1
Fifth stage
ENT
Lec-9
د.سعد
7/12/2015
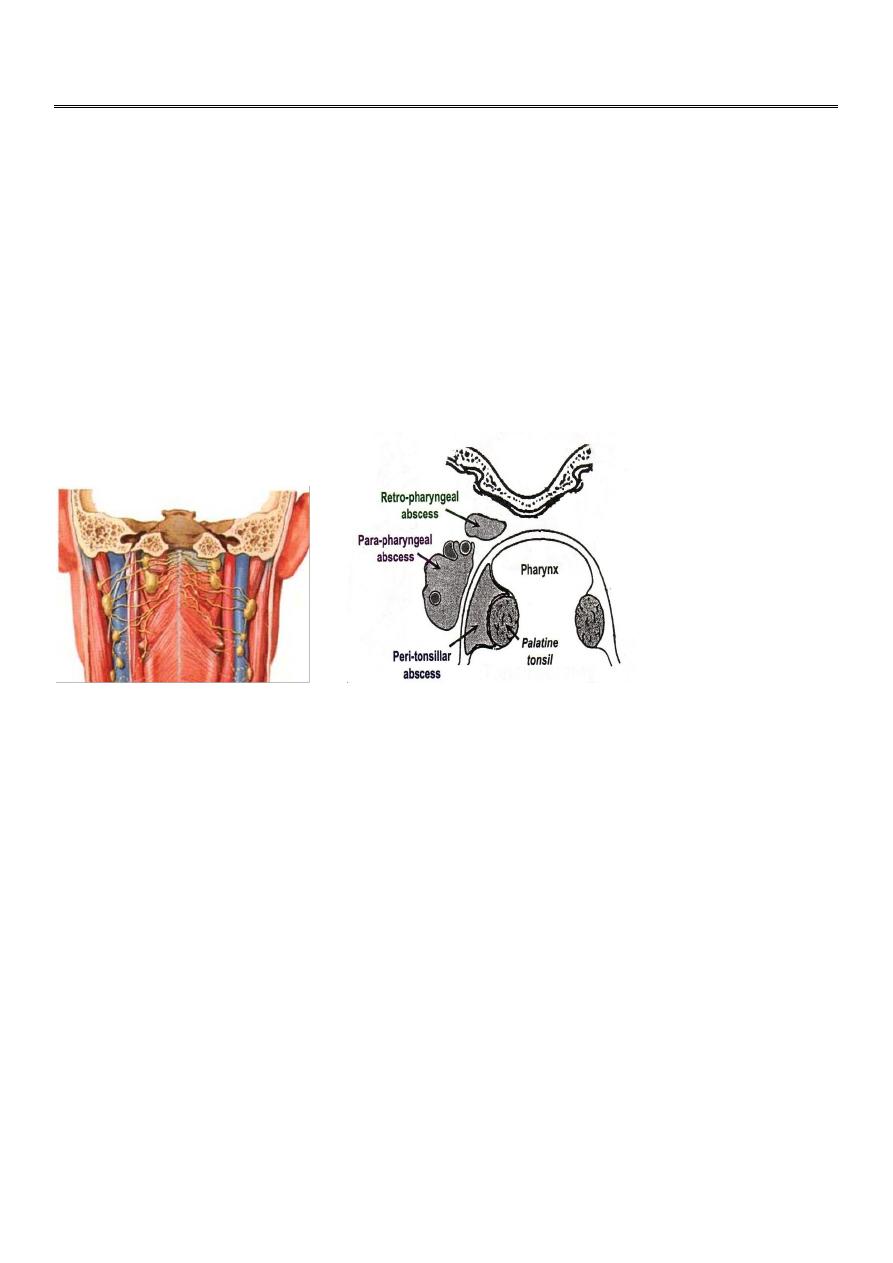
Infection of the Pharyngeal Spaces
Parapharyngeal Abscess
Definition: Collection of pus in the parapharyngeal space which is a
connective tissue space lies on
the lateral side of the nasopharynx and oropharynx and extends from skull base to hyoid bone.
It contains:
1. Great vessels of the neck; common carotid artery and internal jugular vein.
2. Last 4 cranial nerves
3. Cervical sympathetic trunk
4. Deep cervical lymph nodes
Aetiology:
1. Acute Tonsillitis or after tonsillectomy or after bursting of peritonsillar abscess: The infection
passes through the superior constrictor muscle.
2. Infection or extraction of last lower molar tooth.
3. Infection of the parotid salivary gland.
4. Extension of mastoid infection ( Bezold's abscess).
5. Spread from retropharyngeal abscess.
Symptoms:
Occurs mostly in adolescents and adults
1. The patient is feverish, ill and toxic.
2. Acute sore throat.
Signs:
a)
The patient is severely ill with high pyrexia and possibly dehydrated.
b)
The lateral pharyngeal wall & tonsil are pushed medially.
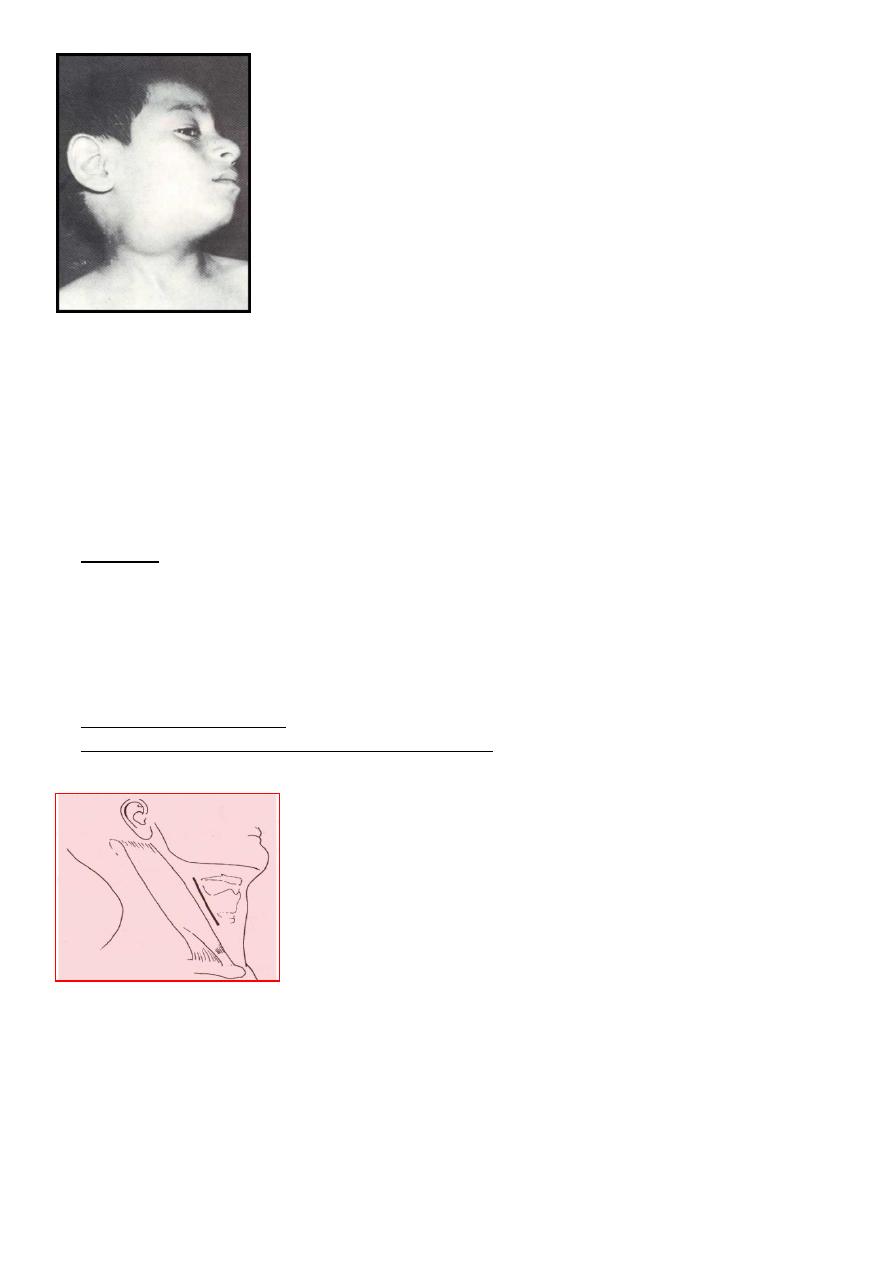
2
c)
There is a unilateral diffuse tender swelling
in the upper part of the neck, below & behind
the angle of the mandible, deep to the anterior
border of the sternomastoid. The neck is tilted
to the diseases side.
d)
Trismus due to spasm of ptrygoid muscles.
Investigations:
1. Full blood count and estimation of urea and electrolytes and blood glucose should be
performed (to exclude immune compromised diseases).
2. Lateral soft tissue neck radiograph, CT & MRI.
Complications
Spread to
1. Skull base: causing meningitis
2. Carotid sheath causing thrmbophlebitis of the internal jugular vein with septicaemia and
erosion of carotid artery.
3. Mediastinum ( along the carotid space) causing mediastinitis
4. Larynx: causing laryngeal oedema
Rupture into the pharynx: aspiration of pus will cause bronchopneumonia
Cranial nerves and sympathetic chain involvement leading to Horner's syndrome.
Treatment
Medical: massive antibiotic therapy.
Surgical drainage
A vertical incision at the anterior border of
the sternomastoid muscle with wide exposure
of the affected neck space and insertion of
large drain.
Acute Retropharyngeal Abscess
Definition: Collection of pus in the retropharyngeal space
.
What is retropharyngeal space?
It is a connective tissue space between the buccopharyngeal fascia & pre-vertebral fascia. The space
is divided into 2 compartments by a fibrous raphe (spaces of Gillette). Each lateral space contains
retropharyngeal lymph nodes which usually atrophy at the age of 5
years old.
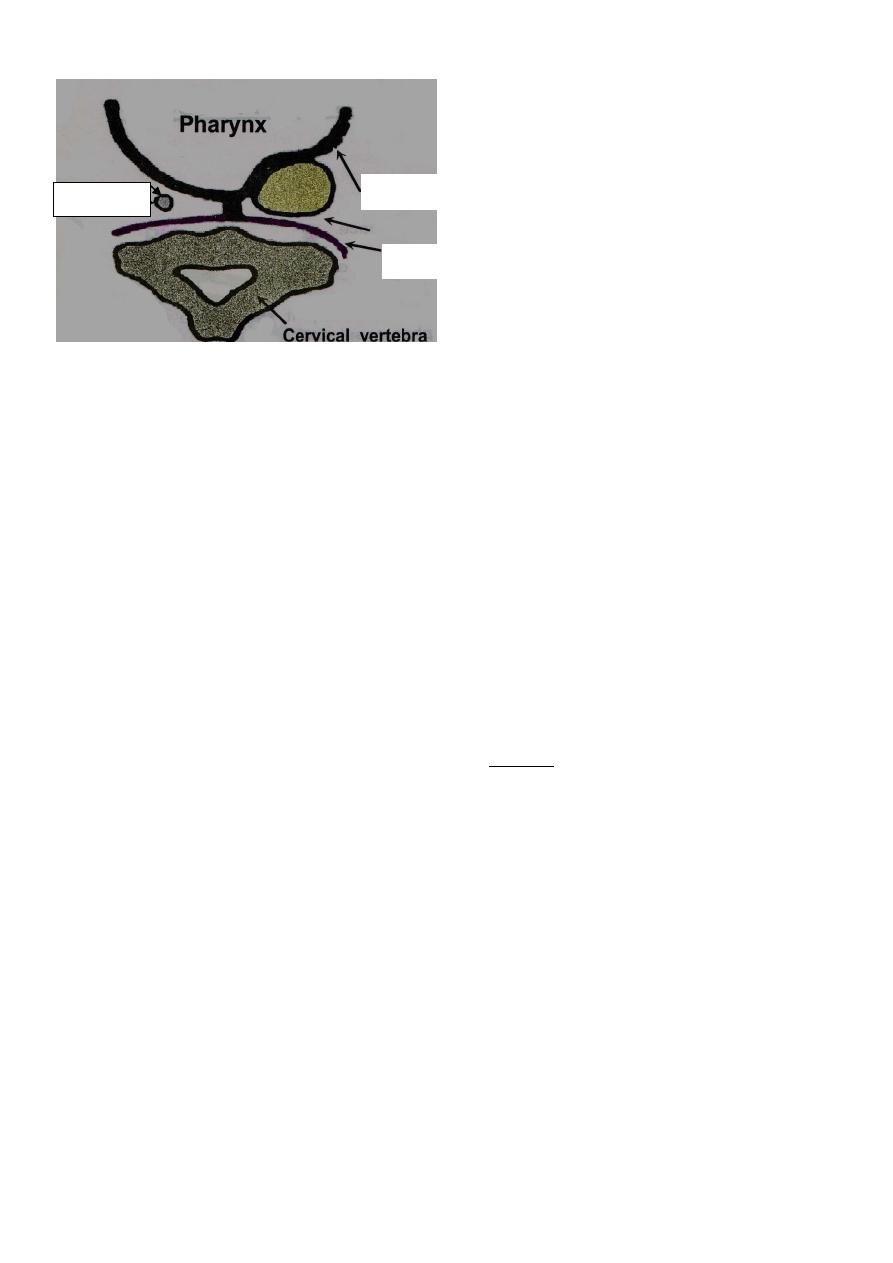
3
It extends from the skull base to the superior mediastinum (bifurcatioin of the trachea).
Age: below the age of 5 (The Retropharyngeal LN atrophy at the age of 5)
Site: at one side of the midline (The two fasciae are attached to each other at the midline by median
raphe.)
Aetiology: it is the result of suppuration of retropharyngeal lymph nodes ( LN of Rouviere)
secondary to:
1. Upper Respiratory Tract Infection.
2. After Adenoidectomy operation.
3. Impacted foreign body or penetrating injury of posterior pharyngeal wall.
Clinical features
The patient is usually a child below 5 years who present with acute onset of:
High pyrexia.
Sore throat with pain and discomfort on swallowing and the patient may drool saliva. .
Stridor and croupy cough may present.
Torticollis. The neck becomes stiff and the head is kept extended.
Bulge in posterior pharyngeal wall. Usually seen on one side of the midline.
Cervical lymphadenopathy.
Investigations:
Radiograph of soft tissue lateral view of the neck & CT scan:
Widening of prevertebral space with
normal vertebral bodies.
Complications:
1- Spread to mediastinum causing mediastinitis.
2- Rupture into the pharynx: aspiration of pus will cause bronchopneumonia.
Treatment:
Medical: massive antibiotic therapy.
Surgical drainage: Incision in the posterior pharyngeal wall with the patient in the Trendlenberg
position why? In this position the head is lower than the chest to avoid aspiration of pus.
Tracheostomy if indicated.
Retropharyngeal LN
buccopharyngeal fascia
Pre-vertebral fascia
4
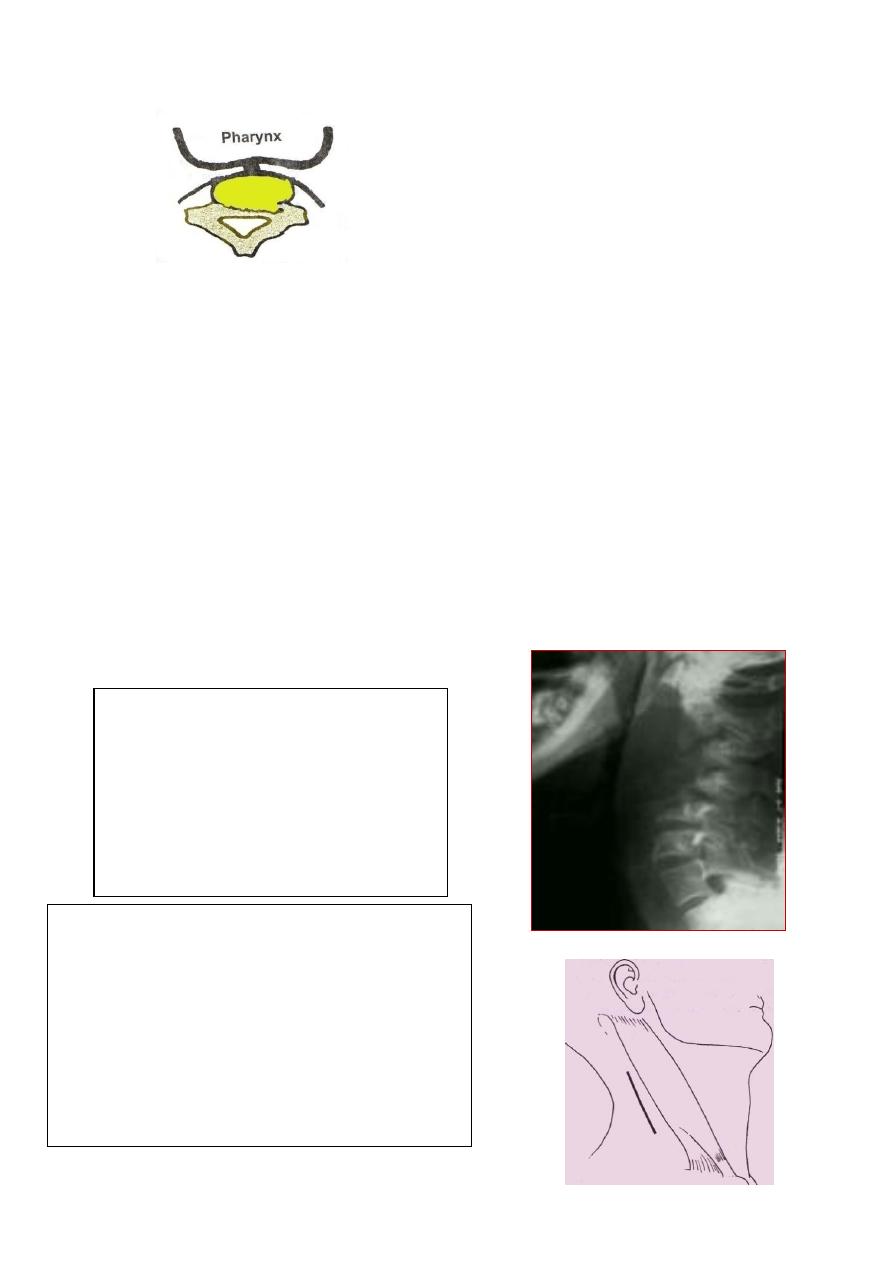
Chronic Retropharyngeal Abscess (Pre-vertebral or Pott's Abscess)
Definition:
Formation of a cold abscess in
the pre-vertebral space.
What is the pre-vertebral space?
It is a space between the cervical vertebrae
and the pre-vertebral fascia.
Aetiology:
Pott’s disease: i.e. tuberculosis of cervical vertebrae. Here the abscess rupture through the
prevertebral fascia and reaches the retropharyngeal space.
Clinical picture
Occur in older children, adolescents and adults. It is of slow onset and present as:
1. Night sweets, night fever, loss of weight, loss of appetite.
2. Pharyngeal discomfort rather than pain.
3. Mild dysphagia.
4.
Limited painful neck movement
.
Signs:
The patient looks pale with low grade fever and loss of weight.
Painless swelling lies in the midline of the posterior pharyngeal wall.
Enlarged painless cervical lymph nodes.
Investigations:
Plain X ray and CT scan of the neck:
1. Widening of prevertebral space.
2. Destruction of the cervical
Vertebrae
Treatment:
1. Medical: Antituberculous therapy.
2. Surgical Drainage: Through a vertical
incision along the posterior border of the
sternomastoid muscle. The drainage should
never be through the mouth to avoid
secondary infection.
3. Orthopedic management
5
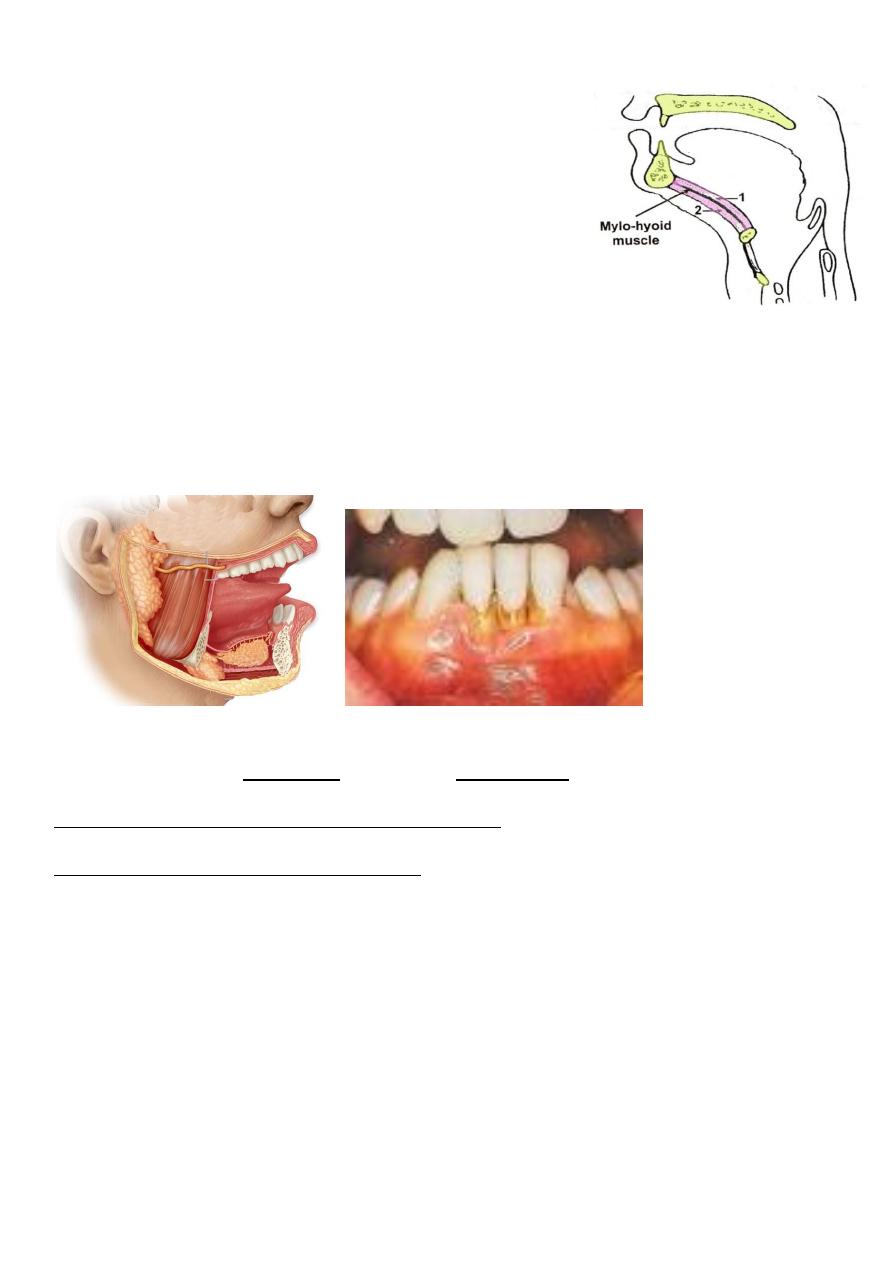
Ludwig’s Angina
Definition:
It is infection of submandibular space. This space lies
between the mucus membrane of the floor of the mouth and
tongue on one side and superficial layer of deep cervical fasci
a
extending between the hyoid bone and mandible
on the other. It
is divided into two compartments by the mylohyoid muscle:
1. Sublingual compartment ( above the mylohyoid)
2. Submaxillary and submental compartment (below the
mylohyoid).
Aetiology
1- Root abscess of the lower premolar & molar teeth (80%). The most usual organisms are
streptococcus veridans and E coli.
2- Suppuration of submandibular gland itself (submandibular sialadenitis).
3- Tonsillar infection, injuries to the oral mucosa and fractures of the mandible account for other
causes.
Clinical features
The patient is ill, toxic (fever > 38°C) with marked odynophagea and drooling of saliva and there is
varying degree of trismus.
When the infection is localized to the sublingual space, structures in the floor of the mouth are
swollen and tongue seems to be pushed up and back.
When infection spreads to submaxillary space, the submental and submandibular regions become
swollen and tender and impart woody-hard feel. Usually there is cellulitis of the tissues rather than
frank abscess (non-fluctuantxzdrer5t677u8op;’loiuyioiudsd swelling). Tongue is progressively
pushed upwards and backwards threatening the airway. Laryngeal oedema may appear.
Treatment
Medical:
1- Massive Antibiotic therapy
2- Bed rest in semi-sitting position to avoid airway obstruction.
Surgical drainage:
If the state progress and the swelling increases, fluctuation should on no account be awaited
because it seldom occurs. Drainage is by a horizontal incision, 2cm below the angle of the mandible.
Usually there is no or little frank pus.
Tracheostomy: If indicated.
6
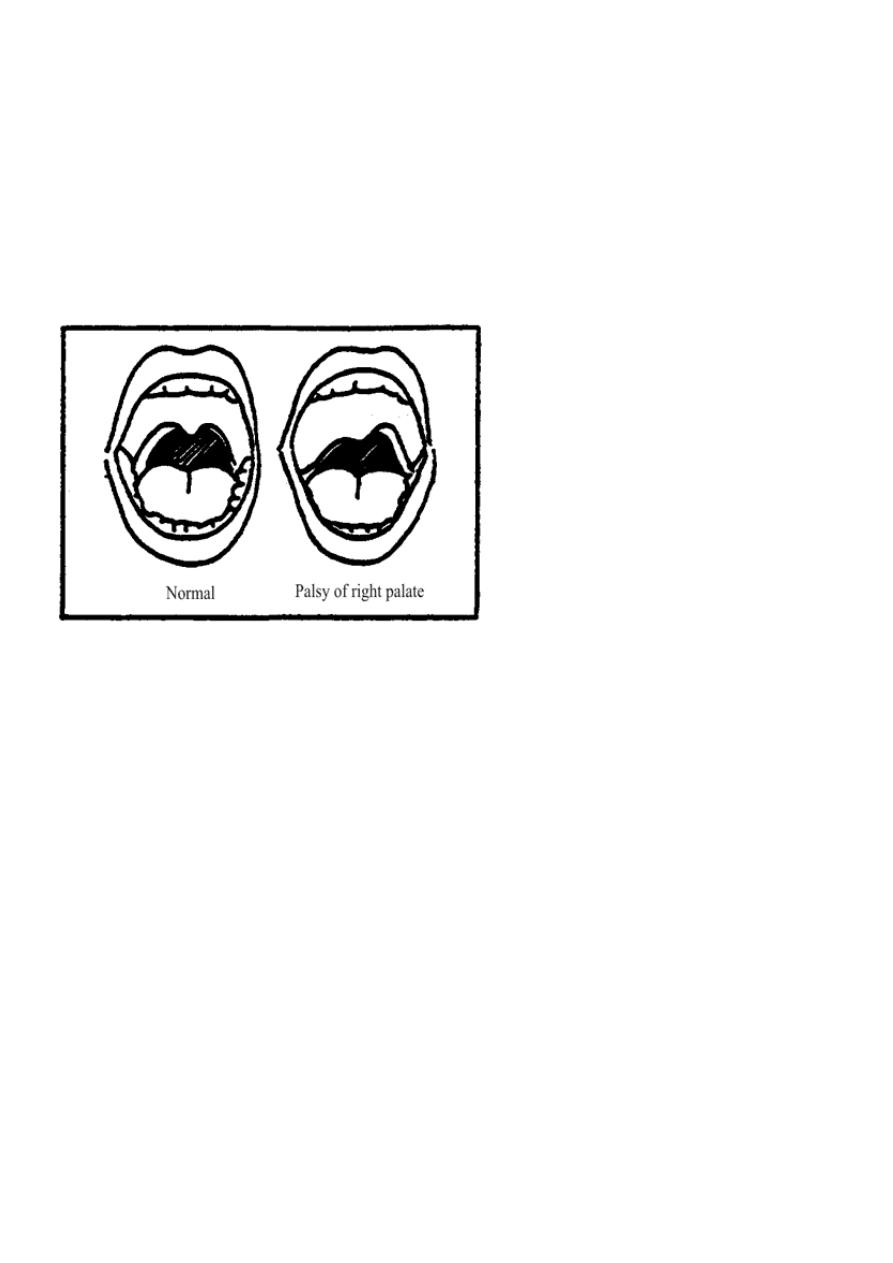
Paralysis of the palate and pharynx
Aetiology
1.
Idiopathic.
2.
Infection: Diphtheria and poliomyelitis.
3.
Neurological: Paralysis of lower 4 cranial nerves by lesions of the brainstem, jugular foramen
and upper part of the neck.
4.
Malignancy:
Nasopharyngeal malignancy
5.
Surgical trauma:
Tonsillectomy and adenoidectomy
.
Clinical Picture
Unilateral: The condition may be asymptomatic although the palate is pulled to the affected side.
Bilateral: Hypernasality (Rhinolalia aperta) and regurgitation of food.
Unilateral: The palate rises up to the healthy side.
Treatment:
1. Treat the cause.
2. In severe cases with regurgitation; nasogastric tube feeding is recommended.
Tumors of the pharynx
Juvenile Nasopharyngeal Angiofibroma
Is a vascular tumor of the nasopharynx occurring almost entirely in adolescent males (7-19 years
with a mean of 14 years). Although the tumor is benign, it is locally invasive and behaves as
malignant due to the anatomical structure of the nasopharynx.
Aetiology
The exact cause is unknown. As the tumor is predominantly seen in adolescent males in the 2
nd
decade of life, it is thought to be testosterone dependent. Such patients have a hamartomatous
nidus of vascular tissue in the nasopharynx and this is activated to form angiofibroma when male
sex hormone appears.
Clinical picture
1. The patient is nearly always a young boy with a mean age of 14 years.
2. Repeated attacks of epistaxis which can be extremely profuse due to absence of muscular coat
from the sinusoids.
3. Progressive nasal obstruction.
7
4. Nasal speech (Rhinolalia aperta).
5. Conductive deafness due to pressure on Eustachian tube.
Examination
Posterior rhinoscopy: smooth, rubbery lobulated mass in the nasopharynx.
Middle ear effusion.
Mass in the nasal cavity or on the check if the tumor has extended anteriorly or laterally.
Proptosis results from extension of the tumor to the orbit through the infraorbital fissure.
Investigation
X-ray of the base of the skull and a lateral view of the skull.
CT scan, MRI and MRA.
External carotid angiography.
Biopsy is contraindicated because of fatal bleeding.
Differential diagnosis
1. Antrochoanal polyp.
2. Nasopharyngeal carcinoma.
Treatment
1. Surgical excision: Haemorrhage is the main danger of operation, so adequate blood should be
prepared before operation.
2. Embolization: is indicated preoperatively to control the vascularity of the tumor.
3. Radiotherapy: should be reserved for patients with inoperable intracranial extension.
Nasopharyngeal Carcinoma (NPC)
This tumor is common in South East Asia especially in China. The maximum age incidence is in the
5
th
decade and it affects males more than females. Most tumors arise from fossa of Rosenmuller.
Aetiology
The exact etiology is unknown. The factors responsible are:
1.
Genetic: The
Chinese have a higher genetic susceptibility to NPC.
2. Viral: Epstein-Barr virus is closely associated with NPC.
3. Environmental: Ingestion of salted fish and indoor cooking in homes without chimneys are
common in china.
Spread of Nasopharyngeal Carcinoma
1. Direct:
Anteriorly: Into the nasal cavity and paranasal sinuses leading to nasal symptoms.
Posteriorly: to the retropharyngeal space and lymph node of Rouviere.
Laterally: into the parapharyngeal space involving the last 4 cranial nerves.
Superiorly through the base of the skull involving the optic nerve and the cavernous sinus.
Inferiorly to the oral cavity and retrotonsillar region.
2. Lymphatic spread to the cervical lymph node,
3. Blood born (rare).
Clinical picture
1. Cervical lymphadenopathy: is often the presenting feature which may be unilateral or bilateral.
2. Nasorespiratory symptom: nasal obstruction, nasal speech and epistaxis.
3. Tinnitus and aural symptoms due to Eustachian tube obstruction. This may proceed to secondary
otitis media.

8
4. Neurological symptoms: the most frequently involved nerves are 5
th
, 6
th
, 9
th
and 10
th
cranial
nerves. The latter two nerves paralysis leads to immobility of soft palate. Involvement of the
sympathetic chain results in Horner's syndromes.
5. Pain and headache due to intracranial extensions or sphenoidal sinusitis.
Examination
Posterior rhinoscopy: a large exophytic tumor may be seen.
The palate is pushed downward and paralyzed.
The neck should be palpated for metastatic lymph nodes.
Middle ear effusion.
Parapharyngeal spread can cause trismus.
Investigation
1. Imaging:
X-ray of the base of the skull ----bony destruction involving the petrus bone, foramen lacerum
and carotid canal.
CT scan and MRI: MRI is superior to CT scan in finding soft tissue.
2. Biopsy under GA,
Treatment
Radiotherapy is the treatment of choice because surgical removal of the primary growth is
impossible.
Chemotherapy as an adjuvant to radiotherapy is of contraverse.
Surgery in form of radical neck dissection is reserved for patients where lymph nodes are not
controlled by radiation or when enlarged lymph nodes appear after the primary tumor has been
controlled.
