
1
Fifth stage
Pediatrics
Lec-3
د.بسام
30/11/2015
BIRTH ASPHYXIA
Birth asphyxia or hypoxia- ischemia:
It refers to a signs & symptoms of hypoxia which means poor oxygen delivery to body
organs that is induced by:-
* hypoxemia: which refers to an arterial oxygen concentration of less than normal.
and if hypoxia is prolonged, cardiac and vascular compromise occur result in hypotension
causing:
ischemia: which refers to a blood flow to cells or an organ that is insufficient to maintain
their normal function which will result in more tissue hypoxia.
Eventually:
*Tissue anoxia occur which is a term used to indicate the consequences of complete lack
of oxygen.
After an episode of hypoxia and, anaerobic metabolism occurs and generates increased
amounts of lactate and inorganic phosphates.
Excitatory and toxic amino acids, particularly glutamate, accumulate in the damaged tissue.
Increased amounts of intracellular sodium and calcium may result in tissue swelling and
cerebral edema. There is also increased production of free radicals and nitric oxide in these
tissues.

2
Etiology:
Hypoxia-ischemia can occur before, during or after delivery:-
Intrauterine (before delivery) asphyxia:
here there is no sufficient gas exchange in the fetus through the placenta, occur in the
following conditions:-
- interuption of the umbilical circulation as in cord prolapse.
- poor perfusion of the maternal side of the placenta as in maternal hypotension, pre
eclampsia, abruptio placentae.
- impaired maternal oxygenation as in asthma,pulmonary embolism or pneumonia.
- impaired fetal oxygenation or perfusion as in fetomaternal hemorrhage or fetal
thrombosis.
Causes of asphyxia during delivery:-
- premature placental separation.
- inadequate relaxation of the uterus to permit placental filling as a result of uterine tetany
caused by excessive use of oxytocine during labor.
- impedence of the circulation of blood through the umbilical cord as a result of
compression or knotting of the cord.
Causes of asphyxia after birth:-
- anemia severe enough to lower the oxygen content of the blood to a critical level due to
severe hemorrhage or hemolysis.
- shock severe enough to interfere with the transport of oxygen to vital cells as in adrenal
hemorrhage,IVH, overwhelming infection, or massive blood loss.
- a deficit in arterial oxygen saturation resulting from failure to breathe adequately
postnatally due to a cerebral defect, maternal medication narcosis, or injury or due to
neuromuscular disease as myasthenia gravis or myopathy.
-failure of oxygenation of an adequate amount of blood resulting from severe forms of
cyanotic congenital heart disease or deficient pulmonary function as hyaline membrane
disease, neonatal pneumonia, meconium aspiration, pneumothorax, diaphragmatic hernia,
pulmonary hypoplasia, or pleural effusion.
3
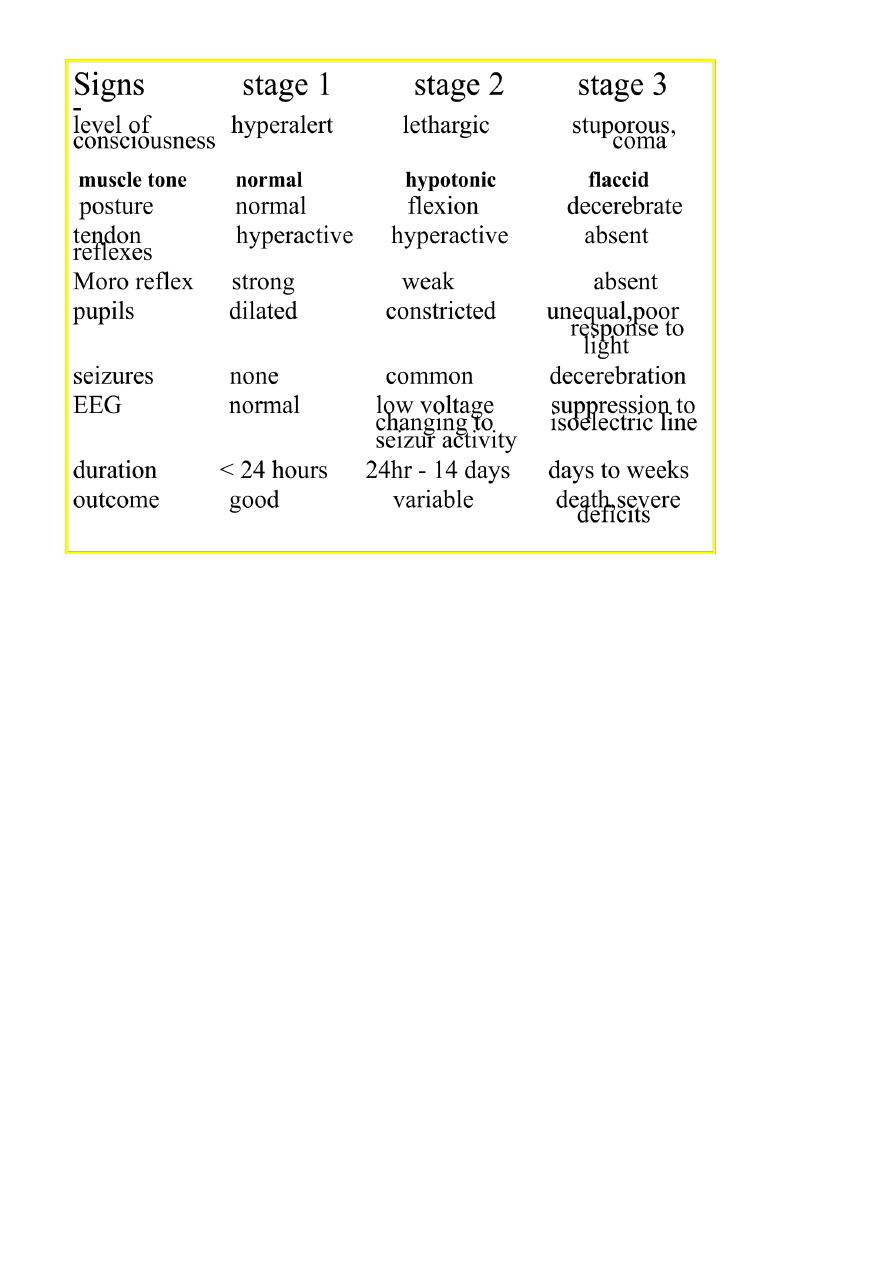
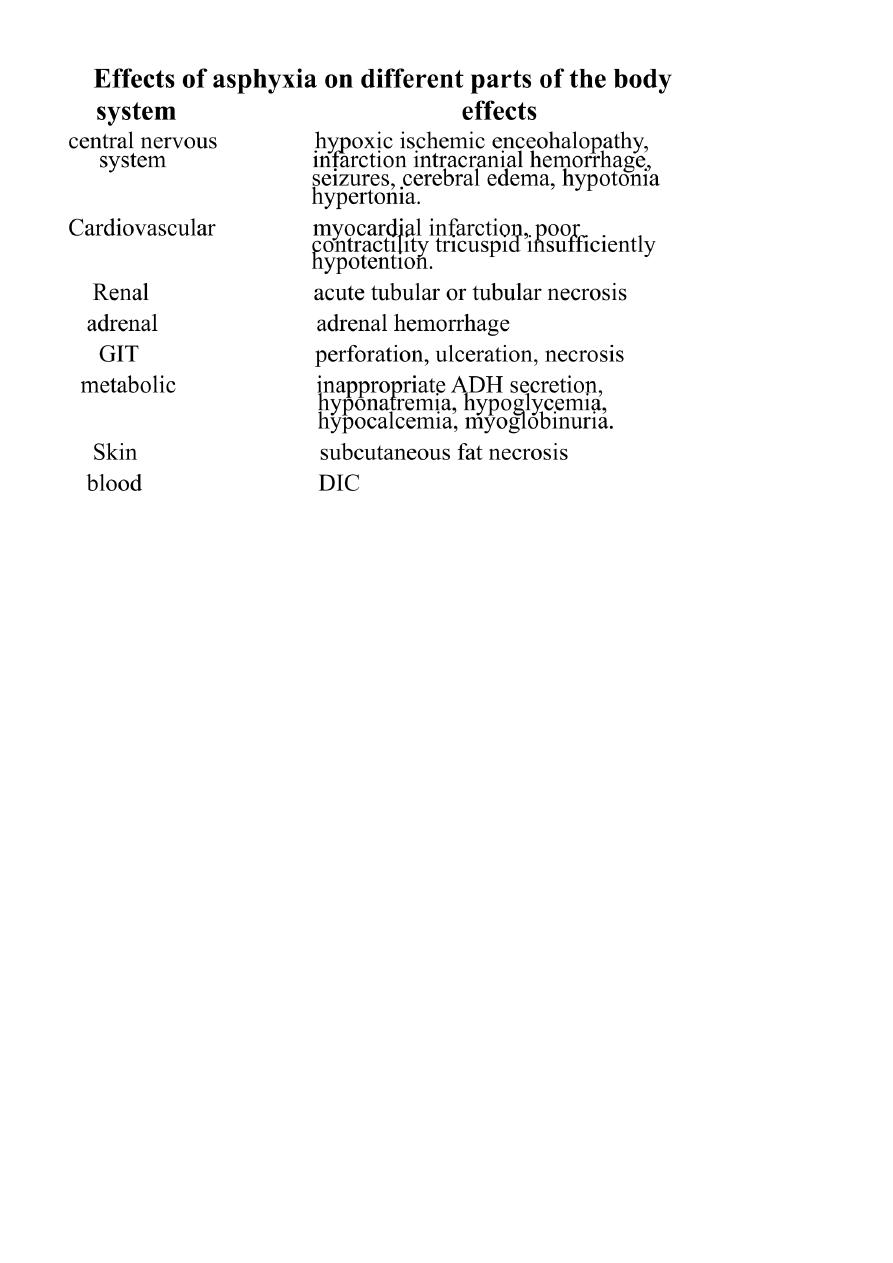
Clinical manifestations:-
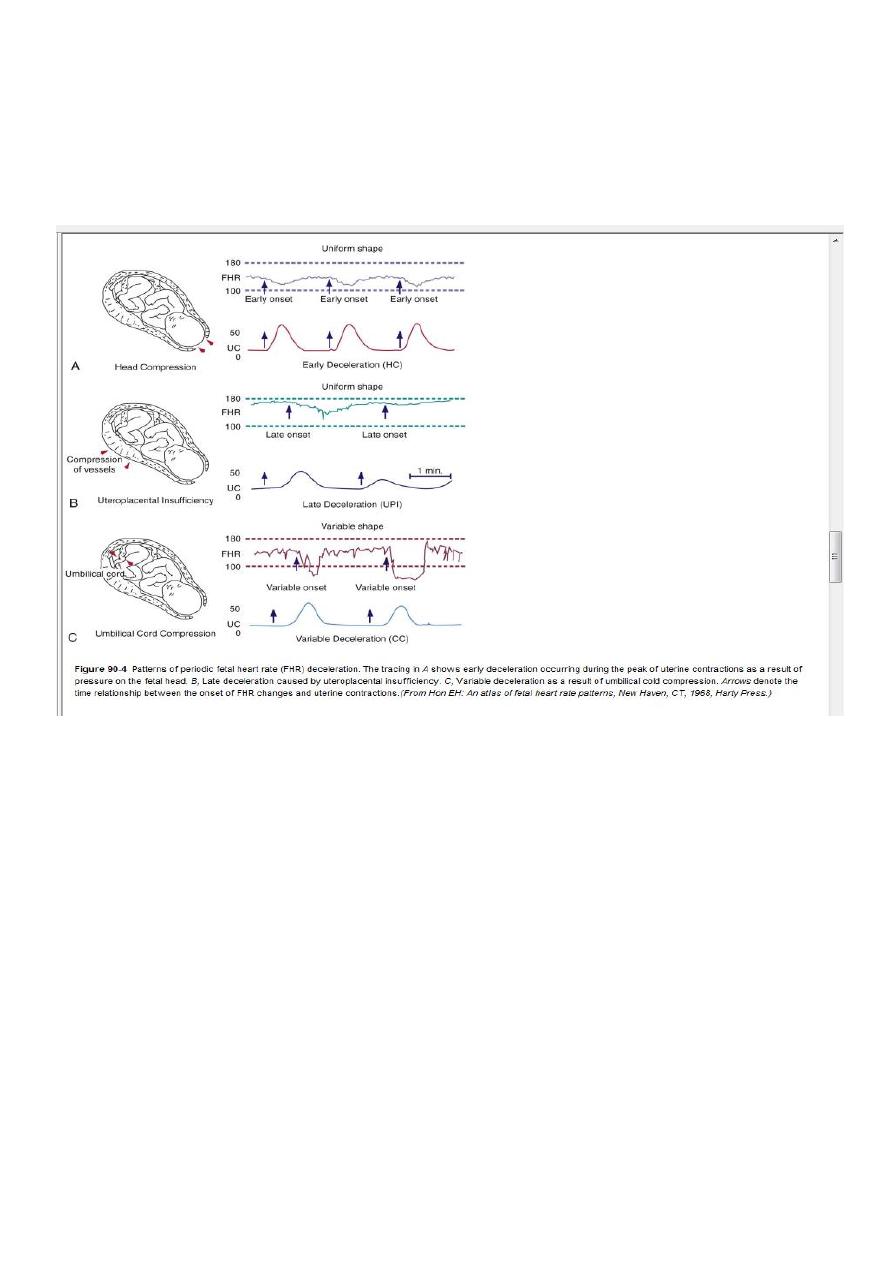
Intrauterine growth restriction with increased vascular resistance may be the 1st indication
of fetal hypoxia. During labor, the fetal heart rate slows. Continuous heart rate recording
may reveal a variable or late deceleration pattern particularly in infants near term.
These signs should lead to the administration of high concentrations of oxygen to the
mother and consideration of immediate delivery to avoid fetal death and CNS damage.
At delivery, the presence of meconium-stained amniotic fluid is evidence that fetal distress
has occurred. At birth, affected infants may be depressed and may fail to breathe
spontaneously. During the ensuing hours, they may remain hypotonic or change from a
hypotonic to a hypertonic state, or their tone may appear normal.
Pallor, cyanosis, apnea, a slow heart rate, and unresponsiveness to stimulation are also
signs of HIE. Cerebral edema may develop during the next 24 hr and result in profound
brainstem depression. During this time, seizure activity may occur; it may be severe and
refractory to the usual doses of anticonvulsants. Though most often a result of the HIE,
seizures in asphyxiated newborns may also be due to hypocalcemia, hypoglycemia, or
infection.
4
Treatment:-
Selective cerebral or whole body (systemic) therapeutic hypothermia reduces mortality or
major neurodevelopmental impairment in term and near-term infants with HIE.
Hypothermia decreases the rate of apoptosis and suppresses production of mediators
known to be neurotoxic, including extracellular glutamate, free radicals, nitric oxide, and
lactate.
Additional therapy for infants with HIE includes supportive care directed at management of
organ system dysfunction. Hyperthermia has been found to be associated with impaired
neurodevelopment, so it is important to prevent hyperthermia before initiation of
hypothermia. Careful attention to ventilatory status and adequate oxygenation, blood
pressure, hemodynamic status, acid-base balance, and possible infection is important.
5
