Maternal Health Care
Cont.Specific objectives
At the end of this lecture, you will be able to:Identify high risk pregnancy
Define focused antenatal care
Differentiated between traditional and focused antenatal care
Enumerate important effect of poor nutrition during pregnancy
Define intranatal and post natal care
During ANC visits pregnant women intended to be classified as
Low risk orHigh risk
based on predetermined criteria
High risk approach
Maternal age
• Primi < 16 yrs• Primi > = 30 years
• Multi >35 years
Weight
Less than 45 kgs
more than 90 kgs
Height
<150 cmHigh risk approach
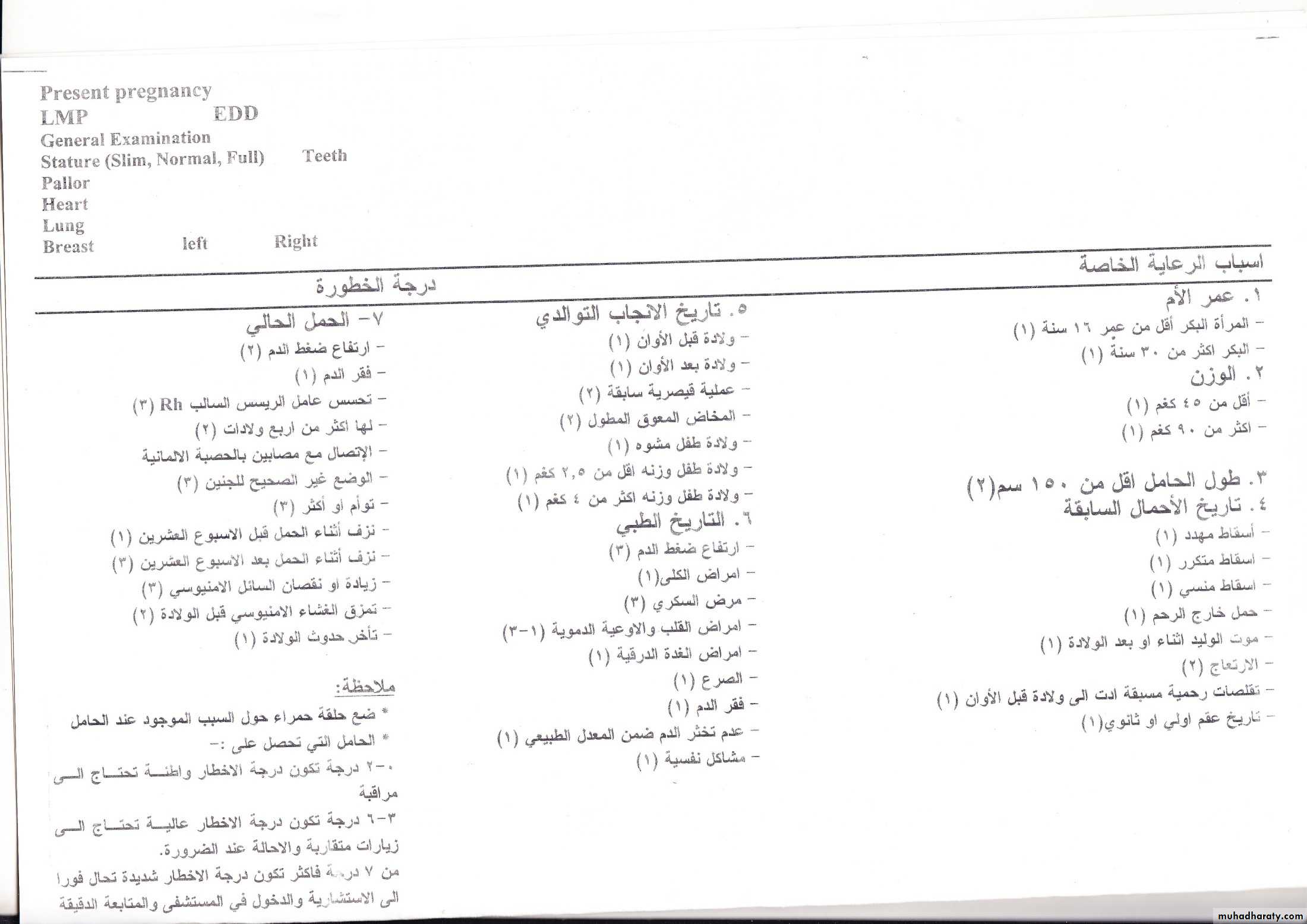
Criteria of high risk approachPresent obstetrical History
HDPAnemia
Rh isosensetiation
High parity (>4)
Too short or too long spacing
Abnormal fetal presentation
APH
Twins
Minimum or no weight gainIntra uterine growth retardation
Post-term pregnancy
Smoker mother
High risk approach
Previous obstetric history
Threatened abortion
Habitual abortion
Missed abortion
More than 2 abortions
Stillbirth
HDP
Prematurity
High risk approach
Previous delivery history
Premature labourPost mature labour
Previous Cs
Previous obstructed labour
Fetal abnormality
Medical history
Hypertension, renal diseases, DM, CVD, Thyroid disease, epilepsy.High risk approach
FOCUSED ANTENATAL CARE
• The routine ANC (discussed previously) assumes that frequent visits and classifying pregnant women into low and high risk by predicting the complications ahead of time, is the best way to care for the mother and the fetus.• This traditional approach was replaced by focused antenatal care (FANC) — a goal-oriented antenatal care approach, which was recommended by researchers in 2001 and adopted by the World Health Organization (WHO) in 2002. FANC is the accepted policy in Ethiopia.
• .
FANC
Focused or goal oriented ANC services provide specific evidence-based interventions for all women, carried out at certain critical times in the pregnancy
Principles of Focused ANC
• Thorough evaluation of the pregnant woman to identify and treat existing obstetric and medical problems.• Administer prophylaxis as indicated, e.g. preventive measures for malaria, anaemia, nutritional deficiencies, sexually transmitted infections, including prevention of mother to child transmission of HIV (PMTCT, see Study Session 16), and tetanus.
FANC
3. With the mother, they decide on where to have the follow-up antenatal visits, how frequent the visits should be, where to give birth and whom to be involved in the pregnancy and postpartum care.4. Provided that quality of care is given much emphasis during each visit, and couples are aware of the possible pregnancy risks, the majority of pregnancies progress without complication.
5. No pregnancy is labelled as ‘risk-free’ till proved otherwise, because most pregnancy-related fatal and non-fatal complications are unpredictable and late pregnancy phenomena.
FANC
How many visits
A recent multi-country randomized control trial led by the WHO (17) and a systematic review showed that essential interventions can be provided overfour visits at specified intervals, at least for healthy women with no underlying medical problems.
• First visit: On confirmation of pregnancy
• Second visit: 20-28 weeks
• Third visit: 34-36 weeks
• Fourth visit: before expected date of delivery
OR when the pregnant woman feels she needs to consult health worker
Focused ANC Program Activities
VisitFirst Visit
Second visit
Third visit
Fourth visit
Gestational age
<16 weeks
28 weeks
32 weeks
38 weeks
Activities
Classification to either the basic or specialized component
Clinical exam
Hgb test
Gestational age determination
Blood pressure
Weight/Height
Syphilis/STIs
Urinalysis
ABO/RH
TT administration
Iron supplementation
Document on ANC card
Clinical exam for anemia
Gestational age; FH; FHB exam
Blood pressure
Weight- only if underweight at initial visit
Urinalysis- for nullipara or previous preeclampsia
Iron supplement
Complete on ANC card
Hgb test
TT second dose
Instructions for birth planned
Recommendations for lactation/contraception
Document on ANC card
Examine for breech presentation
Document on ANC card
Focused antenatal care
Traditional antenatal care
Characteristics
4 for women categorized in the basic component
16–18 regardless of risk status
Number of visits
Integrated with PMTCT of HIV, counselling on danger symptoms, risk of substance use, HIV testing, malaria prevention, nutrition, vaccination, etc.
Vertical: only pregnancy issues are addressed by health providers
Approach
Assumes all pregnancies are potentially ‘at risk’. Targeted and individualized visits help to detect problems
More frequent visits for all and categorizing into high/low risk helps to detect problems. Assumes that the more the number of visits, the better the outcomes
Assumption
Does not rely on routine risk indicators. Assumes that risks to the mother and fetus will be identified in due course
Relies on routine risk indicators, such as maternal height <150 cm, weight <50 kg, leg edema, malpresentations before 36 weeks, etc.
Use of risk indicators
Shared responsibility for complication readiness and birth preparedness
To be solely dependent on health service providers
Prepares the family
Two-way communication (counselling) with pregnant women and their husbands
ne-way communication (health education) with pregnant women only
• Communication
Less costly and more time efficient. Since majority of pregnancies progress smoothly, very few need frequent visits and referral
Incurs much cost and time to the pregnant women and health service providers, because this approach is not selective
Cost and time
Alerts health service providers and family in all pregnancies for potential complications which may occur at any time
Opens room for ignorance by the health service provider and by the family in those not labelled 'at risk', and makes the family unaware and reluctant when complications occur
Implication
Weight Gain During Pregnancy
Healthy pregnant women gain 10-12 kgs.
Undernourished women will gain <7 kgs.
Gain in weight of <6 kgs indicates high risk.
Nutrition during pregnancy
• Outcomes of Maternal Malnutrition• LBW & Prematurity
• Fetal & neonatal Mortality & Morbidity
• Increased chance of death in neonatal period
• congenital Malformations
Diet:
-Daily requirement in pregnancy about 2500 calories.- Women should be advised to eat more vegetables, fruits, proteins, and vitamins and to minimize their intake of fats.
Purpose:
*Growing fetus.
*Maintain mother health.
*Physical strength & vitality in labor.
*Successful lactation.
Objectives:
Thorough Asepsis (“The Five Cleans” - clean hands, surface, blade, cord, tie)Minimum injury to mother and newborn.
Preparedness to deal with complications.
(prolonged labor – ante partum hemorrhage convulsions malpresentation….etc.)
Care of baby at delivery.
Determination of place of birth, with a well-organized back up system.
Intra-natal Care
Postnatal CareCare of mother after delivery (puerperium begins after the placenta is expelled and lasts for 6 weeks).
Its components are:
Postpartum examination
Medical care
Follow up
Health education
Family planning services
Psychological and social support
Objectives
• Restoration of mother to optimum health
• To prevent complications of puerperium
• Provide basic postpartum care and services to mother and child
• Motivate, educate and provide family planning services
• To check adequacy of breast feeding