
1
4th stage
باطنية
Lec-10
د.ظاهر
6/12/2015
Empyema
Empyema
The presence of pus in the pleural space. Which may be thin as
serous fluid or thick and impossible to aspirate by ordinary needle.
Microscopically, neutrophil leucocytes are present in large
number.
It may involve the whole pleural space or loculated (encysted)
Empyema is almost invariably unilateral.
Empyema
Aetiology
Empyema is always secondary to infection in a neighboring structure,
usually the lung;
1-Bacterial pneumonia &tuberculosis.
2-Over 40% of patients with community-acquired pneumonia develop an
associated pleural effusion
And 15% of them develop secondary bacterial infection and empyema.
3-Infection of haemothorax,& rapture of subphrenic abscess.
4-Delay in the diagnosis and instigation of appropriate therapy.

2
Pathology
Both layers of pleura are covered with a thick, shaggy
inflammatory exudate.
The pus in the pleural space is often under considerable pressure
and if the condition is not adequately treated pus may rupture
into a bronchus causing a bronchopleural-fistula and
pyopneumothorax,
Or track through the chest wall with the formation of a
subcutaneous abscess or sinus.
Empyema can heal by eradication of the infection.
Obliteration of the empyema space and apposition of the visceral
and parietal pleural layers.
Re-expansion of the compressed lung is secured at an early stage
by removal of all the pus from the pleural space.
Factors interfere with the re-expansion of the lungs
1-The visceral pleural becomes grossly thickened and rigid due to
delayed treatment or inadequate drainage of the infected pleural fluid.
2-The pleural layers are kept apart by air entering the pleura through a
bronchopleural fistula.
3-There is underlying disease in the lung, such as bronchiectasis,
bronchial carcinoma or pulmonary tuberculosis preventing re-expansion.
3
The Stages of Empyema
Stage I - “Exudative”
sterile pleural fluid develops secondary to inflammation without fusion
of the pleura
Stage II - “Fibrinopurulent”
a fibrinous peel develops on both pleural surfaces limiting lung
expansion
Stage III - “Organizing”
in-growth of capillaries & fibroblasts into the fibrinous peel
Clinical features
Systemic features ;
1-Pyrexia,usually high and remittent
2-Rigors,sweating,malaise and weight loss
3-Polymorphonuclear leucocytosis, high (C-Reactive Protein) CRP.
Local feature ;
1-Pleural pain; breathlessness; cough and sputum usually because of
underlying lung disease; copious purulent sputum if empyema rupture
into a bronchus (bronchopleural fistula)
2-Clinical signs of fluid in the pleural space
Differential diagnosis
Pleural involvement occurs in up to 5% of patients with
rheumatoid arthritis.
Pleural malignancy
Chylothorax and pseudochylous effusion
Pulmonary embolism
Esophageal rupture
4
investigation
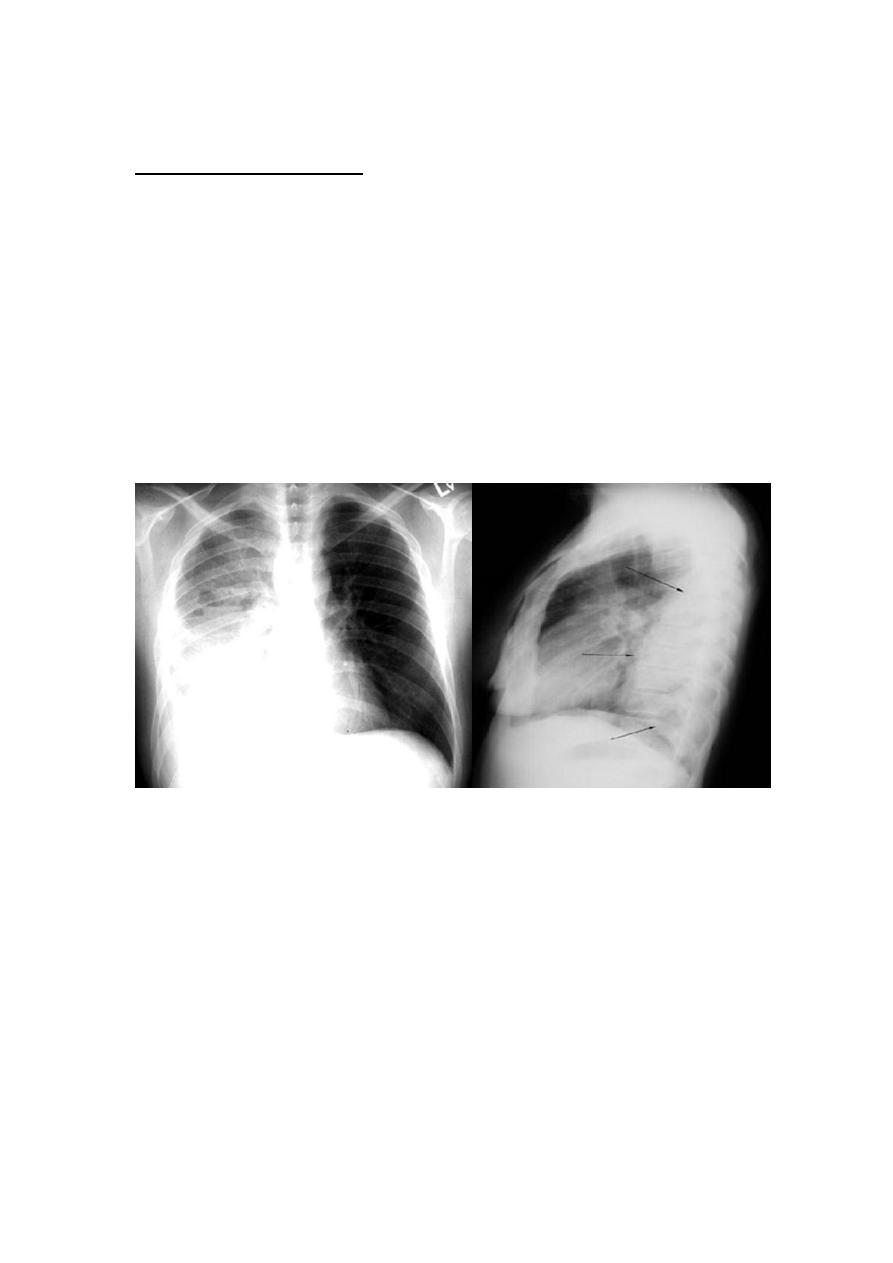
Radiological examination;
The appearance is often indistinguishable from those of pleural
effusion.
When air is present in addition to pus (pyopneumothorax).
A horizontal 'fluid level' marks the interface between the liquid and
air .
Ultrasound and CT are extremely valuable in defining the extent of
pleural thickening and location of the fluid .
And in the case of CT assessing the underlying lung parenchyma
and patency of the major bronchi.
Radiology Examination Cont..
The presence of fever, pulmonary infiltrates and fluid should
always alert clinician to the possibility of a parapneumonic
collection.
Ultrasound is good visualizing septations within loculations that
are not usually seen on CT images, but may not identify some
separate fluid loculations in inaccessible areas of the thorax.
5
Bacteriology
Aerobic organisms are the most frequent organisms identified
from infected pleural fluid.
These are most commonly Gram-positive organisms from
Streptococcal species, followed by Staphylococcus aureus.
Gram-negative empyema is more frequent in patients with
underlying diseases, especially those with diabetes and
alcoholism.
Staphylococcus aureus and Gram-negative enteric bacteria such
as Klebsiella pneumonia have a particular propensity to cause
pleural infection.
6
Bacteriological data.
Streptococcus pneumoniae: 15-20%
Increased resistance
Staphylococcus:15-30%
Streptococcus spp
Gram Negative: 20-50%
Klebsiella, Enterobacter, Pseudomonas, Hemophilus, E.Coli
Anaerobes: Fusobacterium, Bacteroides fragilis
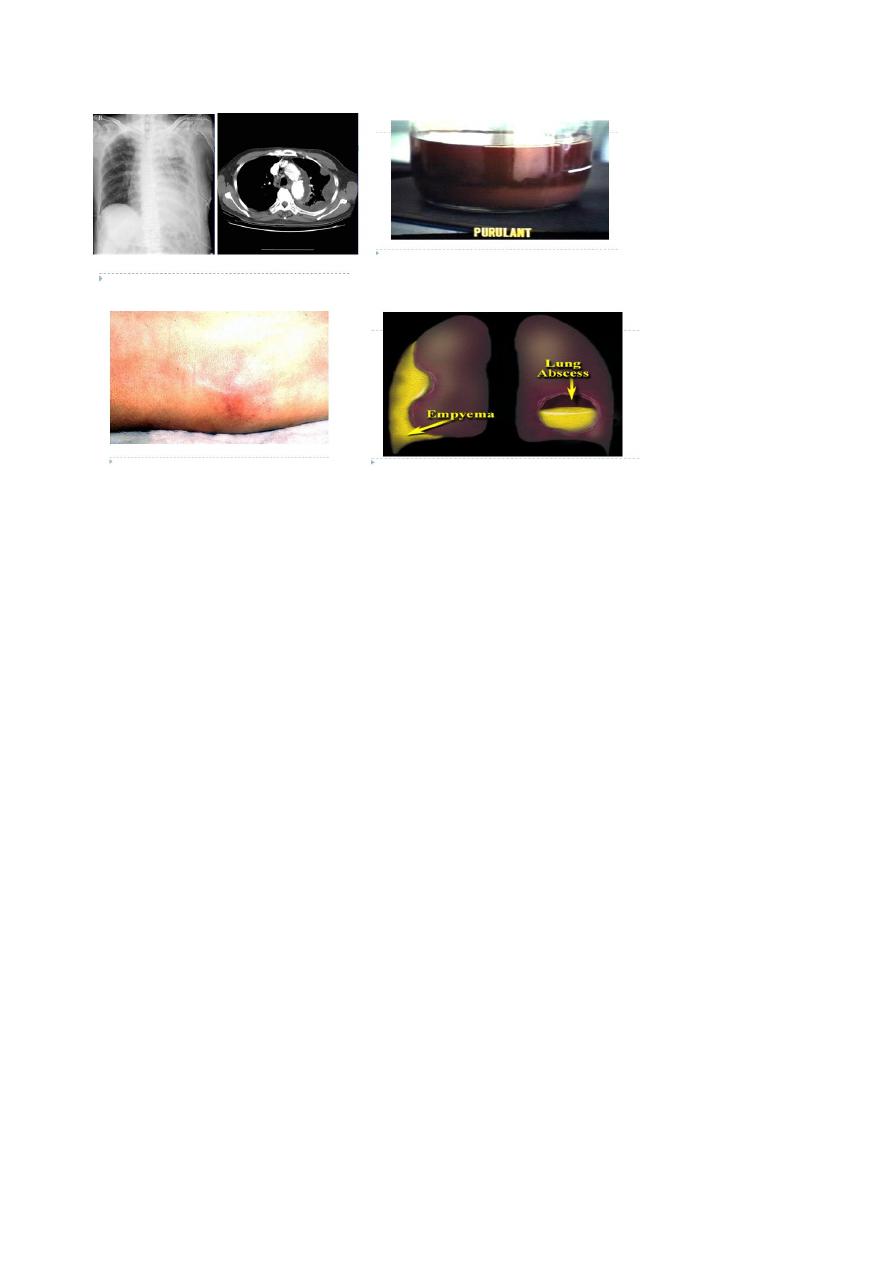
Aspiration of pus
This confirms the presence of an empyema. Ultrasound or CT is
recommended to identify the optimal place to undertake
pleuracentesis, which is best performed using a wide-bore needle.
The pus is frequently sterile when antibiotics have already been
given.
The distinction between tuberculous and non-tuberculous disease
can be difficult and often requires pleural histology and culture.
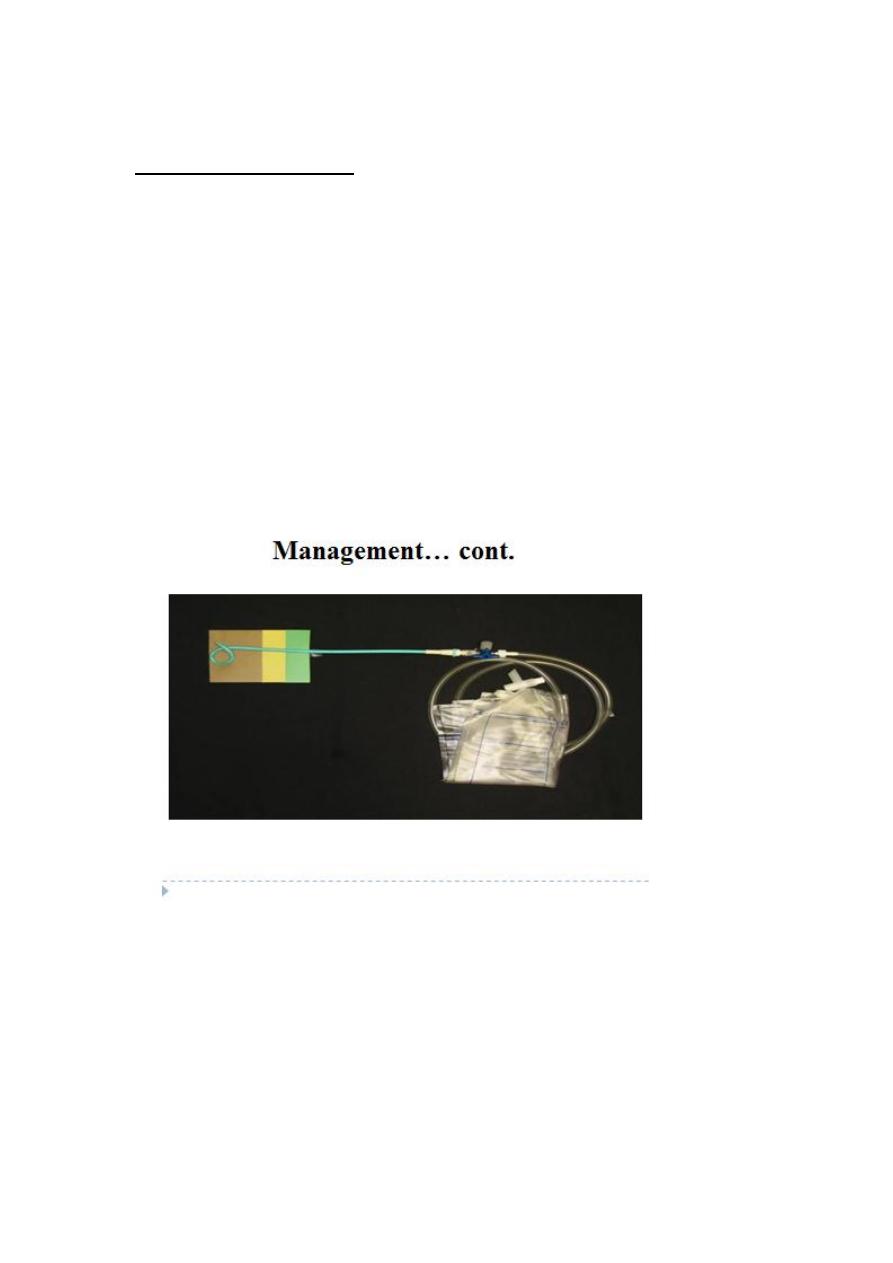
Management
Treatment of non-tuberculous empyema;
If the pus is thin an intercostal tube should be inserted under
ultrasound or CT guidance into the most dependent part of the
empyema space and connected to a water-seal drain system.
If the initial aspirate reveals turbid fluid or frank pus, or if
loculations are seen on ultrasound, the tube should be put on
suction (5-10 cm water) and flushed regularly with 20 ml normal
saline.
7
Chest catheter drainage
Optimal size of catheter?
Excellent outcomes may be achieved with such small catheter
especially when combined with fibrinolytic therapy.
Drainage may fail if the fluid is of high viscosity and direct blocks
the tube.
The balance of forces drawing it down the tube is inadequate.
If the fluid is partitioned by fibrinous septae.
The rapidity of chest tube drainage might be improved by
increasing the drain size, but the successful drainage is
unchanged.
Here again, provide that the catheter is patent, its bore is
irrelevant.

8
Intrapleural fibrinolytics
1949 Tillet and Sherry: partial purified streptococcal fibrinolysin
Highly purified streptokinase: 250000IU
Urokinase: 100000IU
It form a complex with plasminogen that converts additional
circulating plasminogen to plasmin. Plasmin lyses fresh fibrin clot
and digests prothrobin and fibrinogen.
Improvement in the chest radiograph and greater volume pleural
drainage, not outcome of mortality, surgical frequency, or hospital
stay.
Tube drainage with streptokinase and early surgical intervention
showed reduced length of hospitalization
Potential side effect: hemorrhage, pleuritic pain and fever
Management… cont.
Thoracocentesis and pleural fluid analysis help in deciding therapy
.
Streptokinase and Urokinase can be used in multiloculated
empyema.
Video assisted thoracoscopic surgery or thoracoscopy with
debridement are equally effective for multi-loculated empyema.
Cases not responding to above measures need decortication
Management cont….
Antibiotic directed against the organism causing the empyema
should be given for 2-4 weeks.
An empyema can often be aborted if the previously mentioned
measures are started early.
If the intercostal tube is not providing adequate drainage (when
the pus is thick or loculated) surgical intervention is required .
Surgical 'decortications' of the lung If gross thickening of the
visceral pleura has developed and is preventing re-expansion of
the lung.

9
Antibiotic treatment
As soon as the bacteriologic sample are recovered
Pneumonia
Amoxicillin, 3GC or 3GC +/- Metronidazole
Amox-clavulanic acid
Dosage of the molecule
Nosocomial
Tazobactam or Imipenem
+/- Aminoglycoside or Quinolone
Not Pneumococcus directed molecules
Adapted to the laboratory results
Treatment of tuberculous empyema
Antituberculosis chemotherapy must be started immediately
The pus in the pleural space aspirated through a wide-bore needle
until it ceases to re-accumulate .
Intercostal tube drainage is often required.
In many patients required to ablate a residual empyema space.
Surgery for pleural infecetion
No definite data that define the point at which a patient with
empyema should proceed to surgical intervention.
Open thoracotomy with decortication
Mini-thoracotomy
Video-assisted thoracoscopic surgery (VATS)
Rib resection with open drainage
VATS: reduced hospital inpatient time, postoperative
complications and length of operating time
VATS: failures are with empyema in the organizing stage of the
disease
