Revision from the previous lecture:
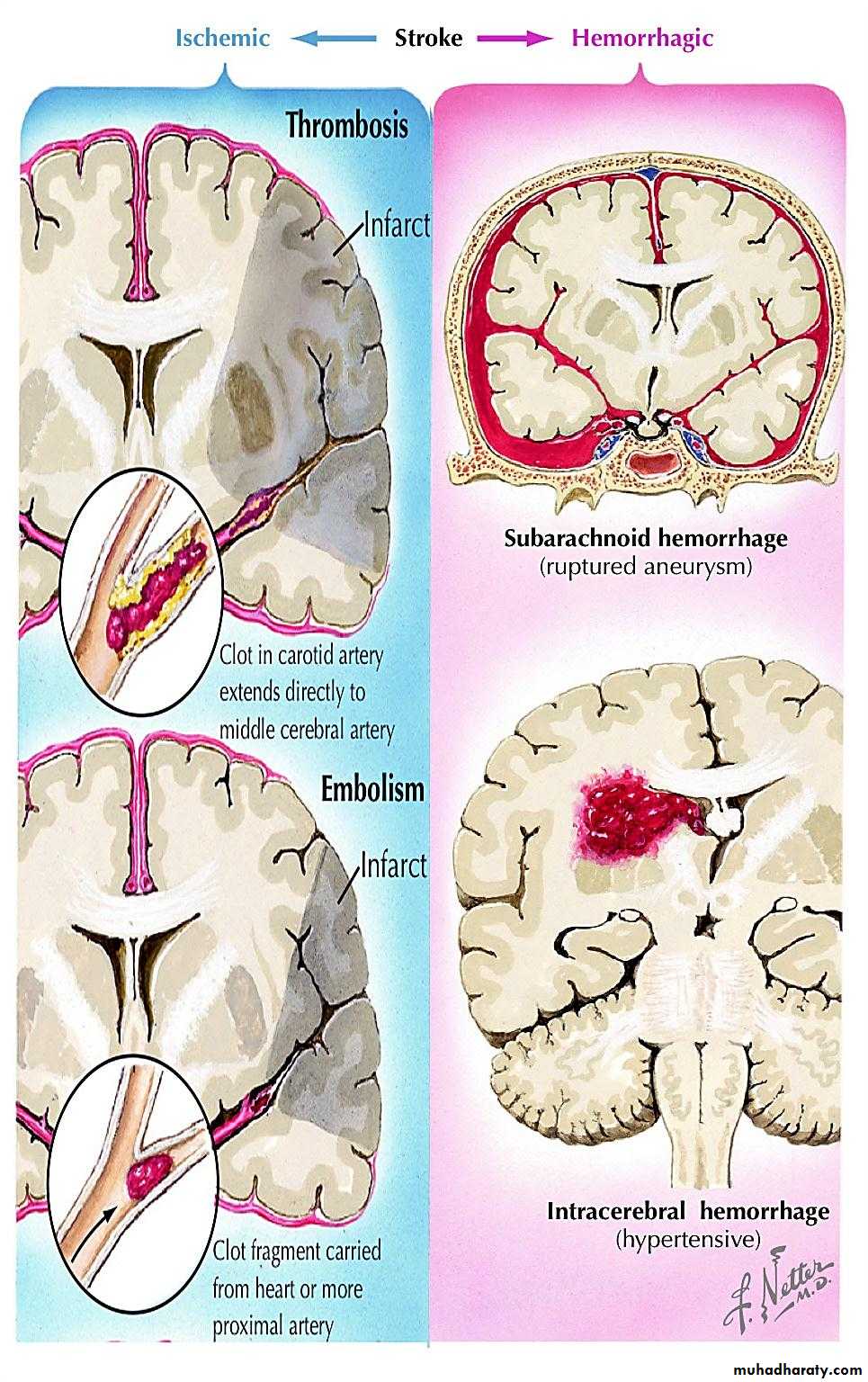
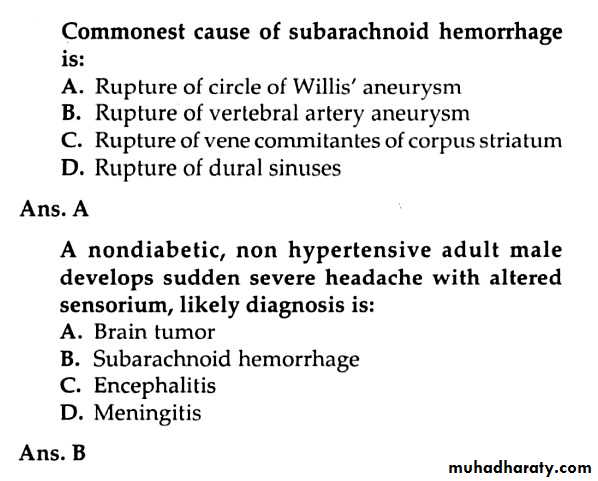
Note: The below revision were added by the students (its not included in lecture):The previous lecture discussed the ischemic type of stroke, while in this lecture we will complete the other type (hemorrhagic) which represents %15 of all stroke and is subdivided according to location into intracerebral haemorrhage and subarachnoid haemorrhage.
The new lecture
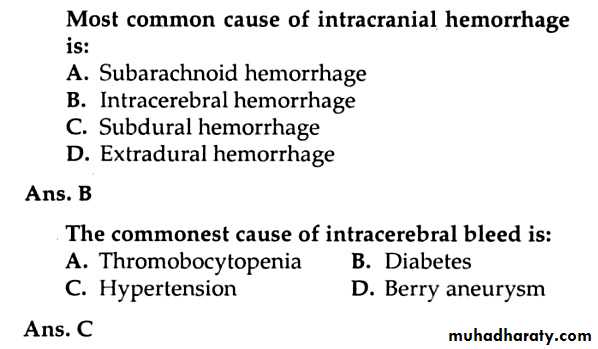
Intracranial HemorrhageIntracerebral haemorrhage
Intracerebral haemorrhage causes about 10% of acute stroke. It usually results from rupture of a blood vessel within the brain parenchyma.
Causes of intracerebral haemorrhage and associated risk factors:
Complex small-vessel disease with disruption of vessel wall (Age Hypertension, High cholesterol)
Amyloid angiopathy (Familial, Age)
Impaired blood clotting(Anticoagulant therapy, Blood dyscrasia, thrombolytic therapy)
Vascular anomaly (Arteriovenous malformation)
Substance misuse (Alcohol, Amphetamines, Cocaine)
Spontaneous ICH results from intracerebral arterial rupture, particularly perforating vessels. The haematoma expands following the path of least resistance, usually along white matter tracts, and occasionally into the ventricular system.
Neurological deficit results both from direct tissue destruction and indirectly from local compression and mass effect, usually in proportion to both the volume of haematoma and its rate of expansion.
Hypertensive hemorrhage occurs without warning, most commonly while the patient is awake. Headache is present in 50% of patients and may be severe; vomiting is common. Blood pressure is elevated after the hemorrhage has occurred. Thus, normal or low blood pressure in a patient with stroke makes the diagnosis of hypertensive hemorrhage unlikely, nerveless, it is wrong to believe that patients with less severe stroke syndromes can be diagnosed on clinical grounds to have had ischaemic strokes.
Clinical features vary with the site of hemorrhage:
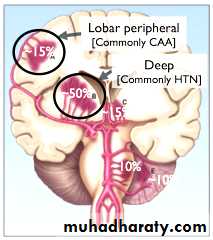
Deep cerebral hemorrhage (putamen & thalamus): produces a contralateral sensorimotor deficit.
Lobar hemorrhage: the frontal, parietal, temporal, and occipital lobes. Symptoms and signs vary according to the location.
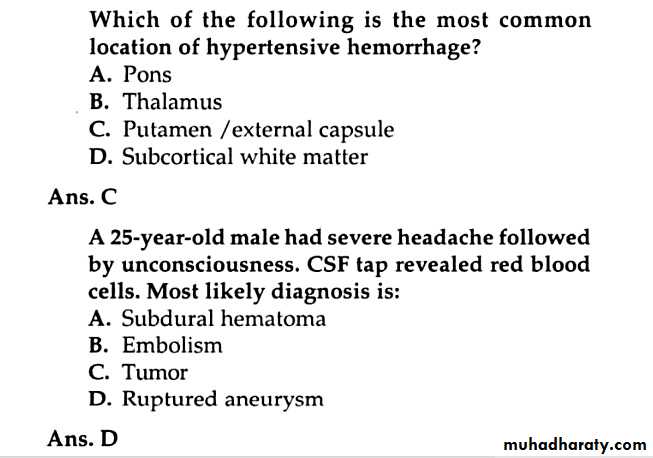
Pontine hemorrhage: With bleeding into the pons, coma occurs within seconds to minutes and usually leads to death within 48 hours. Ocular findings typically include pinpoint pupils. Horizontal eye movements are impaired.
Cerebellar hemorrhage: The distinctive symptoms of cerebellar hemorrhage (headache, dizziness, vomiting, and the inability to stand or walk) begin suddenly, within minutes after onset of bleeding. Although patients may initially be alert or only mildly confused
Management of ICH
A- Investigations:CT /MRI the best to detect heamoorage is brain CT
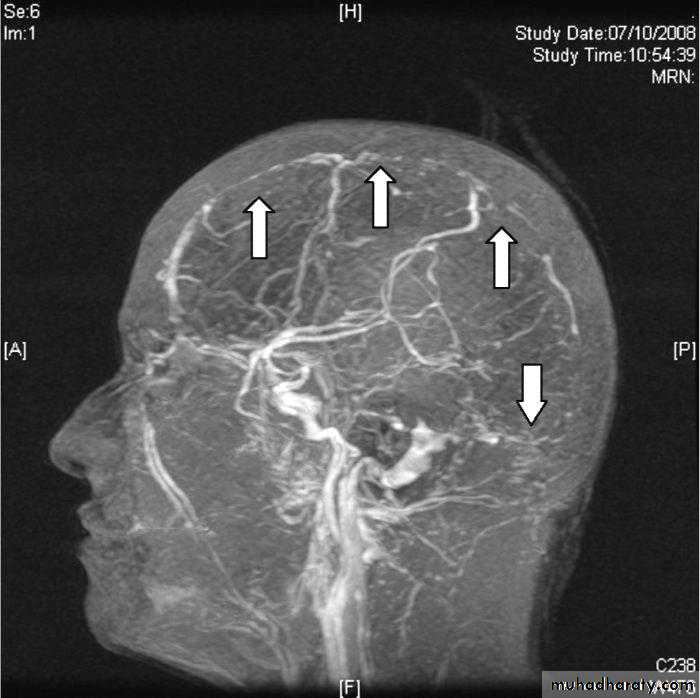
CT angiograph or MRA (magnetic resonance angiography) in case of AVM (arteriovenous malformation) suspension.
CBC, PT , PTT and INR for bleeding tendency
RBS and electrolyte measurement.
B-Treatment:
Surgical measures: Cerebellar decompression if patient deteriorating neurologically or have or brain stem compression, is most important therapeutic intervention in hypertensive hemorrhage is surgical decompression for cerebellar hematomas. Unless this step is taken promptly, there may be a fatal outcome or unexpected deterioration. Note that this procedure may also reverse the neurologic deficit.
Medical measures
Anticoagulant and antithrombotic medications should be discontinued in the setting of acute intracerebral hemorrhage, and any coagulopathy should be reversed by administering fresh-frozen plasma and vitamin K.
The use of antihypertensive agents, BP should be controlled in all patient, when SBP between 150 and 220 acute lowering of SBP to 140 mmhg is safe.
Antiedema agents if significant odema present such as use of mannitol.
SUBARACHNOID HEMORRHAGE
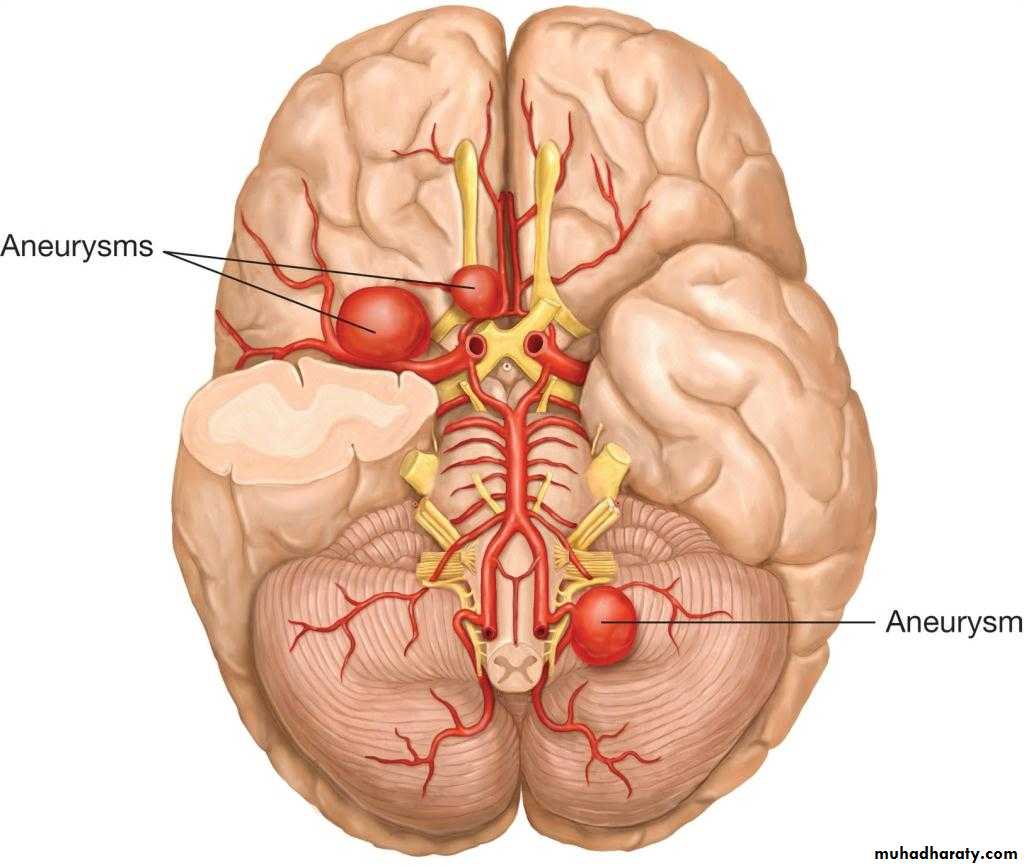
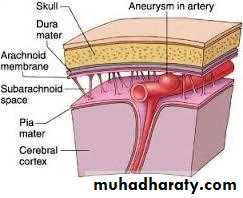
Spontaneous (nontraumatic) subarachnoid hemorrhage (bleeding into the subarachnoid space) is usually the result of a ruptured cerebral arterial aneurysm or an AVM. Rupture of a berry aneurysm accounts for approximately 75% of cases. Rupture occurs most often during the fifth and sixth decades, with an approximately equal sex distribution. The risk of rupture of an intracranial aneurysm varies with patient's age, and aneurysm site and size.Hypertension has not been conclusively demonstrated to predispose to the formation of aneurysms, but acute elevation of blood pressure (e.g., at orgasm) may be responsible for rupture of aneurysms. Intracranial AVMs, a less frequent cause of subarachnoid hemorrhage (10%), occur twice as often in men and usually bleed in the second to fourth decades.
Pathology
Cerebral artery aneurysms are most commonly congenital “berry” aneurysms, which result from developmental weakness of the vessel wall, especially at sites of branching. These aneurysmal dilatations arise from intracranial arteries about the circle of Willis at the base of the brain, other congenital abnormalities, including polycystic kidney disease and coarctation of the aorta, may be associated with berry aneurysms. AVMs consist of abnormal vascular communications.
Clinical Findings
The classic (but not invariable) presentation of subarachnoid hemorrhage is the sudden onset of an unusually severe generalized headache (“the worst headache I ever had in my life”). The absence of headache essentially precludes the diagnosis. A third of patient present with headache alone. In the remainder, loss of consciousness at onset is frequent, as are vomiting and neck stiffness. Symptoms may begin at any time of day and during either rest or exertion.Investigation
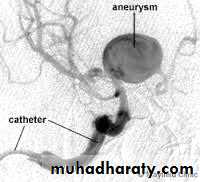
Computed tomography (CT) scan: will detect subarachnoid blood in more than 90% of patientsCSF examination may be needed if CT is negative which will reveled grossly bloody or the supernatant of the centrifuged CSF becomes yellow-tinged (xanthochromic) within several hours (certainly by 12 hours) following the hemorrhage
Four-vessel cerebral arteriography, CT angiography and magnetic resonance angiography may be used to detect aneurysm and AVM.
Complications & Sequelae:
RECURRENCE OF HEMORRHAGEARTERIAL VASOSPASM
ACUTE OR SUBACUTE HYDROCEPHALUS
SEIZURES
Syndrome of Inappropriate antidiuretic hormone secretion (SIADH) and resultant diabetes insipidus can occur.
MEDICAL TREATMENT:
Preventing elevation of arterial pressure that might re-rupture the aneurysm or AVM.
Absolute bed rest, mild sedation, and analgesics for headache Drugs impairing platelet function (e.g., aspirin) or anticoagulation should be avoided.
Intravenous fluids should be administered with care, since over hydration can exacerbate cerebral swelling. Intravenous fluids should be isotonic to minimize free water exacerbating brain edema. Normal saline can be given in amounts sufficient to ensure normovolemia. Hyponatremia is frequently seen, serum sodium should be monitor daily .treat hyponatremia.
Prophylactic use of the calcium channel antagonist drug nimodipine, 60 mg orally every 4 hours for 21 days, may reduce the ischemic sequelae of cerebral vasospasm.
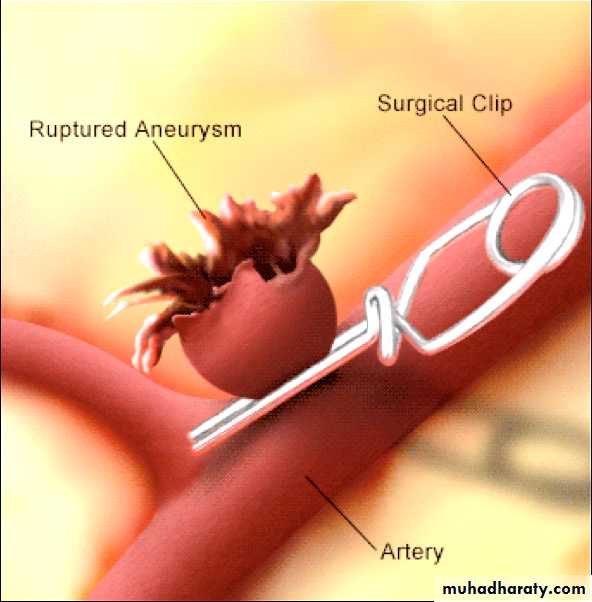
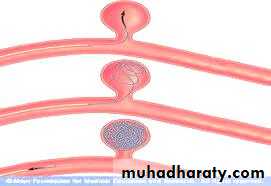
SURGICAL TREATMENT: ruptured aneurysm consists of clipping the neck of the aneurysm or the endovascular placement of a coil to induce clotting.
AVMs—Surgically accessible AVMs may be removed by en bloc resection or obliterated by ligation of feeding vessels or embolization via local intra-arterial catheter.
Coiling Clipping
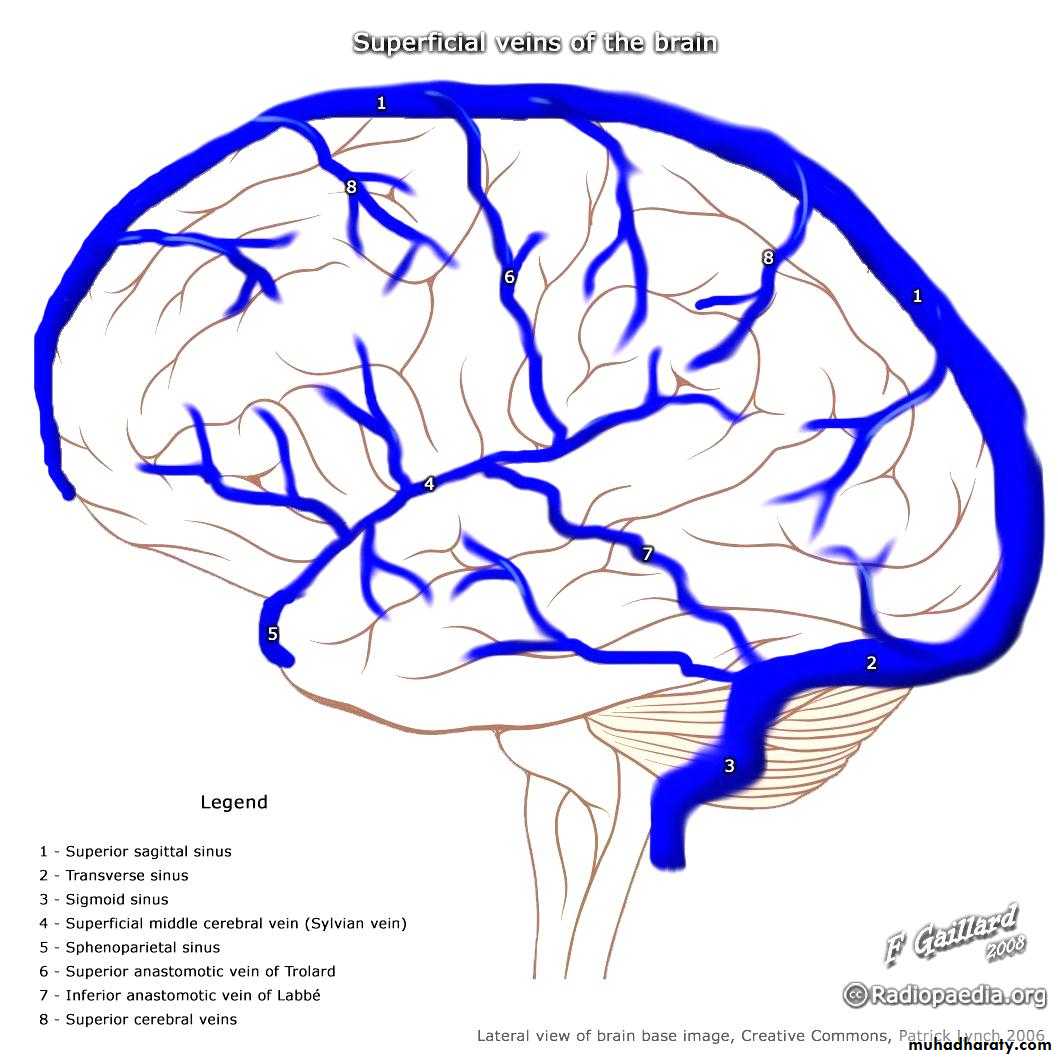
CEREBRAL VENOUS DISEASE:
Thrombosis of the cerebral veins and venous sinuses (cerebral venous thrombosis) is much less common than arterial thrombosis.Cerebral venous sinus thrombosis usually presents with symptoms of raised intracranial pressure such as headache and papilledema, also seizures, focal neurological symptoms and sometime coma. The clinical features vary according to the sinus involved
Common causes of cerebral venous thrombosis
Dehydration
Thrombophilia
Pregnancy
Oral contraceptive use
Investigations
MR venography demonstrates a filling defect in the affected vessel.Treatment:
Anticoagulation, initially with heparin followed by warfarin, is usually beneficial
END
Note: the below appendix were added by the students (its not included in lecture):
Case 1:
A 67 -year-old male presents to the emergency department with severe dizziness and the inability to walk. He complains of repetitive vomiting and occipital headache. The symptoms started two hours ago when he was playing golf in sunny weather with his friends. His past medical history is significant for hypertension and diabetes. He underwent coronary stenting two years ago for recurrent chest pain. His current medications are aspirin. Glipizide. Enalapril and metoprolol. His blood pressure is 210/110 mmHg. Heart rate is 78/min. temperature is 37 .8• C (100• F). And respirations are 18/min. Muscle strength is preserved in all four extremities. And there are no sensory abnormalities. Which of the following is the most likely cause of this patient's symptoms?Heat stroke C. Vestibular neuronitis
Posterior cerebral artery occlusion D. Cerebellar hemorrhage
Explanation:
The clinical features described in the vignette are consistent with cerebellar hemorrhage. This condition generally evolves over a few hours. Patients typically have an acute onset occipital headache. Repeated vomiting and gait ataxia. A small hemorrhage may not manifest with any other neurological deficit. A larger hemorrhage may manifest with 6th nerve paralysis. Conjugate deviation. And blepharospasm. Fever is common with any type of intracranial hemorrhage. Patients with large hemorrhages often become stuporous in a few hours. Immediate evacuation of the hematoma is required and life-saving for these patients. Neurological recovery in patients who survive is usually near complete.
So the answer is D
Case 2:
A 60-year-old female is brought to the emergency department due to a sudden onset of worsening left-sided hemiplegia, which was followed by a headache and altered mental status. She was taking her regular morning walk when she developed these symptoms. Her past medical history is remarkable for uncontrolled essential hypertension. She has been a chronic smoker for the last 30 years. The neurological examination shows muscle weakness on the left side, and deviation of eyes towards the right side. The CT scan is consistent with a hemorrhagic stroke which of the following is the most likely diagnosis?
Putamen hemorrhage C. Cerebellar hemorrhage
Pontine hemorrhage D. Subarachnoid hemorrhage
Explanation:
The above patient most likely has an intraparenchymal brain hemorrhage. Hypertension is the most important risk factor for this entity. Focal neurological signs suddenly develop and gradually worsen over minutes or hours. The onset of symptoms is not abrupt as in subarachnoid hemorrhage or embolic stroke. Symptoms usually start during normal activity or may be precipitated by sex or strenuous activity. As the hemorrhage expands, headache, vomiting and altered mental status develop.
The most common site of hypertensive hemorrhage is the putamen (35%). The internal capsule that lies adjacent to the putamen is almost always involved, thereby leading to hemiparesis. The other neurological signs include hemi-sensory loss, homonymous hemianopsia, stupor and coma. The eyes are deviated away from the paralytic side.
So the answer is A