University of Al Qadisiyah
College of PharmacyDr. Bassim I Mohammad,
MBChB, MSc, Ph.D
Low Efficacy Diuretics
Potassium sparing diureticsCarbonic anhydrase inhibitors
Osmotic diuretics
Miscellaneous
Potassium sparing diuretics
Aldosterone antagonistsSpironolactone
Eplerenone
Renal epithelial Na+ channel inhibitors
Triamterene
Amiloride
Carbonic anhydrase inhibitors
Acetazolamide
DichloroEthaxazolamide
Osmotic diuretics
MannitolGlucose
Miscellaneous
CCBsARBs
Dopamine
Adenosin Receptor Antagonists
Potassium sparing diuretics
Spironolactone:It acts by competitive inhibition with aldosterone for specific intracellular receptors on DCT leading to NaCl loss and decrease K excretion.
It increases calcium excretion by direct action on the tubules
Action is dependent on aldosterone
PKs
Spironolactone : oral bioavailability ~75 %
Converted into metabolite (canrenone).
Delayed onset of action (max. diuretic effect 4 days)
Uses
It is a weak diureticMore useful in refractory edema which is associated with hyperaldosteronism in cases of liver cirrhosis, CHF and nephrotic syndrome.
Resistant HT
It is used (as K-sparing) to counteract the K+ loss due to thiazides or loop diuretics
Hyperkalemia especially in patient with renal diseases or co-therapy with ACIs, ARBs or with NSAIDs and B-blockers (reduced renin).
Gynaecomastia
Menstrual irregularities
Impotence
Metabolic acidosis
GI upset, confusion and skin rash
Side Effects
Hyperkalemia especially in patient with renal diseases or co-therapy with ACIs, ARBs or with NSAIDs and B-blockers (reduced renin).Gynaecomastia
Menstrual irregularities
Impotence
Metabolic acidosis
GI upset, confusion and skin rash
Eplerenone
Eplerenone is the first of a new class of drugs known as selective aldosterone receptor antagonists (SARA), which selectively block the aldosterone receptor with minimal effect at other steroid receptors.
like spironolactone, is a competitive antagonist of the aldosterone receptor.
Oral eplerenone is approved for use in patients with LV systolic dysfunction following MI.
PKs
It is 50% - 75% as potent as spironolactone
It is cleared primarily via metabolism by CYP3A4 toinactive metabolites, with an elimination half-life of 4 to 6 hours
Side Effects
Hyperkalemia and sex hormone–related side effects appear to be lower than with spironolactone.Mild dose dependent increases in cholesterol
Elevated serum transaminases and Thyroid-stimulating hormone was reported
Drug/Drug interaction with hepatic enzyme inducers/inhibitors
Eplerenone vs. Spironolactone
ParameterEplerenone
Spironolactone
Receptor Selectivity
SARA
Non-SARA
Potency
Less
More
metabolite
inactive
active
Duration of action
shorter
longer
Side effect profile
Less
high
Hepatic enzyme inducer/inhibitors I
Yes
No
Renal epithelial Na+ channel inhibitors
Triamterene and Amiloride
They non-aldosterone antagonists
Both are used in conjunction with thiazides and loop diuretics
Hyperkalemia is potential risk
Triamterene
Half life ~ 4 hrs
Leg cramps, renal stone, impaired glucose tolerance and photosensitivity are noted side effects
Amiloride
Its structurally related to but 10 times more potent than the triamterene
It decreases calcium excretion and increases urate excretion (uricosuric effect)
Half life ~ 15 hrs
Blocks entry of lithium into renal cells and mitigate DI caused by lithium
As aerosol – symptomatic improvement in cystic fibrosis by increasing fluidity of respiratory secretions
Carbonic anhydrase inhibitors
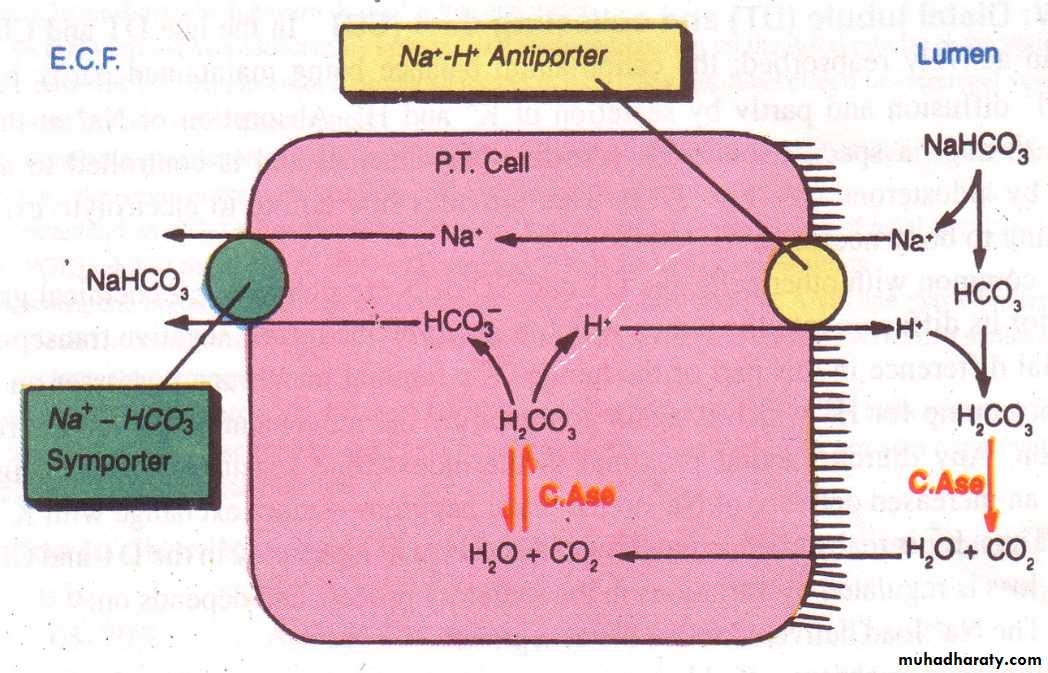
CA is an enzyme which catalyzes the reversible reactionH20 +CO2 «-------------» H2CO3.
Carbonic acid ionizes into HCO3 and H+, thus helps in the transport of CO2 and H+ secretion.
The CA enzyme is present in the renal tubular cells, gastric mucosa, pancreas, ciliary body and RBC.
Acetazolamide
The net effect is inhibition of HCO3 reabsorption in PCT.
The secretion of H+ is inhibited.
The distal Na+ is exchanged with K. So K+ loss in urine.
The urine produced is rich in bicarbonate -- alkaline urine – depletes body of HCO3---- producing acidosis.
Extra – renal actions:
Lowering of IOP due to decreased formation of aqueous humor.Decreased gastric acid and bicarbonate secretion.
Raised levels of CO2 in brain and lowering of pH – raising seizure threshold and sedation
Uses
Very weak diureticGlaucoma
To alkalinize urine (salycilate poisoning)
Epilepsy
Acute mountain sickness
Side effects
Drowsiness, Parasthesia and HeadacheAcidosis
Hypokalemia
Crystalurea and stone formation
Contraindicated in liver disease – interfere with elimination of ammonia
Osmotic diuretics
Mannitol
It is a non-electrolyte – pharmacologically inertNot metabolized, freely filtered in the glomerulus, undergoes no (limited) reabsorption
Inhibits water and electrolyte reabsorption
Expands extracellular fluid and increases GFR
Increases renal blood flow - salt reabsorption is reduced
Primary action is to increase urinary volume
Not absorbed orally – given I.V
Side effects
Headache, Nausea, Vomiting and allergyMiscellaneous
CCBs (DHPs group) have direct (intrinsic) diuretic effect. For ex. Nefidipine increase urine volume and Na excretion and may inhibit aldosterone release.ARBs and ACEIs, as they have antialdosterone effect, they act as K-retaining agent.
They should not be combined with other K-retainers especially in patients with renal impairment
Dopamine:
Indirect diuretic action: improvement in COP and cardiac function, so increase renal perfusion.
Direct effect: in case of fluid retention, stimulation of DA1 receptor on renal tubular cells which appose the effect of ADH.
Adenosin receptor antagoinsts:
They act by afferent arteriolar dilatation and increase GFR.
Special problems with diuretics
Overdiuresis
Resistance
Hyponatremia
Overdiuresis
Overdiuresis: overvigrous duiresis is common and may reduce intravascular volume and ventricular filling so that COP dropped thus tissue underperfusion occursOverdiuresis is seen during hospital setting when rigid policy is carried out. Some time the addition of ACEIs and ARBs enhance the risk of overdiuresis
Diuretic Resistance
Compensatory Mechanisms (RAAS, SNS)Failure to reach tubular site of action
a - Decreased G.I. absorption
b - Decreased secretion into tubular lumen
(e.g. uremia, decreased kidney perfusion)
c - Decreased availability in tubular lumen
(e.g. nephrotic syndrome)
Interference by other drugs (e.g. NSAID’s)
Tubular adaptation (ex chronic Loop diuretic use) (hypertrophy of distal nephron cells as a result of aldosterone induced growth ,)
Can Use Combination of Diuretics to Induce a Synergistic Effect (SNB)
Hyponatremia
Hyponatremia may occur especially in HF (elderly patients): Predominant H2O retention caused by:
In appropriate release of ADH
Increase activity of Ag II