Stroke
Stroke: is acute, focal brain dysfunction due to vascular disease, is the third most common cause of death in high-income countries after cancers and ischemic heart disease, and the most common cause of severe physical disability. Stroke accounts for 11% of deaths in England and Wales; About 750 000 new strokes occur and about 150 000 people die from stroke in the United States each year. Around half of all stroke survivors are left dependent on others for everyday activities: if a patient can return home, the burden on careers is significant. One-quarter of all strokes occur in people below the age of 65 years.The underlying pathology responsible for the persistent symptoms of stroke is either infarction or haemorrhage.
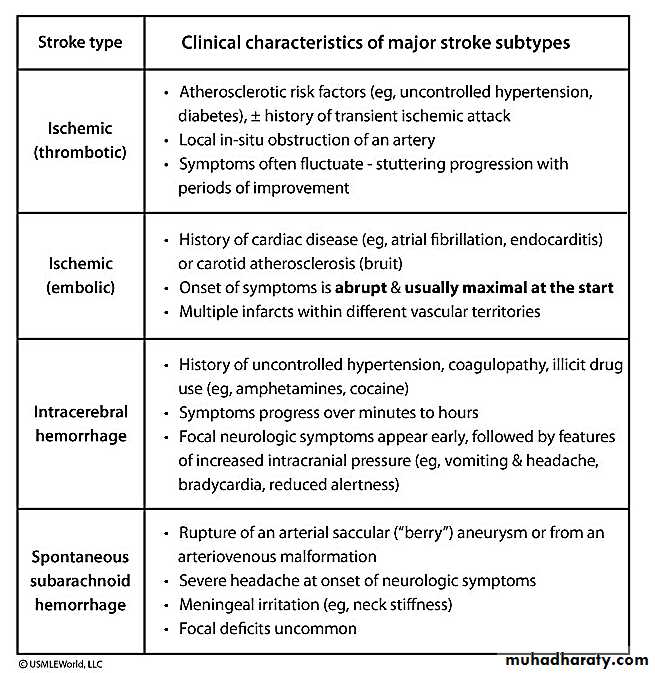
Haemorrhage is subdivided according to location into intracranial haemorrhage and subarachnoid haemorrhage, while infarction is caused by either embolic (Sudden) or thrombotic (gradual)
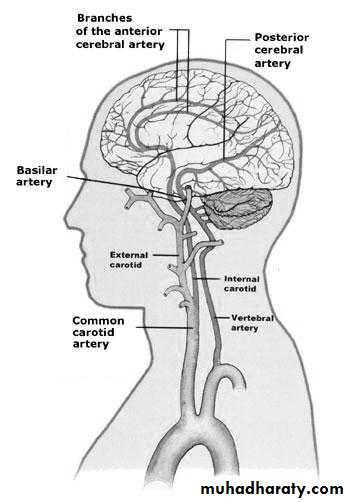
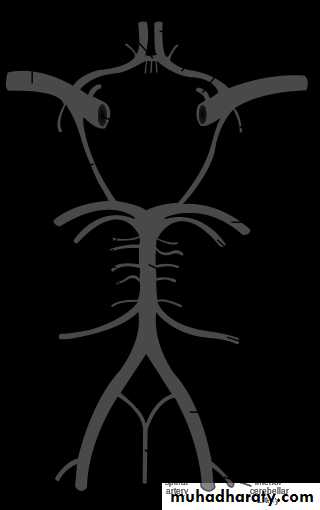
The main arterial supply of the brain comes from the internal carotid arteries, which supply the anterior brain, and the vertebral and basilar arteries (vertebrobasilar system), which provide the posterior circulation. The anterior and middle cerebral arteries supply the frontal and parietal lobes, while the posterior cerebral artery supplies the occipital lobe. The vertebral and basilar arteries perfuse the brain stem and cerebellum; Communicating arteries provide connections between the anterior and posterior circulations and between left and right hemispheres, creating protective anastomotic connections that form the circle of Willis.
Three stroke types:
IschemicStroke Clot occludingartery85%Intracerebral HemorrhageBleedinginto brain10%Subarachnoid Hemorrhage Bleeding around brain5%When infarction involves only a small volume of the tissue (<1.5 cm in diameter on computerized tomography [CT]) secondary to occlusion of a penetrating artery, the resulting death of tissue is known as a lacuna or a lacunar infarct. The underlying pathology responsible for lacunar infarction is often referred to as small vessel disease. Lacunas are generally found in subcortical white matter or the basal ganglia. Larger infarcts usually involve a wedge of both cortical and subcortical white matter and result from occlusion of the trunk or branches of the major cerebral arteries.
Vessel Stroke Syndrome:
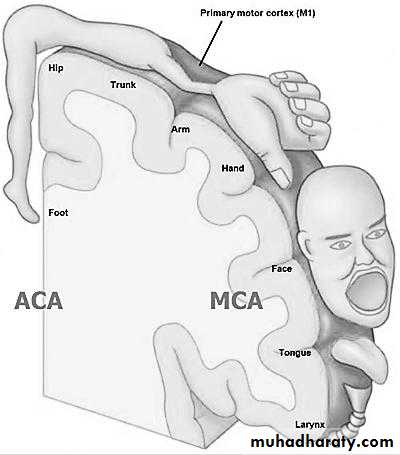
Middle cerebral artery (MCA):
Arm>leg weakness
Left (MCA) : Aphasia
Right (MCA ) : Neglect
Anterior cerebral artery (ACA):
Leg>arm weakness, Voluntary control of micturition may be impaired
Posterior cerebral artery (PCA):
Hemianopia
Cerebellar arteries
Ipsilateral ataxia
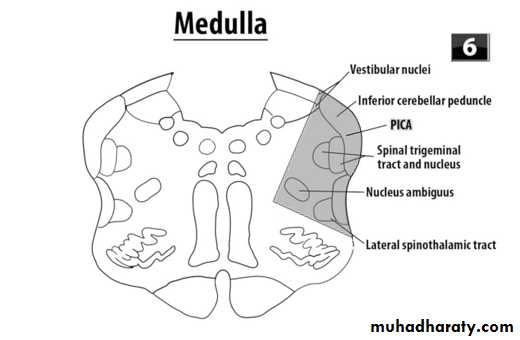
Brain stem vessels
Cross signs (ipsilateral cranial nerve plus contralateral weakness or sensory loss) e.g.:Posterior inferior cerebellar artery occlusion (PICA): results in the lateral medullary (Wallenberg) syndrome. This syndrome varies in its presentation with the extent of infarction, but it can include ipsilateral cerebellar ataxia, Horner syndrome, facial sensory deficit and dysphagia; contralateral impaired pain and temperature. The motor system is characteristically spared because of its ventral location in the brainstem.
Risk factors for stroke
Non modifiable risk factorsAge
Gender (male > female except at extremes of age)
Race (Afro-Caribbean > Asian > European)
Previous vascular event:
Myocardial infarction
Stroke
Peripheral vascular disease
Heredity
Modifiable risk factors
Hypertension
Smoking
Hyperlipidemia
Diabetes mellitus
Excessive alcohol intake
Oral contraceptive pill
Polycythemia
Heart disease
Atrial fibrillation
Congestive cardiac failure
Obesity
Differential diagnosis of stroke and TIA
Brain tumors
Syncope
Hypoglycemia
Migrainous aura
Focal seizures
Encephalitis
Demyelination disease e.g. : multiple sclerosis
Conversion disorder
Several terms have been used to classify strokes, often based on the duration and evolution of symptoms:
Transient ischemic attack (TIA) describes a stroke in which symptoms resolve within 24 hours. The term TIA also includes patients with amaurosis fugax, usually due to a vascular occlusion in the retina most likely due to carotid stenosis lead to transient foggy scene in one eye.
Progressing stroke (or stroke in evolution) describes a stroke in which the focal neurological deficit worsens after the patient first presents. Such worsening may be due to increasing volume of infarction, hemorrhagic transformation or increasing cerebral oedema.
Completed stroke describes a stroke in which the focal deficit persists and is not progressing
Investigation of a patient with an acute stroke
Is it a vascular lesion? …… CT/MRI
Is there any cardiac source of embolism? (ECG) & Echocardiogram
What is the underlying vascular disease? Duplex ultrasound of carotids
What are the risk factors? Full blood count, lipid profile & blood glucose
Management of acute stroke
Airway: Perform bedside swallow screen and keep patient nil by mouth if swallowing unsafe or aspiration occurs.
Breathing: Check respiratory rate and oxygen saturation and give oxygen if saturation < 95%.
Circulation & BP: Unless there is heart or renal failure, evidence of hypertensive encephalopathy or aortic dissection, do not lower blood pressure in first week as it may reduce cerebral perfusion. Blood pressure after that should be controlled …
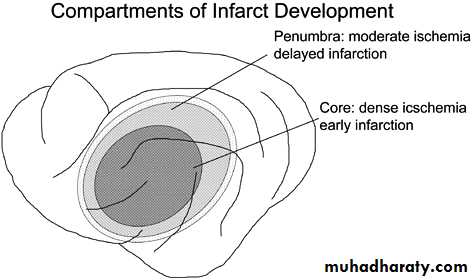
Penumbra
At the center of an infarct the damage is most severe but at the periphery collateral flow may allow continued delivery of blood, although at a lower rate. This zone may become dysfunctional secondary to electrical failure although not dead and is referred to as the ischemic penumbra, once blood flow falls below the threshold for the maintenance of electrical activity, neurological deficit develops. At this level of blood flow the neurons are still viable; if the blood flow increases again, function returns; however, if the blood flow falls further, irreversible cell death occur.Consensus exists that medications should be withheld unless the systolic blood pressure is >220 mm Hg or the diastolic blood pressure is >120 mm Hg in early days unless there is contraindication to keep high BP or we decide to give thrombolytic drug.
This high BP will help to reperfuse the penumbra and keep it viable.
Save the penumbra
CEREBRALBLOODFLOW(ml/100g/min) CBF< 8CBF8-18TIME (hours)123201510 5 PENUMBRACORENeuronal dysfunctionNeuronal deathNormal functionNutrition & hydration: Assess nutritional status and provide nutritional supplements if necessary, if dysphagia persists for > 48 hrs. Start feeding via a nasogastric tube. Hydration by IV fluid may need use isotonic fluid e.g.: GS or NS avoid GW because it exacerbate brain oedema.
Blood glucose: Check blood glucose and treat when levels are ≥ 11.1 mmol/L (200 mg/dL) (by insulin infusion or glucose/potassium/insulin (GKI) ;Monitor closely to avoid hypoglycemia
Temperature: If pyrexic, investigate and treat underlying cause, Control with antipyretics, as raised brain temperature may increase infarct volume.
Incontinence: Check for urinary retention; treat Appropriately, Avoid urinary catheterization unless patient is in acute urinary retention or incontinence is threatening.
Immediate medication include:
Thrombolysis
Intravenous thrombolysis with recombinant tissue plasminogen activator (rt-PA, it should be given within 4.5 hours of symptom onset to carefully selected patients with inclusion and exclusion criteria.Aspirin
In the absence of contraindications, aspirin (300 mg daily) should be started immediately after an ischemic stroke unless rt-PA has been given, in which case it should be withheld for at least 24 hours. Aspirin reduces the risk of early recurrence and has a small but clinically worthwhile effect on long-term outcome.
Strategies for secondary prevention
Lifestyle modificationPatients with the relevant risk factors should be strongly advised to stop smoking, eat healthily to reach and maintain a normal weight, to take regular exercise and reduce excessive alcohol consumption.
Lowering blood pressure
optimum targets: below 140/85 mmHg in general and below 140/80 mmHg for patients with diabetes ,started with thiazide diuretic and then add an ACE inhibitor, If further reduction in blood pressure is required, calcium antagonists can be added
Antiplatelet drugs:
Aspirin 100 mg or clopidogril 75 mg or aspirin/dipyridamole
Lipid lowering agent :
Starting with a statin after ischemic stroke dramatically reduces the risk of recurrent stroke and MI.
Anticoagulation:
Just in case of patients with cardio-embolic sources of thrombus such as AF (atrial fibrillation) anticoagulation will be indicated.Carotid endarterectomy:
Ischemic stroke or TIA with Recently symptomatic severe carotid stenosis
Control of blood glucose:
It is important to maintain HbAc1 levels at less than 7%.
Complications of acute stroke:
Chest infection: Avoid aspiration (nil by mouth, nasogastric tube, possible gastrostomy) treatment by Antibiotics &Physiotherapy
Epileptic seizures: Maintain cerebral oxygenation, Avoid metabolic disturbance treatment by Anticonvulsants.
Deep venous thrombosis/ pulmonary embolism: Maintain hydration, early mobilization, Anti-embolism Stockings or Heparin.
Painful shoulder: Avoid traction injury Shoulder/arm supports Physiotherapy, Local corticosteroid injections may needed.
Pressure sores: Frequent turning, Monitor pressure areas Avoid urinary damage to skin, nursing care And Pressure-relieving mattress.
Urinary infection: Avoid catheterization if possible Use penile sheath. Treatment by antibiotic.
Depression and anxiety: Maintain positive Attitude, treatment by antidepressant.
Constipation: Appropriate aperients and diet
End
The table, picture &clinical cases below were added by the students (it’s not included in the lecture):
ACA: Anterior cerebral artery
MCA: Middle cerebral arteryNote:
The picture above indicate the homunculus which is the representation of the body parts in the brain. Please note that the ACA supply the medial side of the brain which usually represents the lower limb while the MCA supply more lateral side of the brain and it represents the hand and face. This will allow us to localize the vessel involved by the history and examination only as in the case below.Case 1/
A 70-year-old Caucasian male is brought to the emergency department due to a sudden onset of right-sided weakness and urinary incontinence about ten hours ago. His past medical history is significant for type 2 diabetes for the last 20 years and hypertension for the last 28 years. On examination, there is 4/5 power in the right upper extremity and 1/5 power in the right lower extremity. Babinski's sign is positive on the right side. The sensations are decreased over the right foot and leg. Visual fields are full (no defects). Which of the following is the most likely diagnosis?
Lacunar stroke.
Anterior cerebral artery stroke
Right middle cerebral artery stroke
Left middle cerebral artery stroke
Posterior cerebral artery stroke
Explanation:
Strokes can be classified as hemorrhagic (intracerebral hemorrhage or subarachnoid hemorrhage) or ischemic (secondary to thrombosis, embolism, or systemic hypoperfusion). A good history and neurologic examination of a patient with a stroke can often localize the region of brain dysfunction and affected vasculature.
The blood supply of the brain is summarized as follows:
1 . Anterior vasculature - comprised of the internal carotid artery and its branches, especially the paired anterior and middle cerebral arteries
2. Posterior circulation- comprised of the paired vertebral arteries, which unite to form the basilar artery, which further divides into the paired posterior cerebral arteries
In this case, the patient most likely has an anterior cerebral artery stroke. This condition is characterized by contralateral motor and/or sensory deficits which are more pronounced in the lower limb than the upper limb (as seen in this case). Other features that may be seen include urinary incontinence, gait apraxia, primitive reflexes (e.g., grasp and sucking), abulia, and paratonic rigidity.
So the answer is B
Case 2/
A 62-year-old male is brought to the emergency department with a chief complaint of weakness. He says that he was walking his dog 1 hour ago when he began to limp and noticed some weakness in his left arm. His past medical history is significant for hypertension treated with hydrochlorothiazide, and type II diabetes mellitus managed with metformin. He denies nausea, vomiting, chest pain, fever or chills. He does note occasional palpitations and tension headaches at baseline. On physical examination, his blood pressure is 170/95 mmHg and his heart rate is 76/min and regular. His blood glucose level is 190 mg/dl and his HbA 1 c is 7.6%. The neurological examination is significant for profound left-sided weakness and an upgoing Babinski reflex on the left. Non-contrast head CT is negative for any intracranial bleed. Which of the following is most likely to increase his chance of neurological recovery?
Insulin fortight glucose control
Labetalol
Aspirin
Fibrinolytics
Heparin
Explanation:
This patient's left-sided weakness and positive Babinski sign are consistent with acute ischemic stroke, especially given his risk factors of hypertension and type II diabetes. His history of occasional palpitations may indicate paroxysmal atrial fibrillation as well, which would put him at risk for cardiac emboli. In all patients with symptoms of stroke, a head CT without contrast should be obtained as soon as possible to rule out hemorrhage, as hemorrhagic and ischemic strokes are treated differently. Once hemorrhage is ruled out, fibrinolytic therapy should be considered. Intravenous alteplase (tPA) has been shown to improve outcomes in victims of ischemic stroke when given within 3 to 4.5 hours of symptom onset. Because this patient's symptoms began just 1 hour ago, he is a good candidate for fibrinolytic therapy (Choice D). The sooner tPA is administered, the better the outcome.
So the answer is D