Forth stage
Obstetric
Lec-1/2/3
د
.
أ
ﺣ
ﻣ
د
ﺟ
ﺎ
ﺳ
م
20/10/2015
Early pregnancy disorders
Disorders of early pregnancy :
-Early pregnancy loss :
more pregnancies are lost in the early weeks than at any
other stages of pregnancy.
Three of the main categories of early pregnancy loss are:
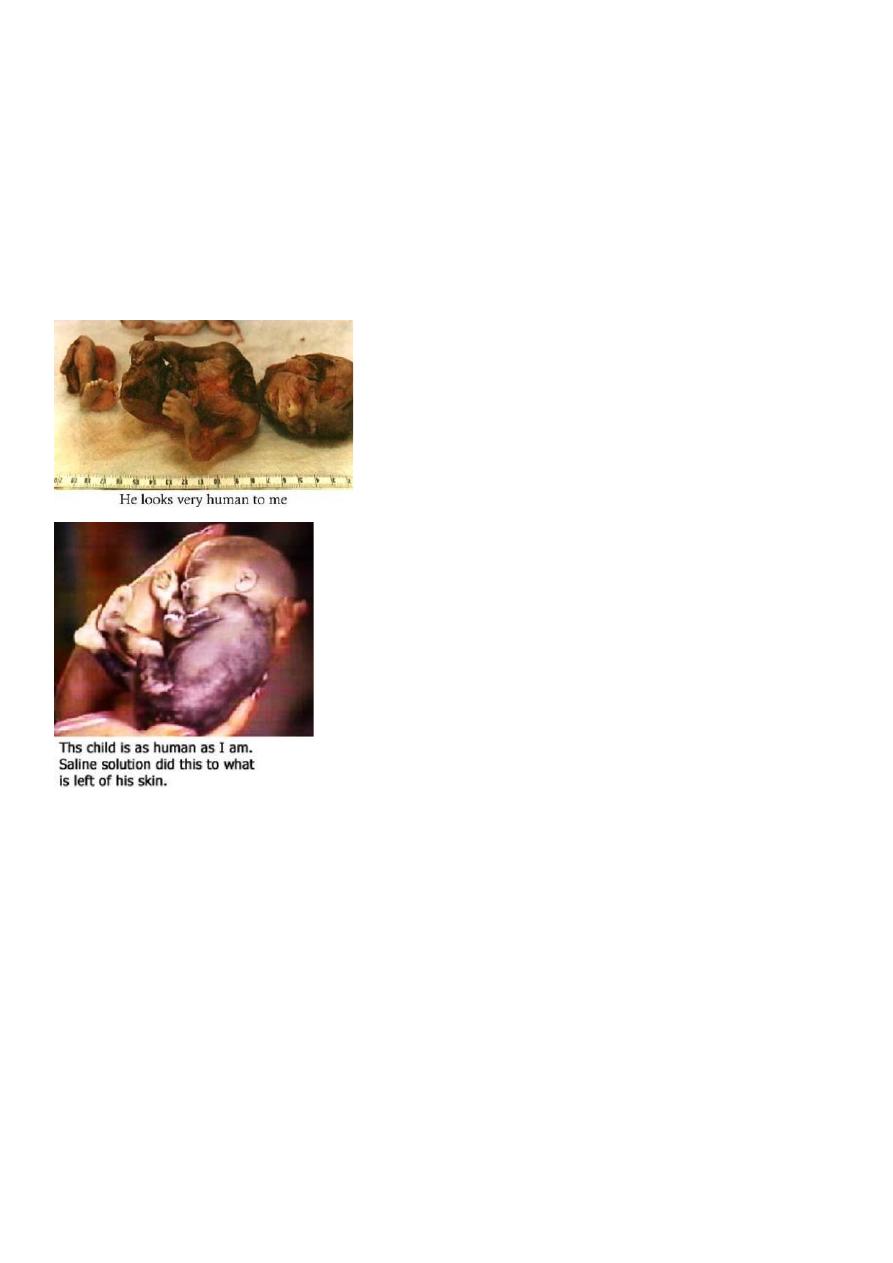
1-abortion (spontaneousabortion , induced abortion ).
2-ectopic pregnancy.
3-hydatidiform mole.
Abortion (miscarriage):-
Is the termination of pregnancy before time of viability which is the 24th weeks of
pregnancy , Viability mean the time where fetus is capable of surviving outside
uterus , (Some consider time of viability as 24th weeks and others considered it as
20th weeks or 22nd weeks)(in our locality 24th weeks).
The most common time for abortion is 7-13 weeks of gestation.(because the placenta
still not formed)
Abortion types:
1-spontaneous 2-induced
Incidence of abortion
it is expulsion of the products of conception without medical or surgical intervention .
15-20% in early pregnancy. The rate of abortion is known to decrease with increasing
gestational age from 25% at 5-6 weeks to 2% after 14 weeks .
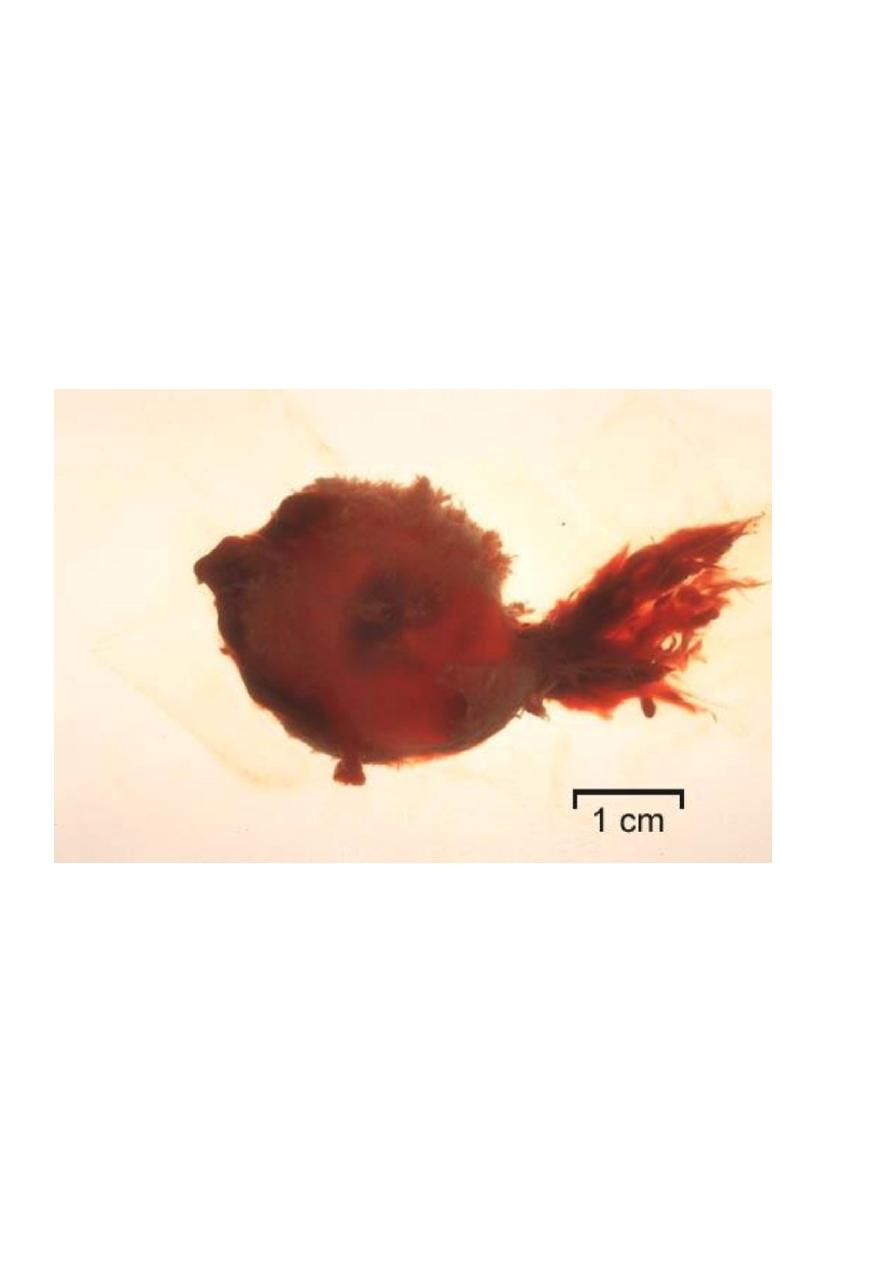
Blighted Ovum (Anembryonic pregnancy):
Those early pregnancy loss in which fetal development is not observed with ultrasound and
fetal tissue is absent on the histologic examination of product of conception. It is caused by
genetic cause
Causes of spontaneous miscarriage:
1- maternal causes 2- fetal causes
1-Maternal causes :-
A.General :
1-Acute febrile illness.
2-infection (bacterial vaginosis, syphilis, rubella). Any severe infection that leads to
bacteraemia or viraemia can cause sporadic miscarriage.
3- Severe hypertension
4-Severe renal disease
5-Badly controlled Diabetes mellitus.
6-Hypothyrodisim.
7-Severe malnutrition
8-Trauma.
-direct penetrating injury
-surgery (abdominal, pelvic)
-amnicentesis (aspiration of the aminiotic fluid from the amniotic sac)
-chorionic villous sampling
9-Poisons (cytotoxic drug, lead, quinine, ergot, smoking, alcohol)
B.local causes :
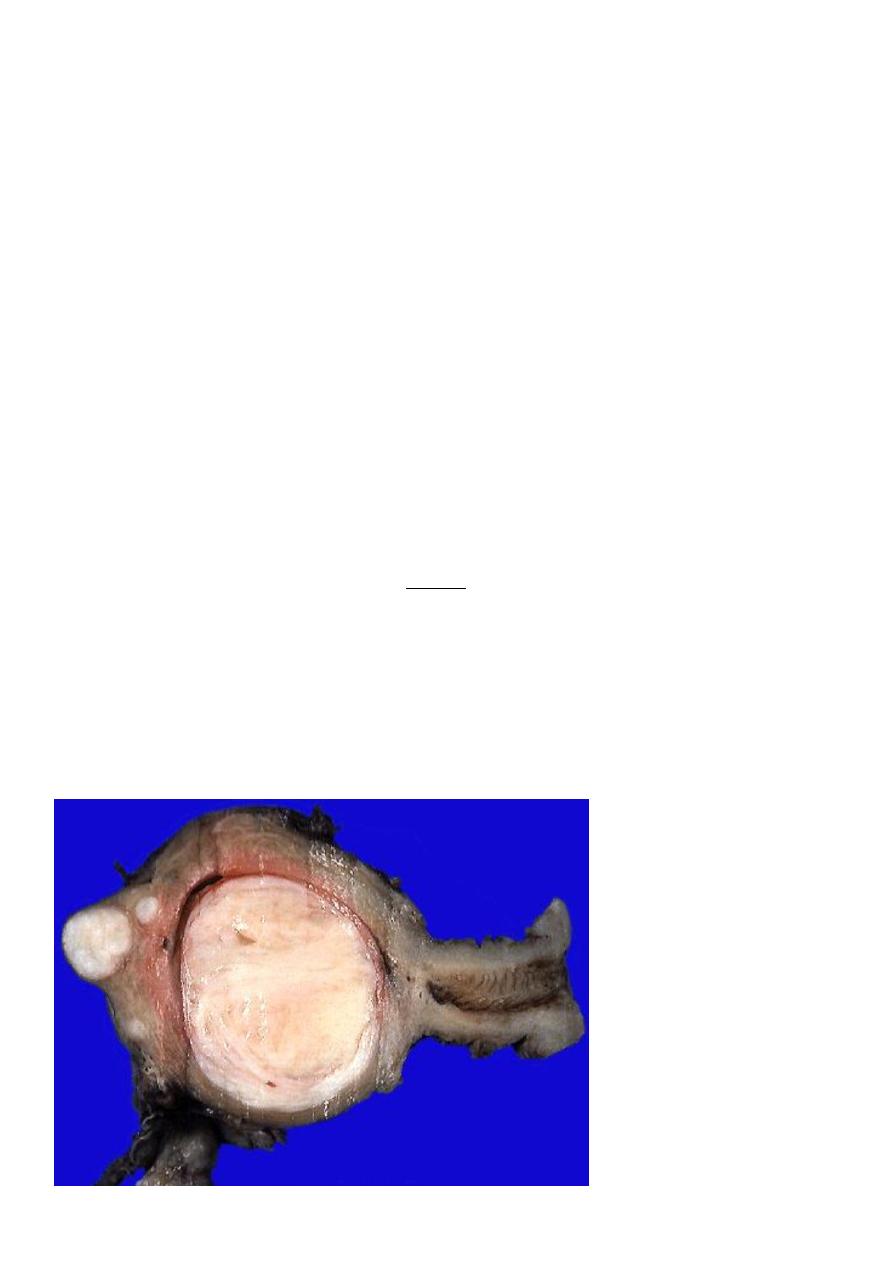
1-Uterine fibroids. (submucous fibroid related to uterine cavity ,like leomyoma).
2-Congenital abnormalities (double, septate uterus).
3-Cervical incompetence/ weakness.
).
(Fixed
Incarcerated retroverted uterus in pelvis
-
4
5-Asherman's syndrome (intrauterine adhesion).
6-Presence of intrauterine contraceptive device (IUCD).
7-Abnormalities of implantation (low implantation of placenta).
Uterin fibroid
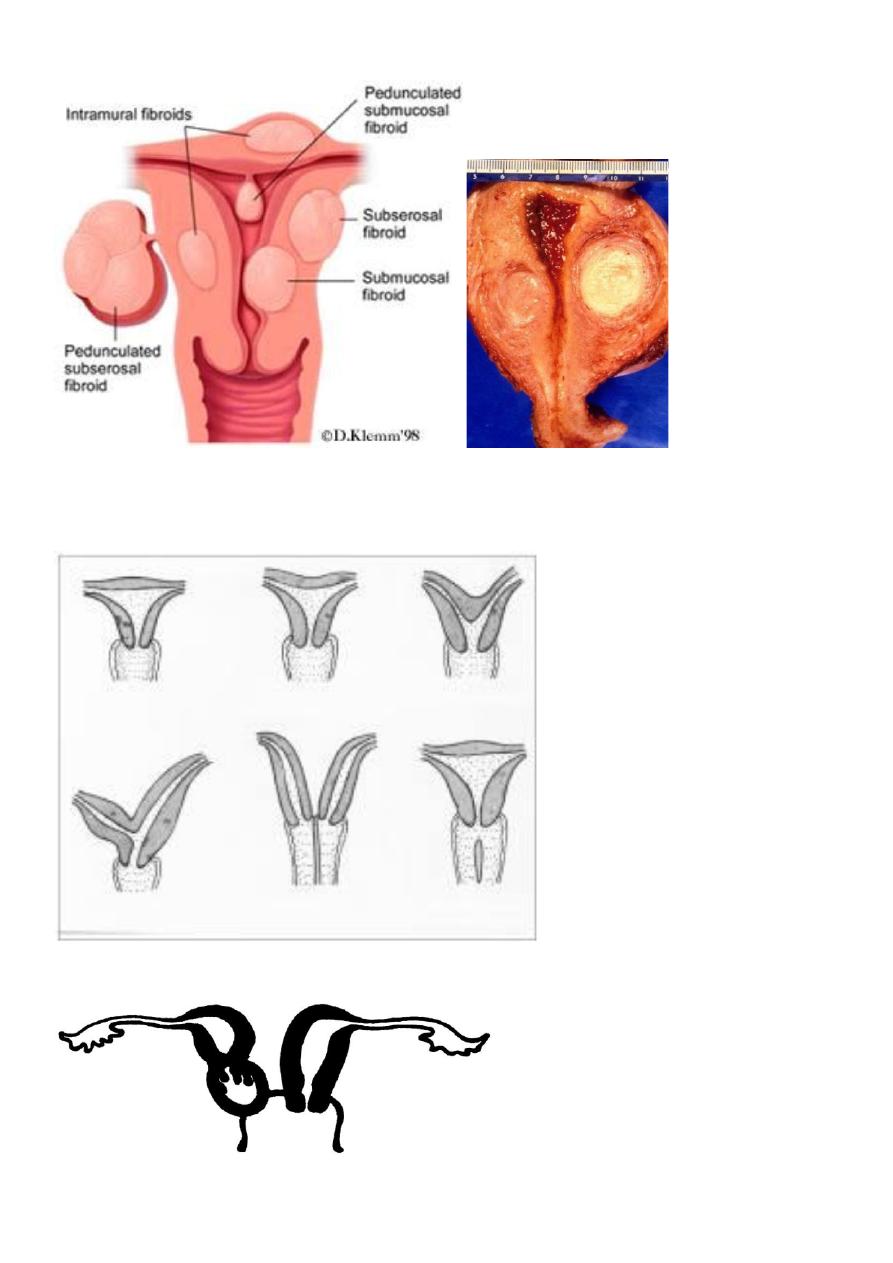
congenital anomalies of uterine
2-Fetal causes:
-Fetal abnormalities.
-multiple pregnancy.
3-immunological causes factors:
a. autoimmune disease (antiphospholipid antibody, thrombophilia, any persistent and
identifiable hypercougulable state either acquired or inhertant).b. Rh incompatibility
(occasionally)
. 4. Endocrine abnormalities:
a. luteal phase inadequacy.
b. hypersecration of LH.
Pathological anatomy:
First trimester of pregnancy(1
st
13 weeks):
The attachment of chorion to deciduas is so delicate that separation may follow strong
uterine contractions produced by any cause. The resulting hemorrhage into the chorio-
decidual space leads to further separation.
In other cases fetal death precedes uterine contractions.
The deciduas basalis remains in the uterus, and membranes and most of deciduascapsularis is
expelled.
In some cases the gestation sac is retained in uterus for days or weeks as a missed abortion
Second trimester(after 13 weeks):
the placenta is a definite structures, and if happen after this time the process of abortion is
similar to that of labour. Bleeding and painful contractions are followed by dilatation of
cervix, rupture of membranes and expulsion of fetus and placenta. If a conceptus is expelled,
normal uterine involuation follows, but frequently part of placenta is retained with some
blood clots.
Clinical varieties of miscarriage (spontaneous abortion):
1-Threatened abortion
2-Inevitable abortion:
3-Incomplete abortion:
4-Complete abortion:
5-Missed abortion:
6-Septic abortion:
7-Recurrent abortion (Habitual):
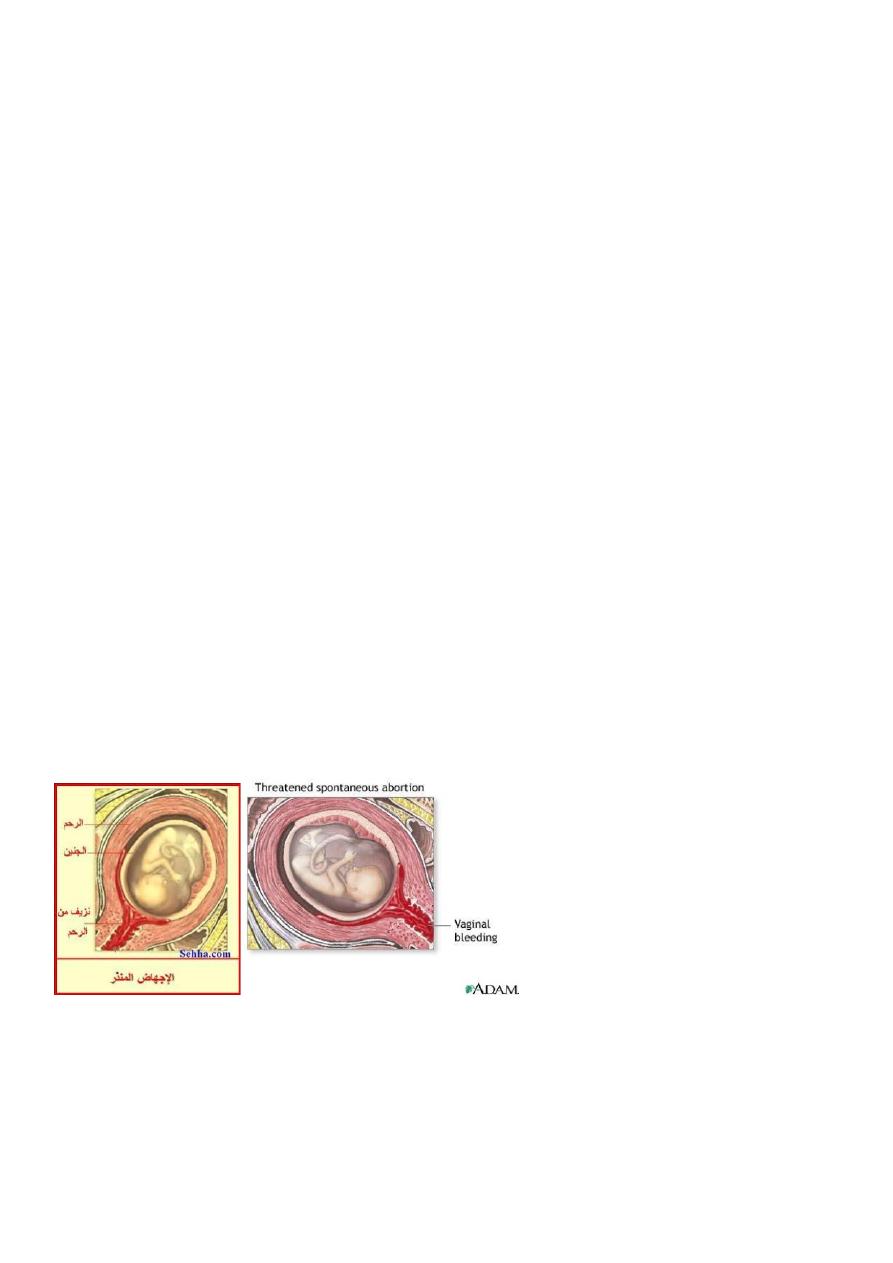
1-Threatened abortion:
symptoms:
1.scanty uterine bleeding(fresh blood) preceded by symptoms of pregnancy(frequency
urination , backache , morning sickness , amenorrhea).
2.pain is usually absent but may be backache or mild lower abdominal pain.
Signs (Examination):
1.uterus is enlarged corresponding with date of amenorrhoea.
2.cervix is closed.
3.no pelvic tenderness
Investigations:
1-Ultrasound :confirm intrauterine gestation (IUG) and fetal heart (FH).
2-Human Chorionic Gonadotrophin (hCG) increase in serial measurement.
Treatment :
1-No specific treatment needed. only need reassurance and rest until bleeding stopped.
2-Progesterone, hCG it's benefit is not confirmed yet???
3-Anti D (250unite) should be given to non sensitized Rh negative women.
Prognosis :
50% of pregnancy have successful outcome and increase risk of:
-Preterm labour
-Low birth weight
-Perinatal death.
-Antepartum hemorrhage
-Manual removal of the placenta
-Cesarean delivery.
appear to be increased.
not
Risk of a malformed surviving infant does
2-Inevetible pregnancy :
Means that it is impossible for the pregnancy to continue and the process is now irreversible
Symptoms:
1.severe vaginal bleeding because a large area of the placenta has detached from the uterine
wall.
2. It is accompanied by acute abdominal pain which is similar to the pattern of uterine
contractions in labour (intermittent).
3. No products of conception expelled yet.
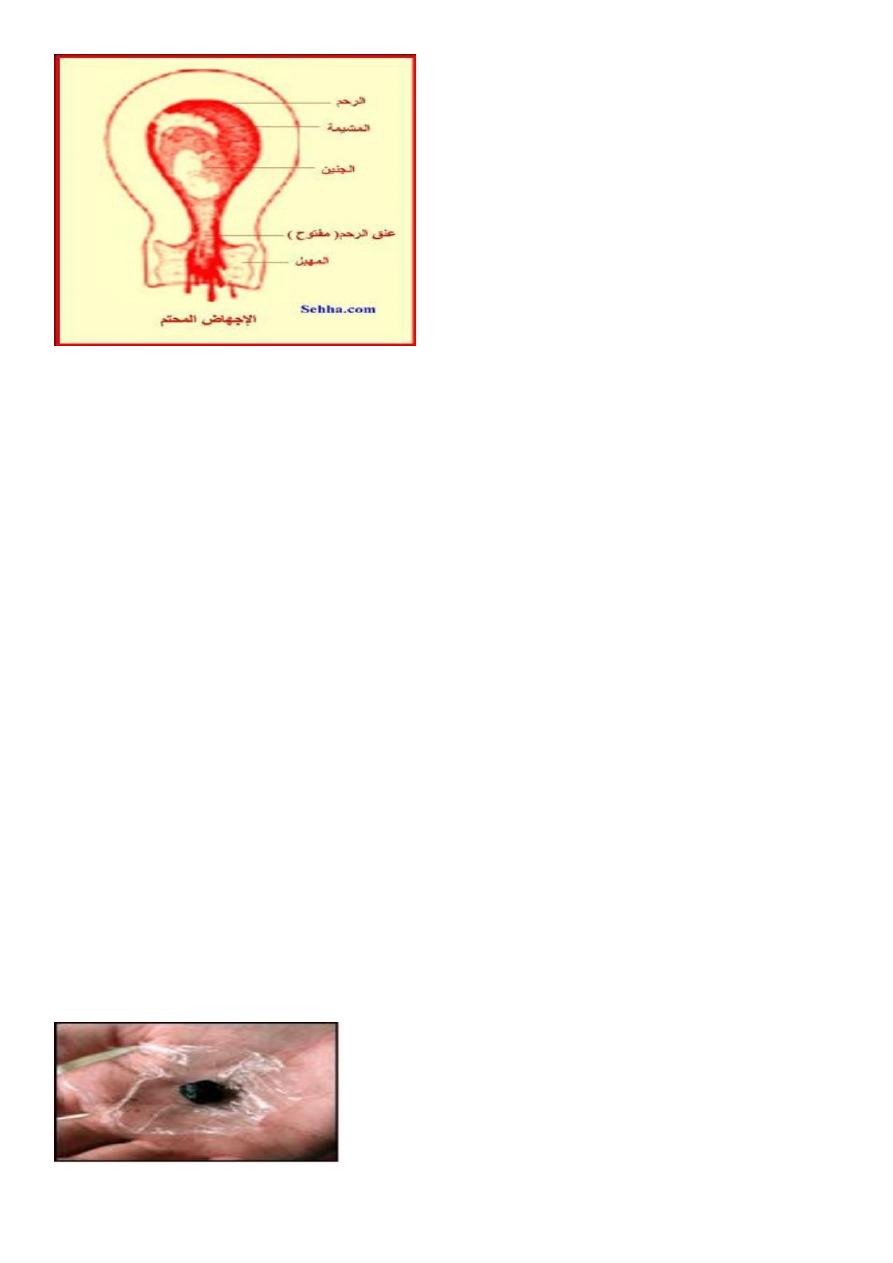
Signs:
Uterus is enlarged.
Internal os is dilated (open).
Treatment:
Once the diagnosis is made, uterus should be evacuated
a-in first trimester :Evacuate uterus under general anesthesia by curettage or suction
curettage (without cervical dilatation because cervix is already dilated).
b-in second trimester :Allow miscarriage to take place spontaneously and the process can
be expedited and bleeding controlled with ergometrine 0.5mg and oxytocin 5unit(increase
contractionof uterus) or prostaglandin in addition to supportive therapy (correction of blood
loss, analgesia, antibiotic is given as necessary).
Uterus need evacuation if patient not abort all the product of conception and severe bleeding
was associated.
Anti D (250unite) should be given to non sensitized Rh negative women
3-Incomplete abortion :
Symptoms are the same as for inevitable abortion but some products of conception are
passing from uterus and part of product of conception retained in the uterus or cervical canal,
a situation that causes ongoing cramping and excessive bleeding with danger of shock and
sepsis.
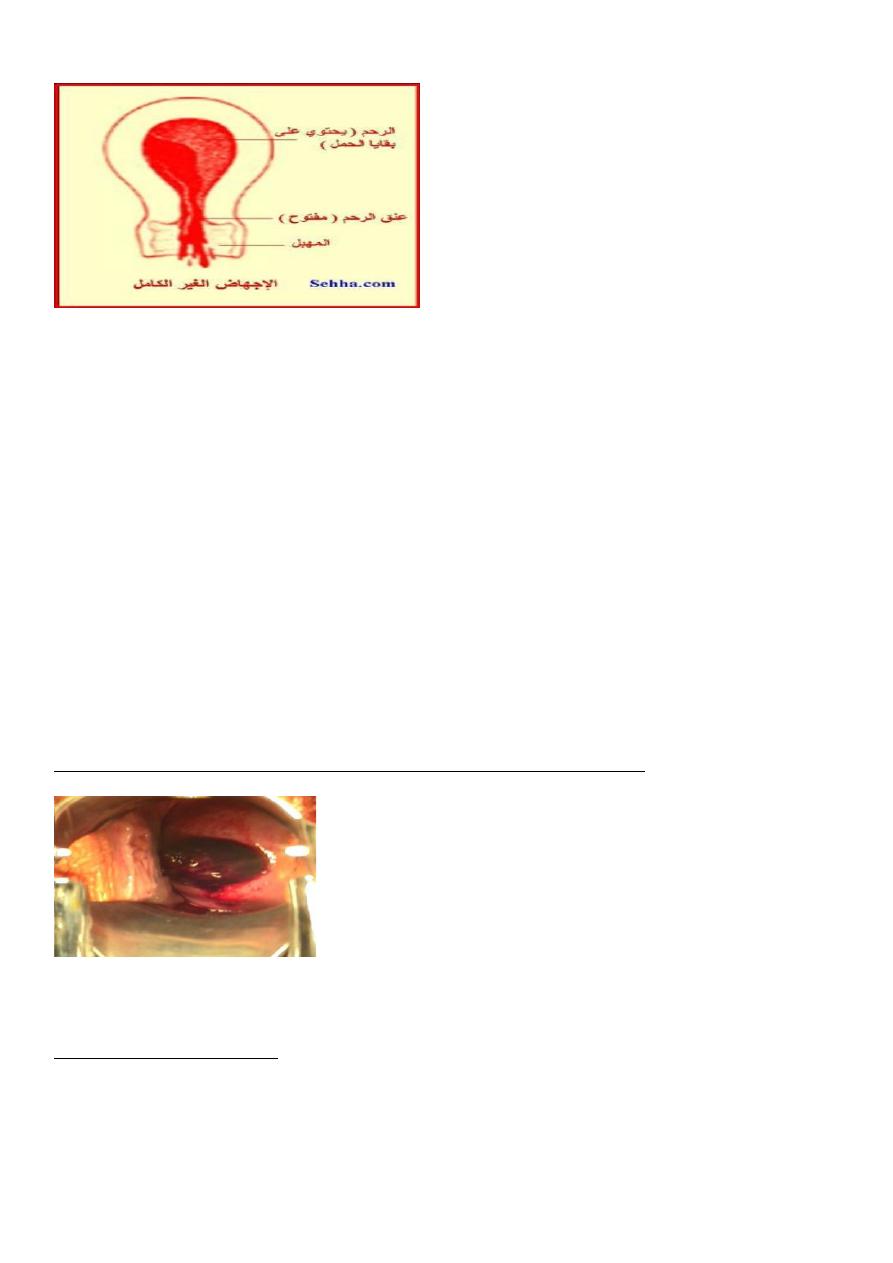
Symptoms:
1. uterine bleeding which is varies may be severe to cause hypovolemia or mild
2.history of passing part of conception (Women describe the product of conception as
looking like pieces of skin or liver).
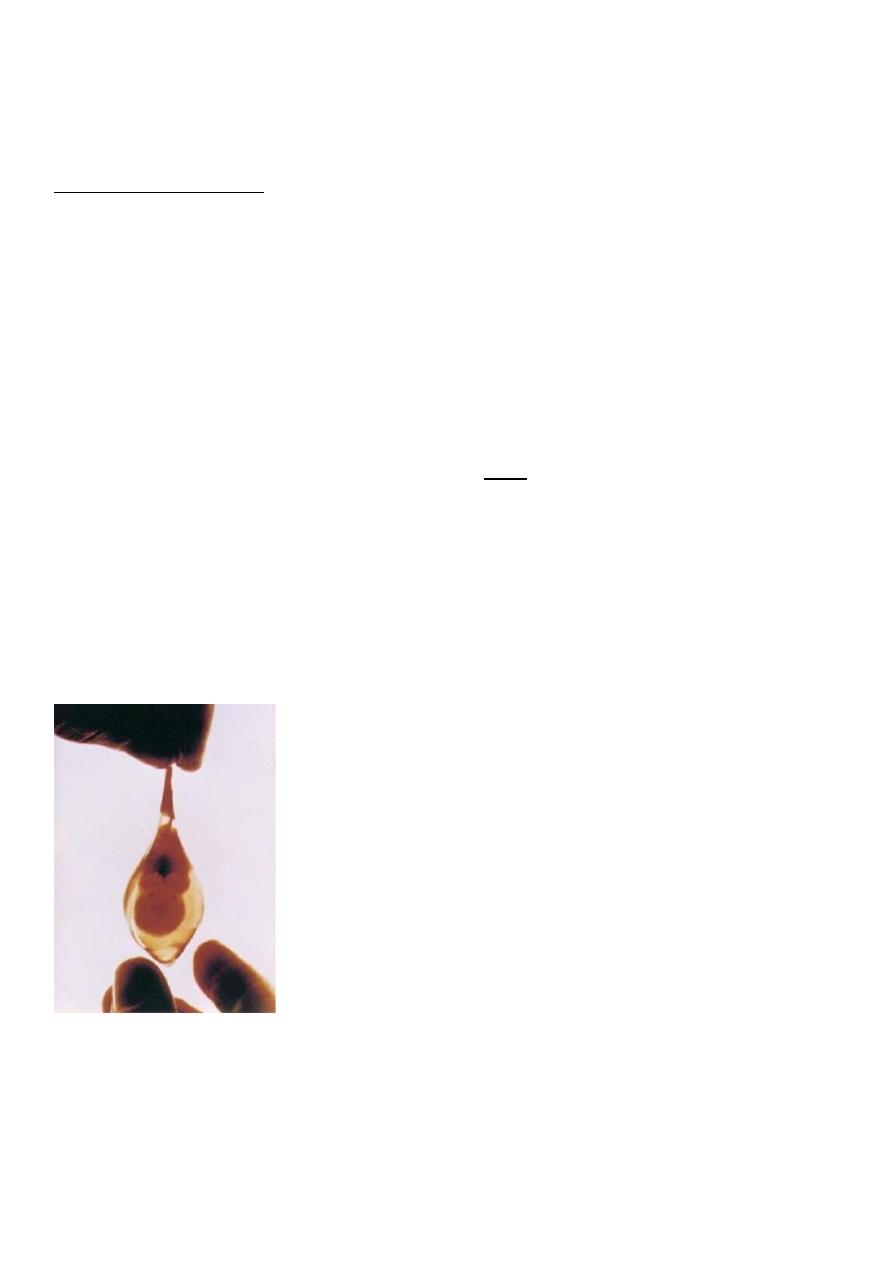
Sign:
1.Uterus may be smaller than expected for period of amenorrhea.
2.Cervix is open.
3.Speculum examination reveals dilated internal os and tissue within the endocervical canal
or vagina.
4.Bleeding may be heavy.
ed cervical os
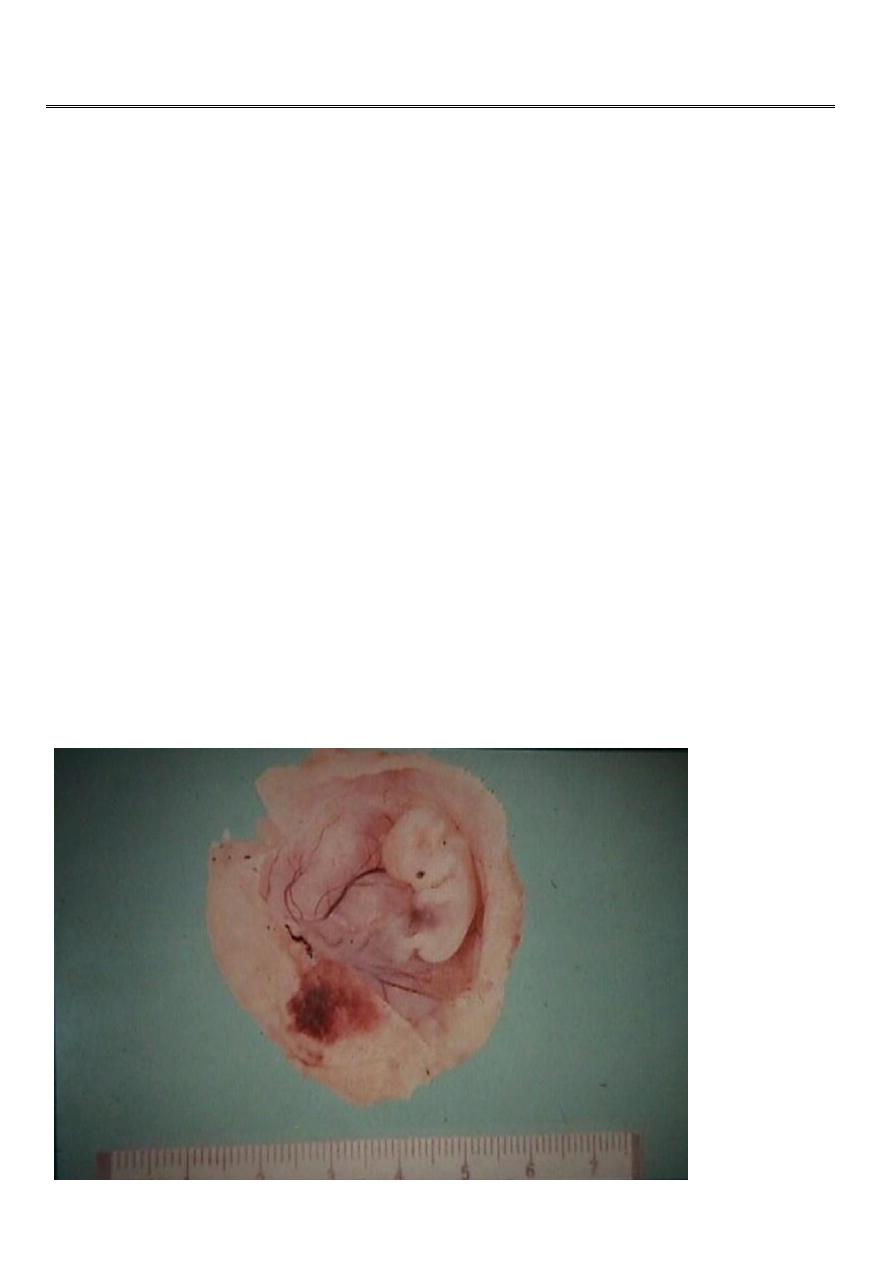
Incomplete abortion with products of conception passing through the dilat
Treatment:
Severe vaginal bleeding
-
A
1- Need admission to hospital and resuscitation with intravenous fluid (IV) fluid and blood
transfusion(if needed) and give analgesia and evacuation of uterus by curettage with out need
of dilatation under oxytoxic drugs.
2-Anti D (250unite) should be given to non sensitized Rh negative women.
3-Digital removing of product of conception which are in cervical canal is advised as this
help to relieve the discomfort.
:
B. Mild vaginal bleeding
1-Ultrasound examination done to confirm presence of retained product of conception which
need surgical evacuation by curettage.
2-Anti D (250unite) should be given to non sensitized Rh negative women.
4- complete abortion :
All product of conception have been expelled and uterus is empty without need for medical
or surgical intervention.
Symptoms:
history of severe abdominal pain
after
Scanty blood loss and cessation of abdominal pain
and severe vaginal bleeding with passing product of conception.
Signs
1.uterus is smaller than period of amenorrhea and firmly contracted.
2. cervix is closed or patulous in multiparous women.
Investigations:
Ultrasound to confirm empty cavity.

-No further treatment is needed but patient warned to report at once if bleeding recur or
develop fever.
Anti D (250unite) should be given to non sensitized Rh negative women.
5-Missed abortion :
fetus dies in uterus and is retained inside uterus.
Symptoms:
1.May be preceded by sign and symptom of threatened abortion.
2.Disappearance of symptoms of pregnancy.
3.Dark brown vaginal discharge.
4.Diagnosed incidentally by ultrasound(sometimes).
Signs:
1.Uterus is smaller than period of amenorrhea (small for date uterus).
2.Cervix is closed.
Investigations:
1-hCG drops in 7-10 days. Positive test dose not exclude missed although negative test
support diagnosis of dead fetus
2-Ultrasound showed: no fetal heart and gestational sac may collapse.
-If there is any doubt about diagnosis, it is wise to wait for a few days and repeat scan to see
if sac is growing.
ray after 16 weeks show collapse of fetal
-
, abdominal x
not available
If ultrasound is
-
skeleton
Complication:
1.infection.
2.coagulation disorder (Disseminated Intravascular Coagulopathy-DIC-). It is rare if less
than one month from death of fetus.
3. psychological distress to mother.
Treatment:
Once diagnosis established, evacuation of uterus without delay after investigation (mainly
for fibrinogen level).
:
First trimester
Suction curettage is preferred.
:
Second trimester
Induction of abortion and uterine activity is stimulated by oxytocin infusion after pre
treatment with mifepristone or vaginal prostaglandin E2 or prostaglandin extra-amniotically
by foly catheter introduced through cervix.
Anti D (250unite) should be given to non sensitized Rh negative women.

5-septic abortion :
Infection of the uterine cavity may occur following any kind of abortion but is more common
following:
-missed abortion.
-incomplete abortion.
-induced abortion (criminal).
Infection will first occur in the uterus but will rapidly spread to the fallopian tubes, pelvic
organs and peritoneum and will cause septicemia if not promptly treated.
The commonest microorganism are Escherichia coli (E coli), streptococcus, staphylococcus
aureus, clostridium Welchii
Symptoms:
1-History of abortion (often criminal).
2-Maternal fever.
3-Lower abdominal pain.
4-Persistent vaginal bleeding.
5-Offensive vaginal discharge.

Signs:
1-patient is ill, toxic.
2-Raise temperature and tachycardia.
3-Suprapubic tenderness with guarding.
4-Uterus is very tender.
5-Cervix remained patulous.
6-Offensive vaginal discharge.
Investigations:
Ultrasound.
Vaginal and cervical swab, blood and urine culture.
Treatment :
1.admission to hospital.
2.antibiotic therapy parentral wide-spectrum antibiotic continuo for at least 5 days after fever
subside.
-If no response, change according to result of culture and sensitivity
-If the product of conception are retained, the uterus should be evacuated by curettage
a.If there is mild bleeding curettage postponed until 24 hours after starting antibiotic therapy
.b. if there is Severe bleedingCurettage under general anesthesia done without delay with
antibiotic and oxytoxic drugs.
Anti D (250unite) should be given to non sensitized Rh negative women.
Complications of septic abortion:
1-bacteramic shock.
2-renal failure.
3-hepatic failure.
4-Disseminated Intravascular Coagulopathy (DIC).
5-more liable for perforation during curettage.
6-gangrenous uterus if clostridia infection.
7-maternal death.
8-long term squeal after treatment (infertility, chronic pelvic infection and pain).

Tissue obtained at the time of miscarriage should be examined histologically to confirm
pregnancy and to exclude ectopic pregnancy or unsuspected gestational trophoblastic
disease.
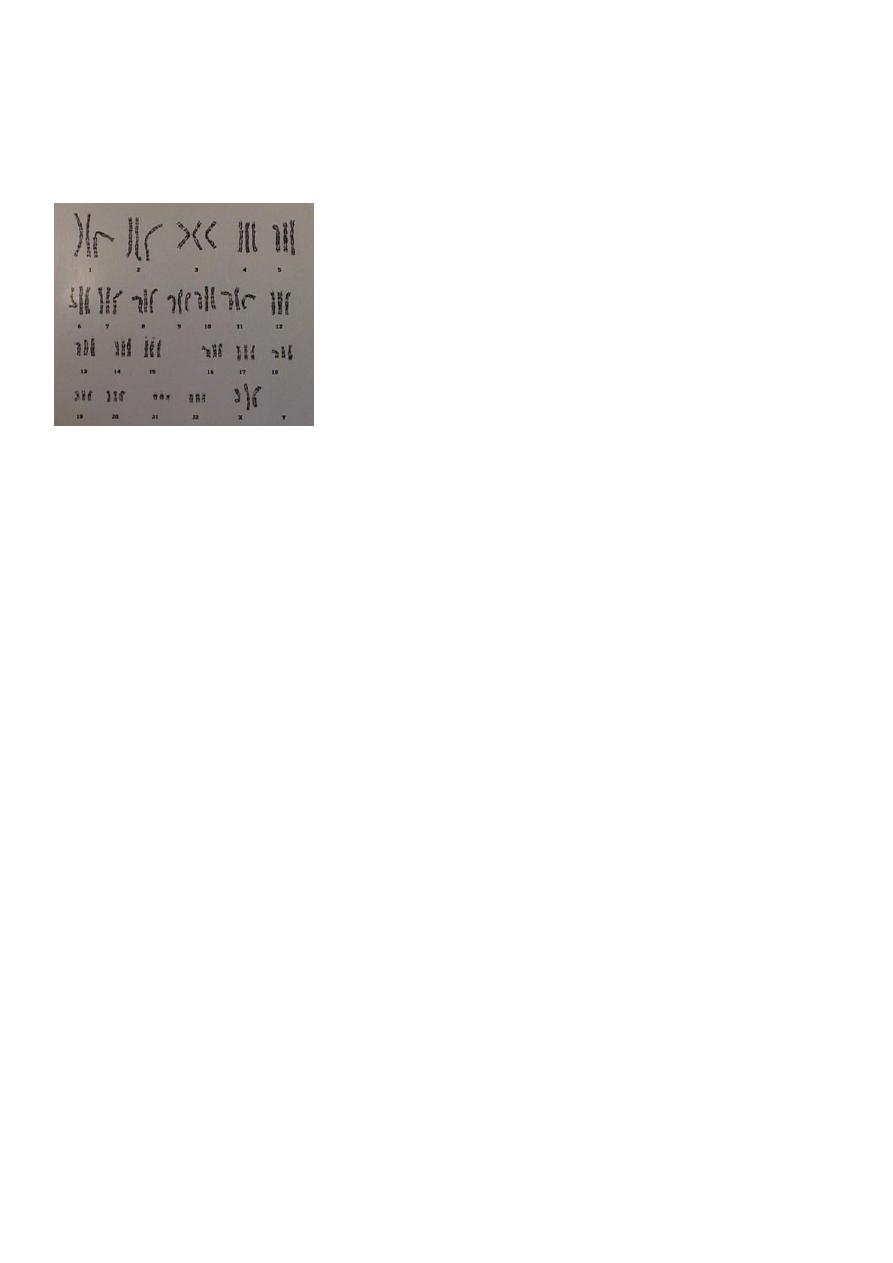
6-Recurrent miscarriage (recurrent abortion)(Habitual abortion):
It is three or more consecutive (successive) spontaneous abortions.
Incidence: 1-2 % of pregnancy.
Risk of further abortion after 3 abortion estimated as 30-70%.
causes:
A. idiopathic (chance phenomena).
B. causes which are:
1.Genetic
Parental chromosome abnormalities (in 3 - 5% of couples with RM).
Fetal aneuploidy ((trisomy or monosomy)).
2.Endocrinopathies
Badly controlled diabetes mellitus (well-controlled diabetes mellitus is not a risk factor for
recurrent miscarriage).
thyroid auto-antibodies are increased among women with RM (treated thyroid
dysfunction is not a risk factor for recurrent miscarriage).
polycystic ovaries (PCO) ???
3.antiphospholipid syndrome(apl)
lupus anticoagulant (LA)and the anticardiolipin antibodies (aCL) have been shownto be of
reproductive significance.
4. thrombophilic defects.
5. Immune dysfunction.
6. Structural uterine abnormalities. (congenital anomalies, submucous and intramural
leiomyomas, polyps, intrauterine adhesions).

Recurrent abortion (Habitual):
Evaluation of wife and husband with recurrent abortion includes:
a. full history (past obstetric history, past gynaecological history, past medical history,
family history, previous investigation and treatment) and history about husband.
b. physical examination.
c. investigations required in recurrent abortion are:
1.Maternal and paternal chromosome analysis (karyotype) and fetal chromosome analysis
to exclude translocations.
2.Thrombophilia screen.
3. Anticardiolipin antibody, lupus anticoagulant.
To diagnose APS it is mandatory that the patient should have two positive tests at least six
weeks apart for either lupus anticoagulant or anticardiolipin (aCL) antibodies of IgG and/or
IgM class present in medium or high titre.
4.Pelvic ultrasound.
5.Hysterosalpingogram/ hysteroscopy (to evaluate uterine cavity).
Mid- follicular serum LH/FSH.
High vaginal swab.
After evaluation , cause can be identified in 50% of cases.
6.Mid- follicular serum LH/FSH.(LH=lutinizing hormone, FSH = follicular stimulating
hormone)
7.High vaginal swab.
A significant proportion of cases of recurrent miscarriage remain unexplained, despite
detailed investigation.
-TORCH (Toxoplasmosis, Other [congenital syphilis and viruses], Rubella, Cytomegalovirus and Herpes simplex virus)
in the investigation of recurrent miscarriage, outside an acute infectious episode .
unhelpful
screening is
Treatment:
1-if the cause can be identified , treat the cause as:
-cervical incompetence – cerclage.
-Uterine abnormalities -Surgical treatment, excision of septum, myomectomy.
-Antiphospholipid Ab can be treated with aspirin and heparin.
-serum immunological factors can be treated by immune therapy under study?.
2-Idiopathic (no identified cause):
These women can be reassured that the prognosis for a successful future pregnancy is good
in subsequent pregnancy. with supportive care alone , the success pregnancy is 75%.
The patient need:
-Supportive care alone.
-Weekly assessment by ultrasound.
-Screen for antiphospholipd Ab
-Screen for bacterial vaginosis.
-Aspirin 75mg/ day peri-coceptional till 36 weeks of gestation.(may be used).
-hCG 10000unit/ week intra muscular.(may be used).
proved.
not
IV immunoglobulin
-
note/Idiopathic recurrent pregnancy loss has successful pregnancy in 67% of pregnancy even
without treatment
7-Induced abortion(termination of pregnancy):
Abortion which occurs as a result of interference which may be medical, surgical or result
from the use of herbal preparations or other traditional practices which cause the uterus to
expel or partly expel its contents.
A-legal induced abortion (therapeutic abortion):
Is the termination of pregnancy before time of viability for purpose of saving mother's life.
as in :
(only)
it is done for medical indication
our locality
In
1-Malignant disease (breast carcinoma, cervical carcinoma).
2-severe cardiac disease.
3-Severe renal problem.
4-Severe Pulmonary disease.
5-Severe gastrointestinal disease.
, it done for fetal abnormalities and for mental health of mother and
other part of world
In
welfare of existing children in family.
B. Illegal induced abortion (criminal abortion):
Strange method are sometimes used as well as instrument not sterile and mostly done by
unskilled person.
It is dangerous because of:
-drug used may cause poisoning.
-infection easily introduced.
-risk of severe hemorrhage.
-embolism may occur.
-perforation of uterus.
Management of miscarriage:-
1-The treatment option should take into account :
2-The patient’s symptoms.
3-type of miscarriage.
4-volume of retained tissue .
5-patient's choice.
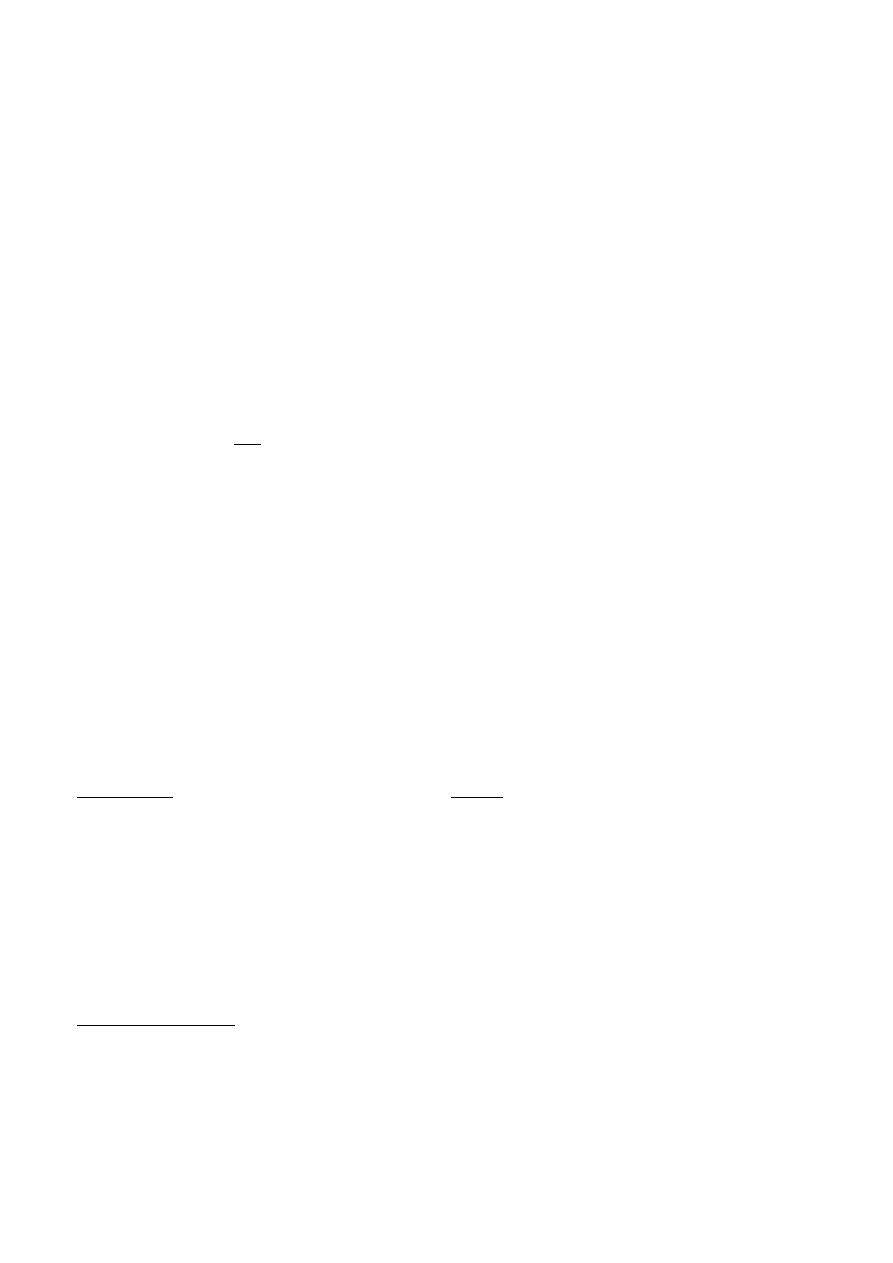
Surgical evacuation:-
Surgical evacuation remains the treatment of choice if:
1-bleeding is excessive.
2-vital signs are unstable.
3-infected tissue is retained.

Surgical evacuation technique determined by duration of pregnancy and skill of obstetricians
and include:
1.Curttage.
2.Suction curettage.
3.Dilatation and curettage (D&C).
4.Dilatation and evacuation.
5.Menstrual aspiration (pregnancy below 6 weeks).
6.Hysterotomy (second trimester rarely).main removal of product of conception after
opening uterus in laprotomy before fetal viability).
7.Hysterectomy (special cases as in cervical carcinoma).(main removal of uterus).
8-Mechanical dilatation (Hegar dilator).
9-Laminaria
10-Prostaglandin pessaries.
11-Laprotomy

In all cases where surgical evacuation by curettage is the treatment option consideration
should be given to the use of a cervical priming agent and method which are:
a.Mechanical dilatation (Hegar dilator).
b.Laminaria
c. Prostaglandin pessaries
MEDICAL MANAGEMENT:-
1-oxytocin infusion intravenously (IV).
2-prostaglandin E2, F2α and PG analogue (second trimester). Route of administration either:
3-vaginal insertion.
4-oral ingestion.
5-Parentral injection.
6-Extra amniotic through folycatheter which pass the cervix.
7-Intra amniotic injection.
8-antiprogestrone (mifepristone Ru 486).
9-intra amniotic hyperosmotic fluid (urea).
10-various combination of the above.
Complications of curettage:
1-Immediate :
-haemorrhage.
-uterine perforation.
-cervical injury.
-acute haematometra.
-intra-abdominal organ injury.
-increase maternal mortality.
2-Delayed:
-infection.
-retained tissue.
3-late:
1.Asherman's syndrome (intrauterine adhesions).
2.Future pregnancy adverse outcome (as cervical incompetence)
3.Rh sensitization if mother Rh negative and not receive prophylactic treatment.
POST-PROCEDURE CARE:
After abortion, patient should know the condition which necessitate immediate medical care
which are:
-prolonged bleeding (more than two weeks).
-prolonged cramping (more than a few days).
-bleeding more than normal menstrual bleeding.
-severe or increased pain.
-fever, chills, or malaise.
-syncope (fainting).
Contraception:
Patient after abortion can get pregnancy even before next menses. All hormonal methods can
be safely initiated immediately following abortion and intrauterine device (IUD) can be
safely inserted.
FinallyDone -_-
