otitis media with effusion
Eustachian tube dysfunction is
the commonest cause
Myringotomy with insertion of Grommet
ventilation tube
-indication
1-CHRONIC O.M. with effusion (commonest in
child)
2-recuurent O.M.
3-Eustachian tube dysfunction with recurrent s and
s (commonest in adult)
4-recuurent episodes of barotrauma
Complication: blockage , otorrhea , chloesteatoma ,
tympanosclerosis
Tympanosclerosis
Precipitation of ca carbonate
after healing of repeated
perforation or myringotomy
Perforation of the tympanic membrane
7
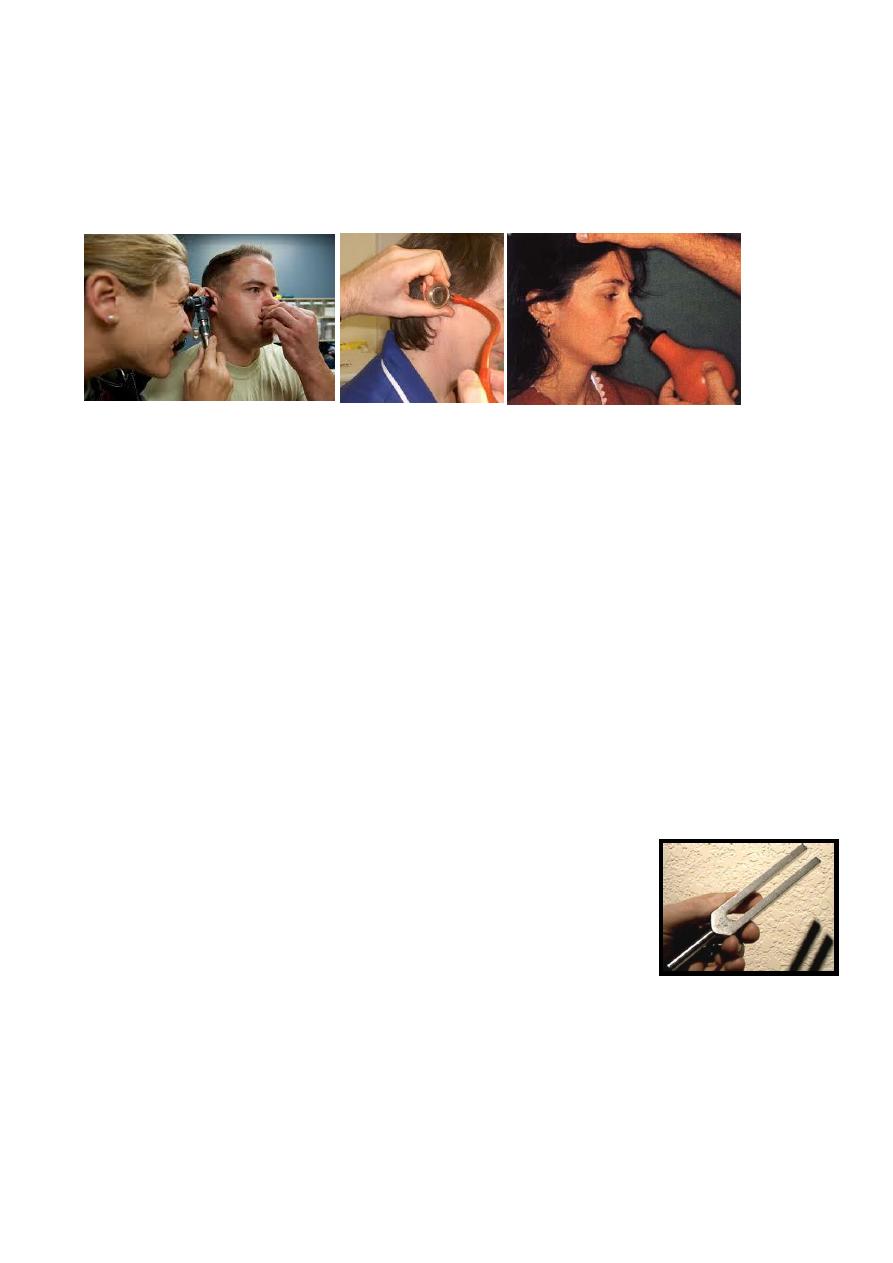
Assessment of tympanic membrane mobility
o Valsava manover (close mouth and nose and swallow)
o Seigle pneumatic speculum (also used for magnification)
o Politzerization (balloon in the nose and drink water)
o Causes of fixed tympanic membrane fluid behind the membrane (otitis media),
fibrosis, calcifications (tymeno-sclerosis), perforation.
Assessment of Hearing
o While assessing the auditory function it is important to find out:
Type of hearing loss ( CHL, SNHL or mixed )
Degree of hearing loss.
Site of lesion.
Cause of hearing loss.
o Causes of conductive hearing loss:
Sclerosis of bone.
Calcification of oval window.
Fluid behind the membrane.
o Clinical tests of hearing:
Finger friction test: rubbing the thumb and finger close to the ear.
Watch test: by clicking watch.
Speech (voice) test: conversation voice, distance of 6 meters.
Tuning fork tests.
o Tuning fork tests:
Traditionally 512Hz ( )االهتزاز أطول لهذا التردد
Rinne and Weber (they were both German)
Help differentiate between conductive and sensorineual
hearing loss
o Rinne`s test:
Compare Air and Bone conduction in the same ear
Normal subject = AC > BC (Rinne +ve)
CHL = BC > AC (Rinne -ve)
SNHL = AC > BC (Rinne +ve) and often the BC is not heard.
False negative Rinne in very severe SNHL.
o Weber test:
In normal subjects the sound is heard in the midline or in both ears equally.
8
In CHL the sound is heard in the affected ear (absence of environmental noise),
i.e.; lateralized toward the affected ear
In SNHL the sound is heard in the non-affected ears.
Assessment of Balance ( Labyrinthine function)
Cranial nerves examination
=================================================================
2- The Nose:
Symptoms of the nose:
Discharge (rhinorrhea).
Epistaxis.
Obstruction or block causes of nasal obstruction:
o Vestibule: big boil.
o Nasal cavity: turbinate hypertrophy, septal deviation, sinusitis, polyp.
o Post-nasal space: tumor, adenoid hypertrophy (it is the most common cause of
nasal obstruction in children)
Nasal fetor:
o Unilateral offensive nasal discharge in children foreign body.
o Unilateral offensive nasal discharge in adult rhinolith, tumor, chronic infection.
Examination of the nose:
Introduce yourself
o Any hyponasal speech (rhinolalia clausa )?
Position the patient
o Head-mirror or headlight?
Inspect the external nose
o Compare nose to rest of face
o Size
o Skin
o Swelling, bruising, ulcers
o Rhinophyma:
Due to untreated rosacea (heavy alcohol aggravate it)
Treatment: carbon dioxide laser or complete excision with skin graft)
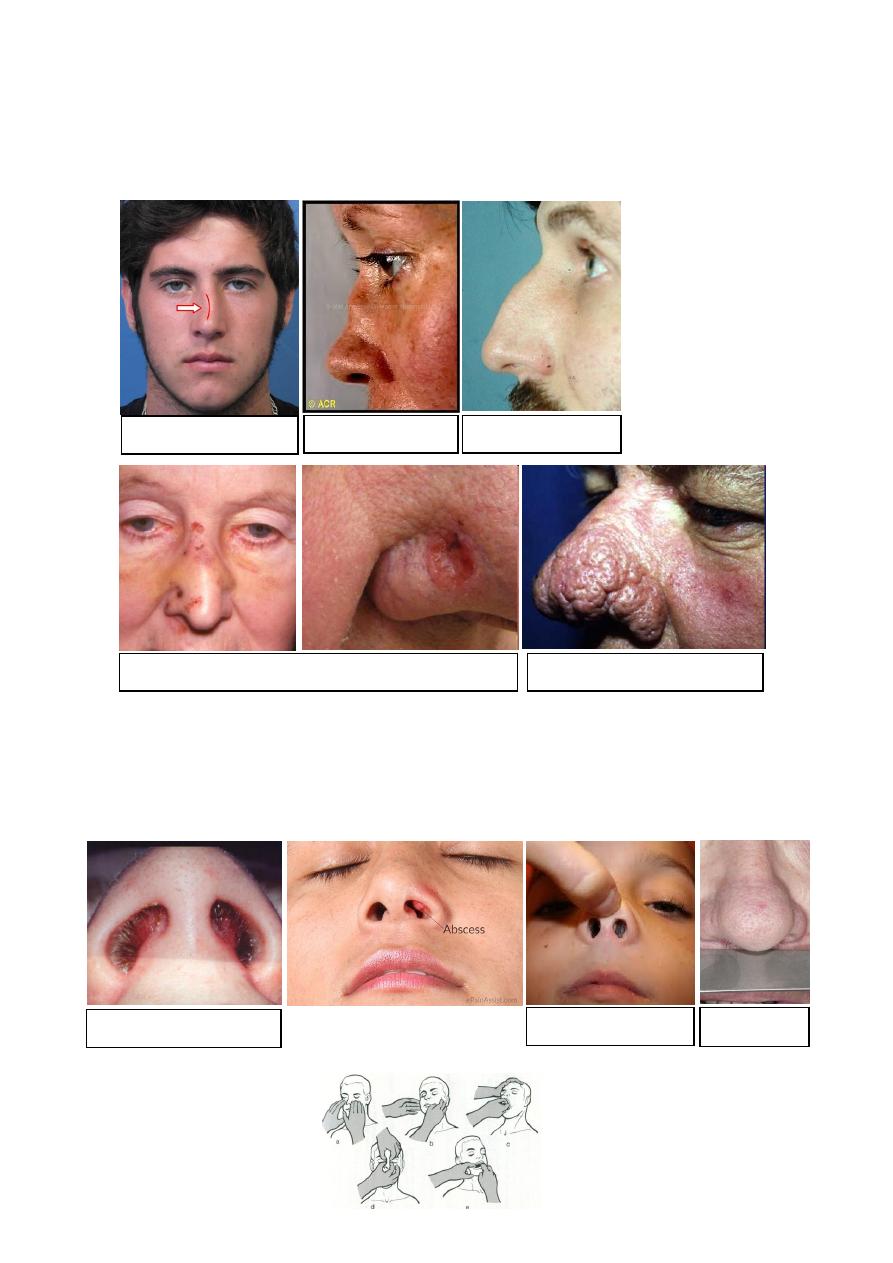
9
o Shape
Banana nose=deviated nose trauma, septal deviation.
High arched nose=roman nose=prominent nose Congenital, Trauma.
Saddle nose HOT SALT (septal haematoma
_operation_trauma_syphilis_septal abscess_leprosy_TB)
Examine the nasal tip, vestibule, and assess the nasal airways
o Nasal tip elevation of nasal tip to see the vestibule.
o Nostrils and air flow
o Mist test For airway patency
Palpation and Percussion
Deviated nose
Saddle nose
Prominent nose
Ulcer
Rhinophyma
Elevation of nasal tip
Septal hematoma
Mist Test
11
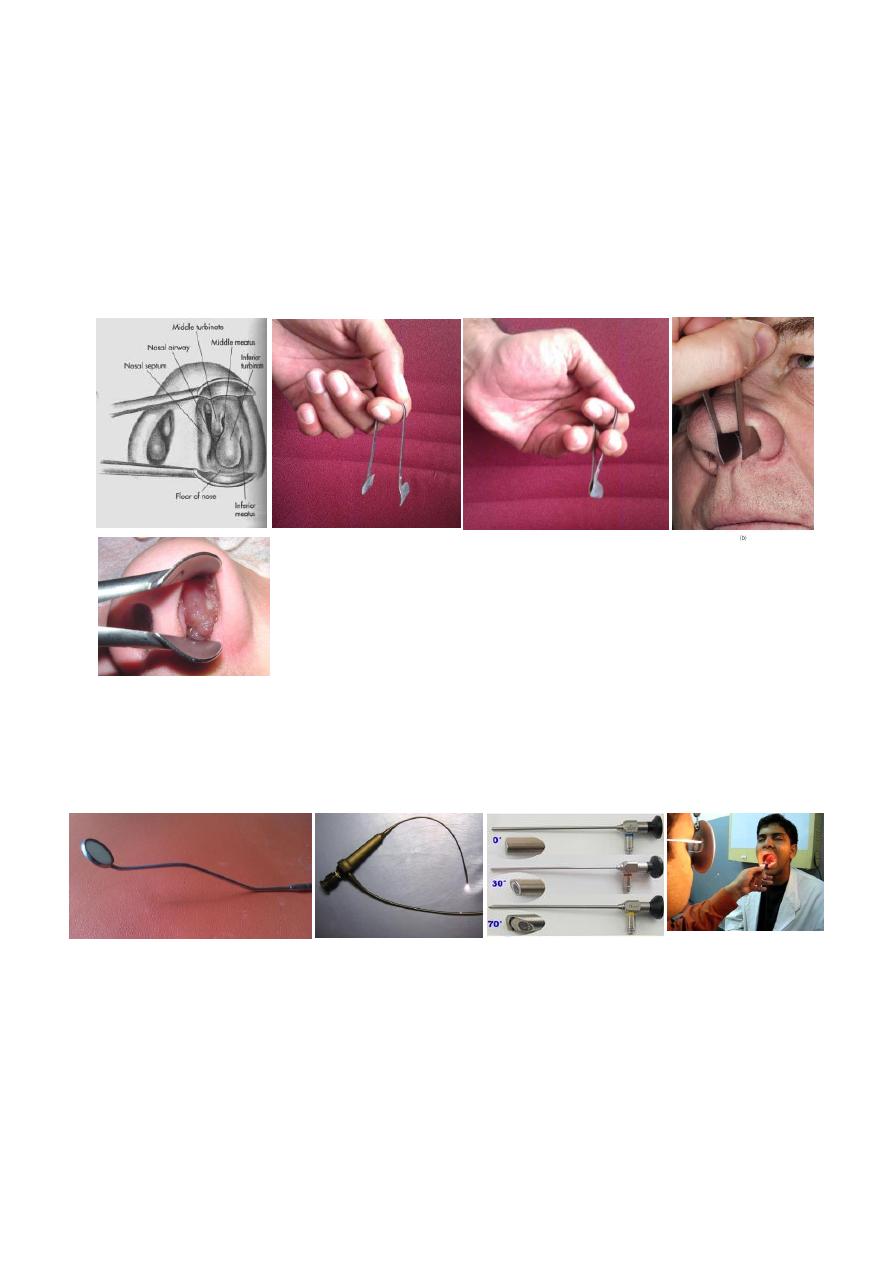
Anterior rhinoscopy:
o Thudichum’s speculum, Killian speculum, otoscope?
Obvious lesions
Mucosa
Septum
Turbinates (and osteomeatal complex)
o Thudichum’s nasal speculum
Used to examine the nasal cavity.
See septum, floor of nose, middle and inferior turbinate, middle meatus.
Polyp
Post nasal space examination:
o With mirror ( nasopharyngeal mirror) (also use tongue depressor)
o Rigid endoscope
o Flexible endoscope
=================================================================
11
3- The Throat:
Symptoms of the throat:
Horsiness (don’t horsiness of the voice, but only horsiness).
Sore throat.
Dysphagia and odynophagia.
Cough.
Strider.
Examination of the throat:
Introduce yourself
Position the patient:
o Headlamp, mirror or other light source
o Seated in chair with space to examine from all sides
Assess speech:
o Stridor
o Hoarseness
o Any other dysphonia
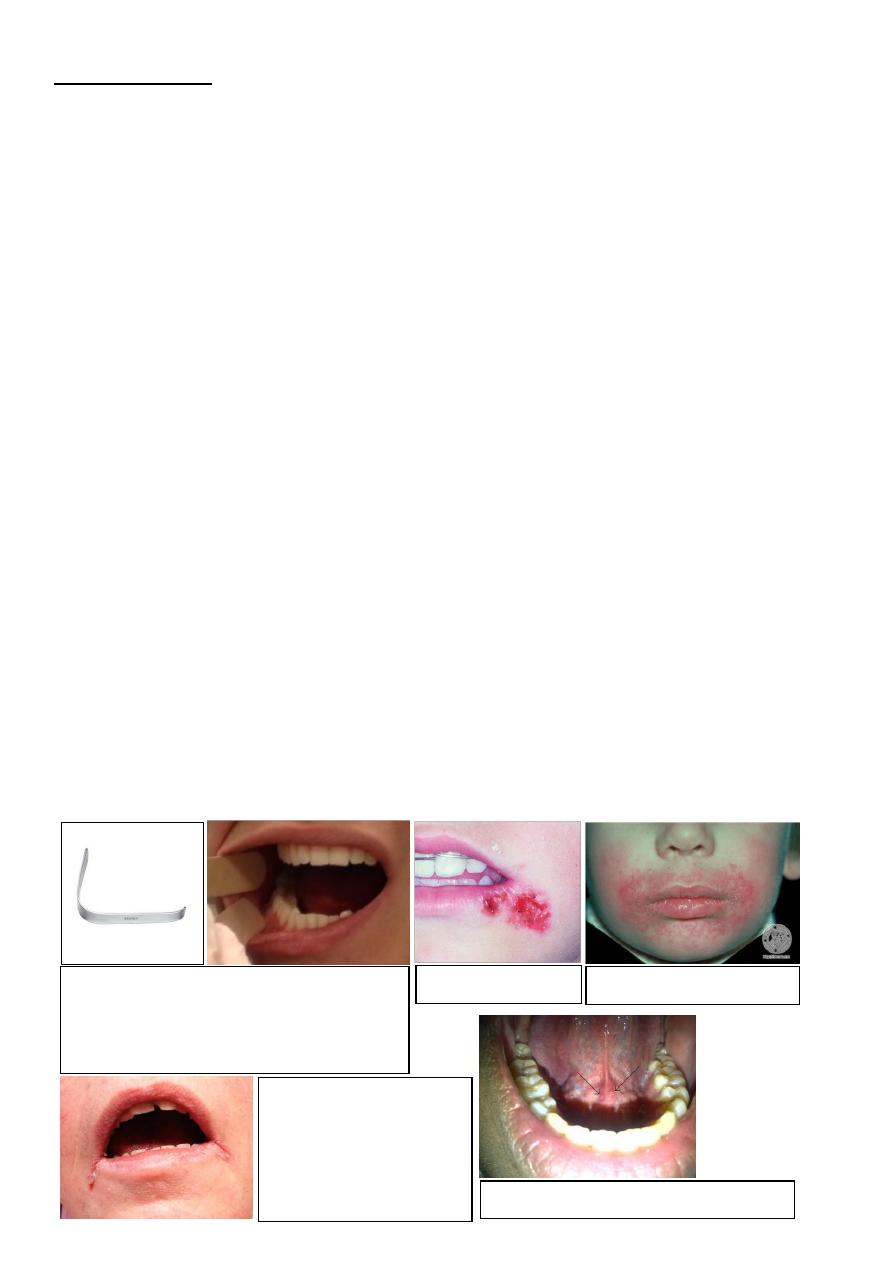
Oral examination
o Lips, perioral lesions
o 1 or 2 tongue depressors
o Inspect tongue, buccal mucosa and oropharynx
o Salivary duct orifaces
o Say ‘Ahhh’ (movement of soft palate) // Say 'Eeee' (movement of vocal cords)
o Finger examination of floor of mouth, cheeks
Tongue depressor
Used for examination of oral cavity and oropharynx
Can use with nasopharyngeal mirror r to examine posterior
nasal space.
Herpes labialis
Peri-oral eczema
Angular stomatitis:
Iron d. anemia
Vit. B. deficiency
Bacterial
Fungal
Contact dermatitis
The orifice of sublingual duct of Brtholine
12
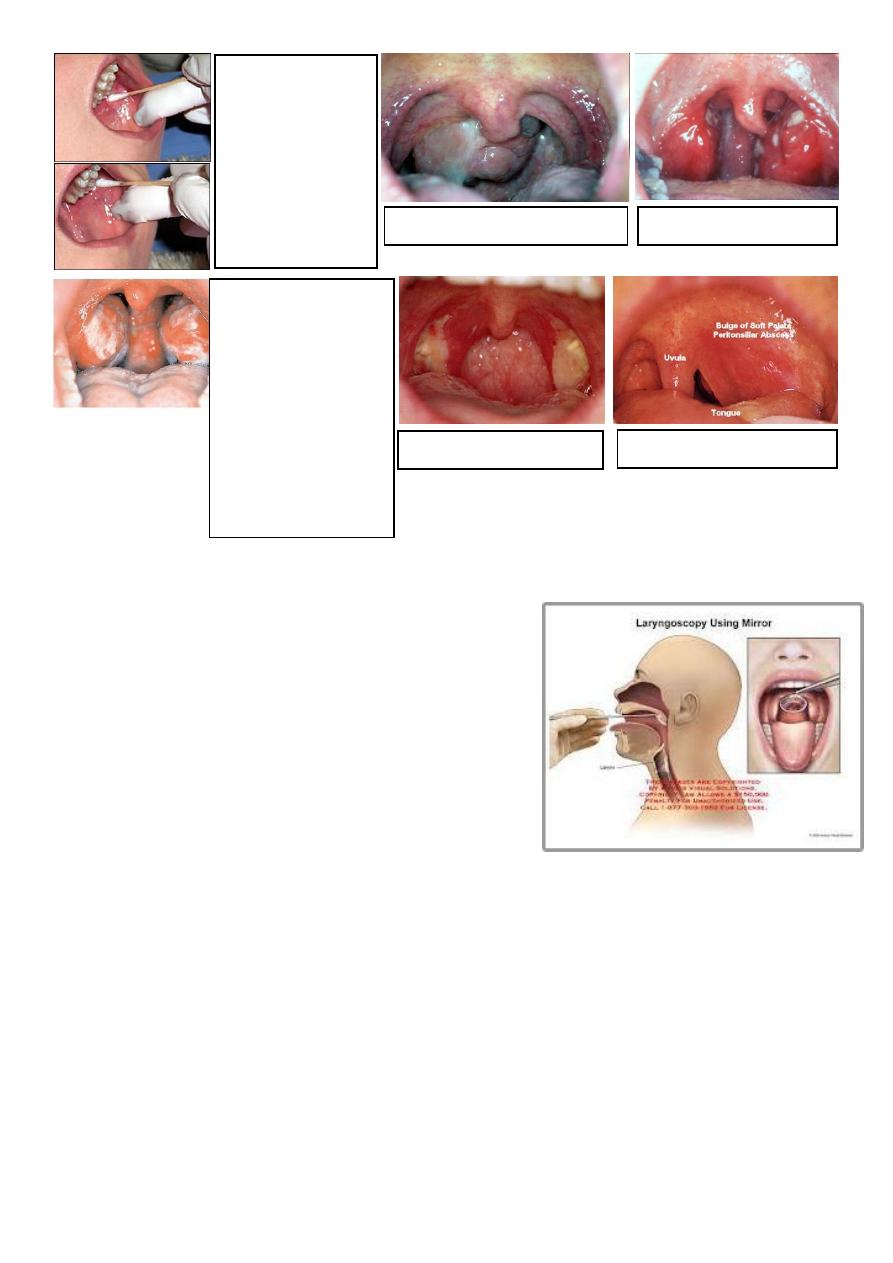
Indirect laryngoscopy
o With mirror or nasendoscope
o Can assess the base of the tongue, vallecula,
Epiglottis, false and true vocal cords.
o Look for abnormality in the mucosa ( e.g.
congestion , mass, vocal cord nodule>>>)
o Check vocal cord mobility by asking the patient
to say (EEE)
o The mirror is warmed before examination to
avoid fogging
Examination of neck
o Head and neck cancers metastasise to neck nodes and to the lungs
o Tonsillar infections are the commonest cause of enlarged lymph nodes
o Skin Skin lesions, Ulceration, Scars and wounds, Stoma, Obvious large masses.
o Swallow Larynx should rise, a goitre may rise, too.
o Examine from behind Let patient know what you are doing, Tender areas,
Gentle, One side at a time.
o Lymph nodes in the anterior and posterior triangle
o Thyroid gland
o Laryngeal skeleton
o Position of trachea
Parotid gland orifice
Using gauze to dry
the area and
watching the flow
by pressing above
Stenson’s duct is a
good indicator of
salivary flow.
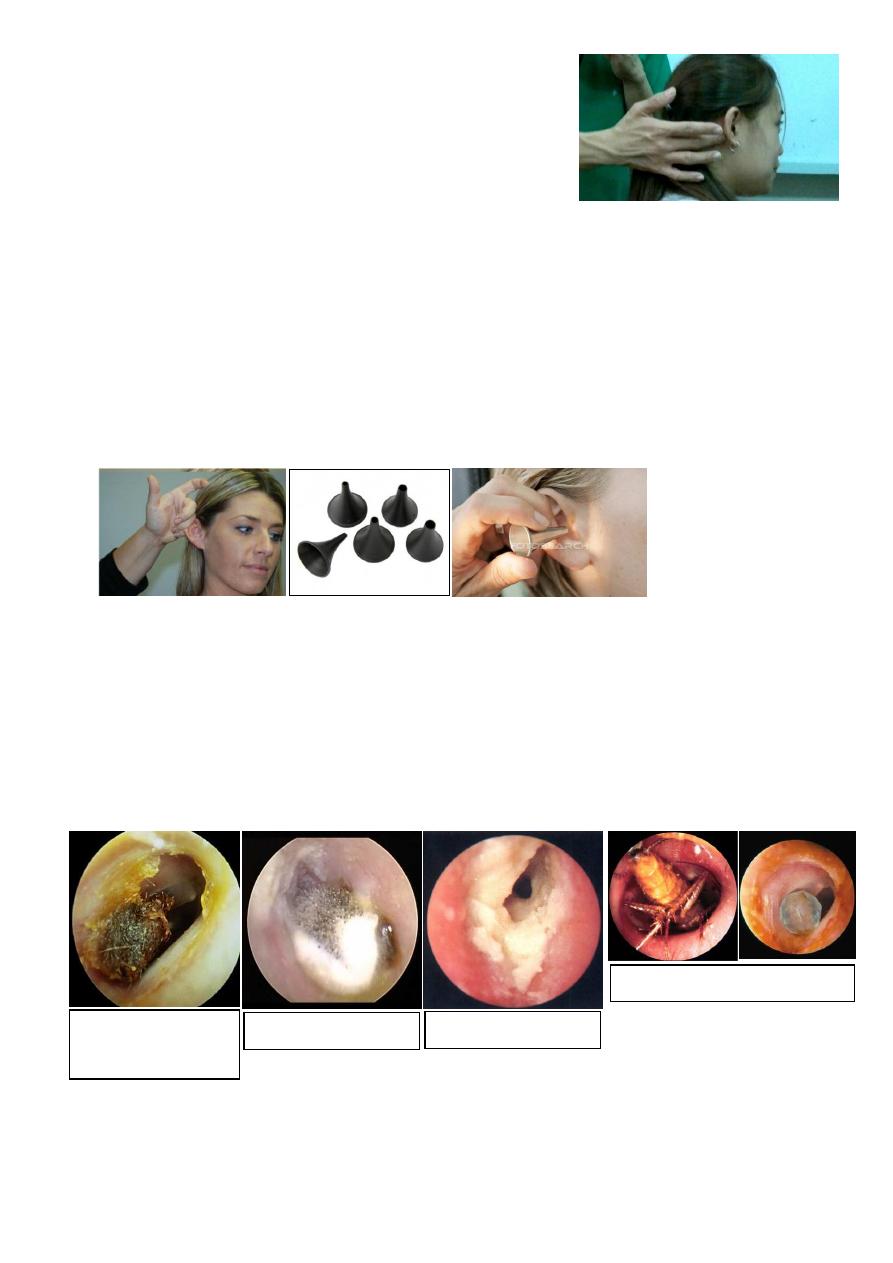
Antrochoanal polyp
Acute follicular tonsilitis
Membranous tonsilitis
DDx:
Diphtheria
Fungi
IMN
Vincent angina
Mention 2 Ix:
WBC count
throat swab
Post-tonsillectomy
Peritonsillar abscess
