University of Al Qadisiyah
College of PharmacyDr. Bassim I Mohammad,
MBChB, MSc, Ph.D
Cardiovascular Pharmacology
AntihypertensivesAntianginal
Drugs for HF
Antiarrythemics
Drugs for Hyperlipoproteniemia
Hypertension
Hypertension is currently defined as usual BP of ≥ 140/80 mmHg.
Hypertension may defined as an abnormal elevation of either SBP or DBP
Hypertension is a condition that afflicts almost 1 billion people worldwide and is a leading cause of morbidity and mortality.
More than 20% of Americans are hypertensive, and one-third of these Americans are not even aware they are hypertensive. Therefore, this disease is sometimes called the "silent killer"
Hypertension - Etiology
The are two basic types of hypertension:
Primary (essential or idiopathic) hypertension
Secondary hypertension
Hypertension – Aetiology
Primary hypertension: The majority of patients (90-95%) have essential hypertension, which is a form with no identifiable underlying cause.
This form of hypertension is commonly treated with drugs in addition to lifestyle changes
Secondary hypertension: A smaller number of patients (5-10%) have secondary hypertension that is caused by an identifiable underlying condition.
These patients are best treated by controlling or removing the underlying disease or pathology, although they may still require antihypertensive drugs
Causes of 2nd Hypertension
Renal or renovascular disease
Endocrine disease
Phaeochomocytoma
Cusings syndrome
Conn’s syndrome
Acromegaly and hypo or hyperthyroidism
Coarctation of the aorta
Pre-eclampsia
Stress (equivocal!!)
Iatrogenic (steroid, oral contraceptive, NSAIDs)
Normal <120 and <80
Prehypertensive 120-139 or 80-89Stage 1 Hypertension 140-159 or 90-99
Stage 2 Hypertension > 160 or >100
Target Organs
Stroke
LVH, IHD HF
Nephropathy
Retinopathy
A Significant CV and Renal Disease Risk Factor
Stroke
CAD
CHF LVH
Renal disease
Peripheral vascular disease
Morbidity
Disability
Goal of Treatment
To control blood pressure.
To prevent complications.
Because the majority of patients (with mild-moderate) HT are entirely asymptomatic our primarily goal is to decrease CV risk.
The objective of anti-HT therapy is to decrease BP (<140/80 mmHg) or even less in high risk patient like DM.
The benefit of treatment is greatest in those with high risk.
Non-Pharmacological Measures
Weight reduction (obese patients)
Aerobic exercise
Diet control
low calories, low fat, moderate Na intake
High in fruits and vegetables
fresh rather than proceed
Moderation of al cohol intake (red wine)
Cessation of Smoking
Independent risk factor
Malignant HT via renal artery damage.
What Determines Arterial Pressure?
Arterial Pressure = Cardiac Output * Peripheral ResistanceCardiac Output affected by (Heart Rate, Filling Pressure, Contractility)
Peripheral Resistance affected by (Arteriolar Radius)
Anti-hypertensive drugs
DiureticsBeta Blockers
a1-adrenoceptor antagonists (a1-blockers)
a2-adrenoceptor agonists
Angiotensin Converting Enzyme Inhibitors (ACE inhibitors)
Angiotensin Receptor blockers (ARBs)
Renin Inhibitors
Calcium Channel Blockers (CCBs)
Potassium Channel openers
Peripheral Vasodilators
Diuretics
Diuretics are basically acting as antihypertensive drugs by increasing Na and H2O renal excretion thereby decreasing the blood volume and CO. This is initial effects, later on diuretics decrease PVR.
As a class agents diuretics are effective in treating:
Patients with volume dependant form of HT (black, elderly, obese, renal).
HT complicated with HF.
Resistant HT
Renal impairment
Thiazides Diuretics
Thiazide and thiazide related agents are widely used as monotherapy or in combination with other antihypertensives (B-Blockers, ACEIs or ARBs).Low dose thiazide diuretics are effective and safe AntiHT agents in mild-moderate HT (12.5 mg of hydrochlorthiazide, chorthalidone and bendrofluzide).
Low dose TD are preferred initial therapy for HT especially in elderly, obese and black patients.
They are more effective in elderly and less effective in younger white.
TD are not effective when GFR severely reduced
Advantages of low dose TD:To minimize the adverse metabolic effects
To decrease the risk of impotence
To avoid E disturbances
To avoid risk of RCCa especially in women.
Loop Diuretics
Loop diuretics are not usually used as AntiHT agent (short acting, required multiple daily dosing).
However they are indicated in HT emergency, renal insufficiency and when multiple drugs with salt retaining properties are used.
B-blockers
PropranololAtenolol
Metoprolol.
Timolol
Nadolol
Primarily by decreasing HR, stroke volume and so COP followed by reduction in PVR.
Inhibit renin release from the kidney and so decreasing the formation of Ang II and aldosterone secretion.Release of vasodilator PGs.
Blockage of prejunctional B-receptors.
Ideal Profile of Anti-HT B-blockers
CardioselectiveLong acting (to prevent BP fluctuation)
Simple Pks profile (good patient compliance)
Effective in standard dose
Has added vasolilating effect
Has neutral effect on lipids
B-blocker
B-blockers are commonly used as first line therapy for HT especially for young (rather than elderly) , white (rather than black) patients or as alternative for diuretics.
B-blockers are suitable antiHT drugs for patients with increase adrenergic drive and those with renin value.
Conditions that discourage use of B-blockers
Severe COLDChronic sever congestive HF
Severe occlusive PVDs
These are commonly found in elderly and diabetic patients
ά –blockers:
PrazocinTerazocin
Doxazocin
Selective ά -blockers are competitive blockers of ά 1-adrenoceptors and they have direct vasodilating effect (due to PDE inhibition).
They decrease PVR and so Bp by dilating both arterioles and venules so they reduce preload and after load (balanced vasodilators).
They are free from metabolic side effects.
They have no or lesser place in initial monotherapy for HT.
These drugs are usually combined with B-blocker (to prevent reflex tachycardia) and diuretics (to counter salt and water retention).
Mild-moderate HT especially those patients with metabolic syndrome and those with BPH
PVDs
Refractory HF.
Side Effects
Reflex tachycardia
First-dose phenomena: brisk sever hypotension after the first or second dose of the drug usually 2 hours after administration. To avoid this phenomenon, we give the dose at bed time or start with small dose and increase it gradually.
Orthostatic hypotension
Nasal and conjunctival congestion
Failure of (or retrograde) ejaculation
Mixed ά and β-blockers
Labetalol: Hypertensive emergency and first line therapy for HT in black patientsCarvidolol: Mild-Moderate HF and first line therapy for HT in black patients
Drugs acting on RAAS
Angiotensin Converting Enzyme Inhibitors (ACEIs)Angiotensin Receptor Blockers (ARBs)
Renin Inhibitors
ACE Inhibitors
ARBsRenin Inhibitor
Captopril
Losartan
Aliskiren
Enanlapril
Irbesartan
Lisinopril
Candesartan
Ramipril
Valsartan
Perindopril
Telmisartan
Quinapril
Olmesartan
Angiotensin Converting Enzyme Inhibitor, ACEIs
CaptoprilLisinopril
Enlapril
Fosinopril
Zofinopril
ACEIs: Mechanism of Action
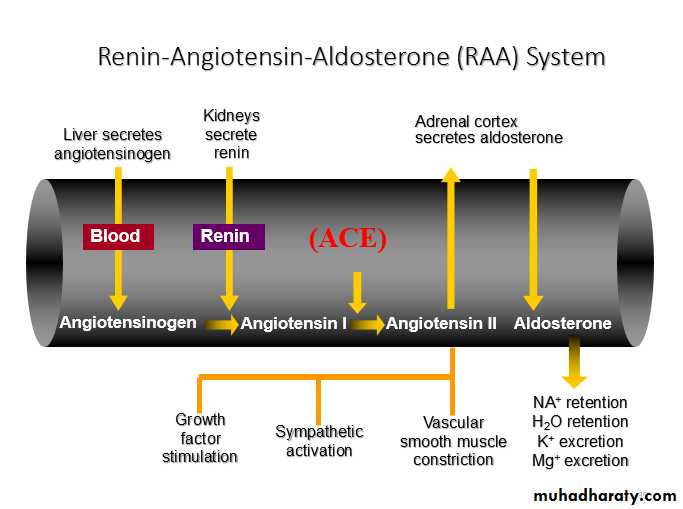
ACEIs: Mechanism of ActionRenin is produced by the kidney in response to renal ischemia, hypoxemia and B2-adrenergic stimulation.
Renin converts angiotensinogen (circulating protein) into Angiotensin-I (Ang I) which is inert substance.
Later, Ang-I is converted into Ang-II by the action of ACI (and by Chymases).
Ang-II is a potent vasoconsitrictor cuasing increase in PVR and stimulate aldosteron release (Na and H2O retention). Further Ang-II caues progressive vascular growth and end-organ damage.
Action of Ang-II is mediated through specific receptors called Ang receptors (AT1 and AT2).
AT1 (vasoconstriction, aldosterone release and vascular growth)
AT2 (antigrowth so has favorable effects)
ACEIs block the conversion of Ang-I to Ang-II. Further they lead to accumulation of Bradykinin (vasodilator) which is also substrate for ACE.
Decreased formation of Ang-II (vasodilatation and decrease aldosterone release) and accumulation of Bradykinin (vasodilatation) results in reduction in BP
Angiotensin II is one of the most potent vasoconstrictors known to man
Angiotensin II releases aldosterone from the adrenal cortex
Aldosterone enhances sodium and water retention and potassium loss from the kidney
Blood volume and BP increase as a result
Renin release from the juxtaglomerular cell
Sympathetic nerve stimulation – beta-1 receptor
Low blood sodium
Low renal artery pressure
Renin acts upon angiotensinogen to form angiotensin I
Angiotensin I is converted to Angiotensin II by a converting enzyme called ACE
Angiotensin II constricts the renal efferent arteriole more than the afferent arteriole
It therefore increases or maintains high glomerular filtration pressure
As mentioned previously, AT-II causes high levels of aldosterone, and therefore leads to water and salt conservation
Blocking the Renin-Angiotensin System
BP decreases MAINLY by lowered TPVR
Cardiac output is usually NOT significantly affected
For some reason, reflex sympathetic stimulation DOES NOT OCCUR
Absence of cardiostimulation makes these drugs safe in patients with ischemia
ACEIs: Uses
Hypertension: as monotherapy or in combination therapy.
Heart failure
MI: post MI phase, they prevent vascular and cardiac remodelling.
Asymptomatic LV dysfunction, they prevent development of overt CHF.
Nephroprotection: prevent protein urea in diabetic and non-diabetic nephropathy.
Side Effects
Hypertension: as monotherapy or in combination therapy.Heart failure
MI: post MI phase, they prevent vascular and cardiac remodelling.
Asymptomatic LV dysfunction, they prevent development of overt CHF.
Nephroprotection: prevent protein urea in diabetic and non-diabetic nephropathy.
Calcium Channel Blockers (CCBs)
Dihydropyridines (DHP)
Non-DHP
Dihydropyridines (DHP)
Non-DHPNifedipine
Nimodipine
Amlodipine
Felodipine
Isradipine
Diliazem
Verapamil
CCBs: Mechanism of Action
CCBs block the inward movement of the Ca by binding and blocking the L-type voltage gated Ca channels in the heart and smooth muscles (of peripheral arterioles and coronary arteries) causing dilatation and relaxation mainly of the arterioles.
All CCBs are therefore vasodilators decreasing arteriolar tone and systemic PVR resulting arterial BP (decrease after load).
In addition CCBs decrease myocardial contractility (-ve inotropic) and the conduction in cardiac muscles (- chronotropic)
Diliazem and verapamil: primary action on heart
Dihydropyridines: primary action on arterioles
Peripheral Effects: Nefidipine >Diliazem > verapamil
Cardiac Effect: verapamil >Diliazem > Nefidipine
CCBs: PKs
They are orally active agents;Verapamil and nicardipine are also given by IV route
Most of them have short half lives
High plasma protein binding and extensive metabolism
All CCBs are save in pregnancy and renal failure
CCBs: Uses
Hypertension and HT emergencies: CCBs are alternative first line antihypertensive agents and can be used safely in pregnancy, asthma, DM or renal impairment. Nifidipine (SL) and nicardipine (IV) are used in HT emergenciesAngina pectoris (stable, unstable and it’s the drug of choice in variant type)
As antiarrythmeic especially verapamil; it is the second choice in treatment or termination of SVT
PVDs
Subarrchinoid hemorrhage (nimodipine causes cerebral vasodilatation
Al though CCBs are contraindicated in HF, amlodipine can be used in the treatment of HF
Migraine prophylaxis especially verapamil
Tocolytics
CCBs: Side effects
Headache, flushing of the face and dizziness
Edema (nifedipine)
Constipation (verapamil)
Gingival hyperplasia
AV block & heart failure (verapamil and diltiazem)
Drug interactions: beta blockers (verapamil and diltiazem), cimetidine
Centrally Acting Drugs
MethyldopaClonidine
Direct Vasodilators
HydralazineMinixidil
Diazoxid
Hypertensive emergencies
Sodium NitroprussideGTN
Diazoxide
Hydralazine
Enalaprilat
Nicardipine
Esmolol
Nifedipine – Sublingual
Fenoldopam